Patient-specific three-dimensional (3D) printed models have been increasingly used in cardiology and cardiac surgery, in particular, showing great value in the domain of congenital heart disease (CHD). CHD is characterized by complex cardiac anomalies with disease variations between individuals; thus, it is difficult to obtain comprehensive spatial conceptualization of the cardiac structures based on the current imaging visualizations. 3D printed models derived from patient’s cardiac imaging data overcome this limitation by creating personalized 3D heart models, which not only improve spatial visualization, but also assist preoperative planning and simulation of cardiac procedures, serve as a useful tool in medical education and training, and improve doctor–patient communication.
1. Introduction
Computed tomography (CT), magnetic resonance imaging (MRI), and echocardiography represent commonly used imaging modalities in the diagnostic assessment of congenital heart disease (CHD). These imaging techniques allow for generation of two-dimensional (2D) and three-dimensional (3D) visualizations, which play an important role in understanding the complexity of CHD and assisting pre-procedural planning of cardiac procedures. Despite useful information provided by these imaging modalities, the images are still limited to be viewed on 2D screens which is very different from the physical models that offer realistic visualization of 3D spatial relationship between normal and anomalous anatomy. 3D printing overcomes this limitation by creating patient-specific or personalized medical models [
1,
2,
3]. The tactile experience offered by 3D printed models is another advantage over traditional image visualizations as the physical models enable comprehensive evaluation of anatomical and pathological structures which cannot be obtained by other methods [
4].
3D printing has been increasingly utilized in the medical field with studies confirming its clinical value and usefulness in many areas, ranging from medical education to pre-surgical planning and simulation of complex surgeries, and to patient–doctor communication [
5,
6,
7,
8,
9,
10]. In particular, personalized 3D printed models have been shown to offer valuable information for treating patients with CHD due to complexity and anatomic variation associated with this disease. Most of the current reports on 3D printing in CHD are dominated by isolated case reports or case series, with only a few single or multi-center studies and randomized controlled trials (RCT) available in the literature.
2. Image Post-Processing and Segmentation Process for Three-Dimensional (3D) Printing in Congenital Heart Disease (CHD)
The first step to generate a 3D printed heart model is to undergo a series of image post-processing and segmentation of volumetric data, which are commonly acquired with cardiac CT or MRI imaging. While high-resolution original datasets are important for accurately isolating the desired anatomy of interest and pathology from surrounding structures, segmentation of cardiac structures remains challenging due to complexity of cardiac features, especially in the CHD cases. Different software is used for segmentation, with Mimics (Materialise HQ, Leuven, Belgium) being the most commonly used commercial software and 3D Slicer (Brigham and Women’s Hospital, Boston, Mass) as the most common open-source tool. Several review articles have provided excellent description of details about the steps required from data acquisition to image post-processing and segmentation [
11,
12,
13,
14].
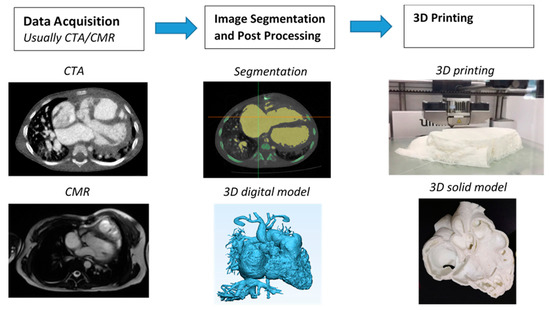
Figure 1 shows the steps to create 3D printed models from data acquisition to image post-processing and segmentation.
Figure 1. Steps involved in fabrication of 3D printed heart models. CTA—computed tomography angiography; CMR—cardiac magnetic resonance; 3D—three-dimensional.
3. Accuracy of 3D Printed Heart Models
The most important part of creating 3D printed models is to ensure that 3D models accurately delineate anatomical structures and pathologies since the model accuracy is essential for treatment planning [
15]. Current research evidence indicates that 3D printed heart models are generally accurate [
16], and this has been validated by other studies, either based on case reports/series or single- or multi-center studies [
17,
18,
19,
20,
21,
22,
23]. In most of the studies, model accuracy is determined by the degree of agreement between the measured dimensions of the 3D printed model and the dimensions of original source images, usually using cardiac CT, MRI, and sometimes using rotational angiography or echocardiography [
16,
17,
18,
22], or intraoperative findings [
19]. Currently, there is no standardized method to measure the dimensions of the 3D printed heart models. Most of the studies carried out measurement using calipers on the physical 3D printed models [
17,
20,
21]. Only a few studies conducted measurement on the standard tessellation language (STL) file [
18] and conducted CT scan on the 3D printed model for measurement [
16]. The authors claimed it is easier to replicate the exact plane for measurement comparison, hence improving the accuracy of the results [
16,
18].
