The load integrals (impulse) over the central metatarsal region significantly increased, indicating that surgeries increased the risk of transfer metatarsalgia. There is no solid evidence that hallux valgus (HV) surgeries could improve forefoot functions from a biomechanical point perspective. Surgeries might reduce the plantar load over the hallux and adversely affect push-off function.
- bunion
- hallux abducto valgus
- metatarsus primus varus
- pedobarography
1. Introduction
2. Forefoot Function after Hallux Valgus Surgery