4. 3D Printed Models in Medical Education and Training
3D printed heart models have been shown to serve as a novel teaching tool in medical education and training and this is confirmed by RCT available in the literature [
22,
23,
24,
25]. Three of them reported the usefulness of 3D printed models of different types of CHD in medical education [
22,
23,
24].
Table 1 shows details of these three studies and other single- and multi-center reports.
Table 1. Study characteristics of randomized controlled trials and multi- and single-center studies.
| Authors |
Study Design |
Sample Size and Participants |
Types of CHD |
Key Findings |
| Loke et al. 2017 [22] |
RCT: study group was presented with 3D printed models, while control group with 2D images |
35 pediatric residents:18 in study group and 17 in control group |
Tetralogy of Fallot (ToF) |
3D printed models resulted in significantly higher satisfaction scores than 2D images (p = 0.03). 3D printed models improved residents’ self-efficacy scores in managing ToF, although this did not reach significant difference when compared to 2D images (p = 0.39). |
| Su et al., 2018 [23] |
RCT: study group participated in teaching seminar including 3D printed models, while control group only attended teaching seminar without having 3D models |
63 medical students: 32 in study group and 31 in control group |
Ventricular septal defect (VSD) |
Significant improvement in VSD learning and structure conceptualization in the study group compared to the control group (p < 0.05). |
| White et al., 2018 [24] |
RCT: study group was given 3D printed models in addition to lectures, while control group received only the lectures |
60 pediatric residents:31 in study group and 29 in control group |
VSD and ToF |
3D printed models of CHD improved residents’ knowledge and confidence in managing complex CHD such as ToF but did not seem to improve simple CHD such as VSD. |
| Olivieri et al., 2016 [26] |
Single-center report of 3D printed models for training and simulation |
10 3D printed models, 70 clinicians participated in the training sessions |
Cardiac and vascular anomalies |
3D printed models can be used as a simulation training tool for multidisciplinary intensive care providers by enhancing their anatomic knowledge and clinical management of CHD patients. |
| Hoashi et al., 2018 [27] |
Single-center experience |
20 cases |
DORV and other cardiac anomalies |
3D printed heart models improved understanding of the relationship between intraventricular communications and great vessels. Further, 3D printed models allowed simulation of cardiac surgeries by creating intracardiac pathways, thus providing benefits to inexperienced cardiac surgeons. |
| Valverde et al., 2017 [21] |
Multi-center study consisting of 10 international centers |
40 patients with complex CHD |
DORV (50%) and other cardiac anomalies |
3D models were accurate in replicating anatomy. 3D models refined the surgical approach in nearly 50% cases. 3D models resulted in significant change in the surgical plan in 24% of cases. |
| Zhao et al., 2018 [28] |
Single-center experience |
25 patients with 8 in 3D printing group and 17 in control group |
DORV |
3D printed models showed high accuracy in measurements of aortic diameters and the size of VSD when compared to original CT data. 3D printed models significantly reduced ICU time and mechanical ventilation time (p < 0.05). |
| Ryan et al., 2018 [29] |
Single-center experience |
Of 928 cardiothoracic surgeries, 164 3D models were printed for various purposes |
DORV, ToF and other cardiac anomalies |
3D printed models reduced mean time in the operating room and 30-day readmission and mortality rates when compared to the standard of care. |
5. 3D Printed Models in Pre-Surgical Planning and Simulation
Due to complexity of the cardiac conditions with wide variations between individuals with CHD, 3D printed models demonstrate great advantages over traditional image visualizations in pre-surgical planning and simulation of cardiac surgeries. A recent systematic review has summarized findings from a number of case reports and series with regard to the use of 3D printed models in facilitating preoperative planning and surgical decision-making in CHD cases [
33].
Table 1 shows some results from single- and multi-center studies which involved more than 20 cases or participants about the value of 3D printed heart models in this aspect [
20,
26,
27,
28,
29]. These studies reported the usefulness of 3D printed heart models from different perspectives. Among all types of CHD, double outlet right ventricle (DORV) and ToF represent the most common types of CHD for fabrication of 3D printed models. This is reported in four out of the five studies mentioned above [
21,
27,
28,
29].
Olivieri et al. created 3D printed models from 10 patients who underwent congenital cardiac surgery due to various cardiac and vascular anomalies [
26]. They presented the 3D models to 70 clinicians including 22 physicians, 38 critical care nurses, and 10 ancillary providers. At completion of the cardiac surgeries, all participants underwent a training session of simulating intra- and post-operative care using 3D printed heart models. The use of 3D printed models was found to be more effective than standard verbal hand off with average score of 8.4 out of 10. In total, 90% of participants scored it very highly with regard to the efficacy of 3D printed models in improving cardiac anatomy understanding, surgical understanding, and ability to manage CHD clinically.
Two other studies reported utilizing 3D printed heart models in the diagnostic management of patients with CHD [
21,
27]. Hoashi et al. created 20 3D printed heart models for the purpose of preoperative simulations of cardiac surgeries [
27]. Despite realistic and expensive models being produced (each model costs between $2000 and $3000), this study mainly focused on findings related to patient’s cardiac surgery outcomes, while the value of 3D printed models was briefly mentioned in some sample cases. Specifically, authors concluded that 3D printed heart models did not reduce cardiopulmonary bypass time. In contrast, Valverde et al. conducted a multi-center study and performed both quantitative and qualitative assessments of the role of 3D printed models in clinical decision-making in patients with complex CHD [
21]. Forty patients recruited from 10 international centers were included in this prospective study with 3D models fabricated using CT or MRI images. 3D printed models were assessed as to whether they changed the surgical decision (from conservative management to surgical intervention) and whether the surgical plan was modified. In more than half of the cases (52.5%), 3D printed models did not result in any change to the surgical decision. However, 3D printed models showed significant clinical impact on redefining the surgical approach in 47.5% cases. In 25% of cases, after inspection of 3D printed models, the surgical plan was modified with conservative management changed to surgery. As the only multi-center study available in the literature, this study shows the impact of 3D printed models on deciding the best surgical approach. However, more similar studies are desirable to validate this.
The other two studies are based on single-center experience reporting the clinical impact of 3D printed models in CHD treatment outcomes [
28,
29]. Zhao et al. divided 25 patients with complex DORV into two groups, 8 in the 3D printing group and 17 in the control group, with all patients undergoing cardiac surgery [
28]. The intensive care unit stay time and mechanical ventilation time in the 3D printing group was significantly shorter than in the control group (
p < 0.05). Although the operative duration, cardiopulmonary bypass time, and aortic cross-clamping time in the 3D printing group was shorter than the control group, this did not reach statistical significance (
p > 0.05). Similar findings are reported by Ryan and colleagues [
29]. The authors presented their single-site three-year experience of using 3D printed models for managing CHD cases. Of 164 models fabricated for different purposes, 79 models covering a range of CHD complexities were selected for surgical planning. When compared to the standard care (without anatomical models) group, the 3D printed heart model group was found to have shorter mean duration in the operative room and lower 30-day readmission and mortality rates. However, it is worthwhile to note that it did not reach statistical significance, and it is likely due to limited study sizes for each CHD types. These reductions in durations could contribute to lower morbidity and mortality associated with management of CHD, although this needs to be validated by further studies. One example would be by investigating the impact of 3D printed models on 30-day post-operative outcome.
6. 3D Printed Models in Doctor–Patient Communication
Physician–patient relationship and working alliance plays a crucial role in improving patient adherence, level of satisfaction, and treatment outcomes [
34]. Due to complexity and variations of cardiac anatomy in CHD, it is especially challenging in achieving good physician–patient communication (physicians specifically refer to cardiologists and cardiac surgeons in the situation of managing patients with CHD) [
35]. Traditional approaches of using diagrams or image visualizations for explanation of complicated cardiac pathologies do not allow doctors to effectively communicate to patients or parents because of difficulty in interpreting 3D conceptualization of spatial relationship between cardiac structures. 3D printed models are able to eliminate this limitation as observers have no restriction in appreciating the spatial relationship between cardiac structures in all dimensions, thus improving doctor–patient communication.
A study by Biglino et al. first attempted to quantify the benefit of 3D printed models in doctor–patient communication [
36]. Ninety-two parents of patients with CHD were randomly allocated to two groups with 45 assigned to the model group using 3D printed heart models during their visit, and 52 to the control group with no models during consultation. Parents were asked to complete two questionnaires: A first brief questionnaire before their child’s consultation and a second brief questionnaire after the consultation with regard to understanding of their child’s heart condition, identification of cardiac defects, and clarity of planned intervention or procedure. Both cardiologists and parents rated the 3D printed models as very useful. Despite the improvement in doctor–parent communication, 3D printed models did not lead to improving parents’ knowledge and understanding of their child’s heart condition. Furthermore, consultations using the 3D printed models were found to be longer than those without the models (21 ± 10 vs. 16 ± 7 min,
p = 0.02), although this did not show significant impact on overall duration of the visits.
This entry is adapted from the peer-reviewed paper 10.3390/jcm8040522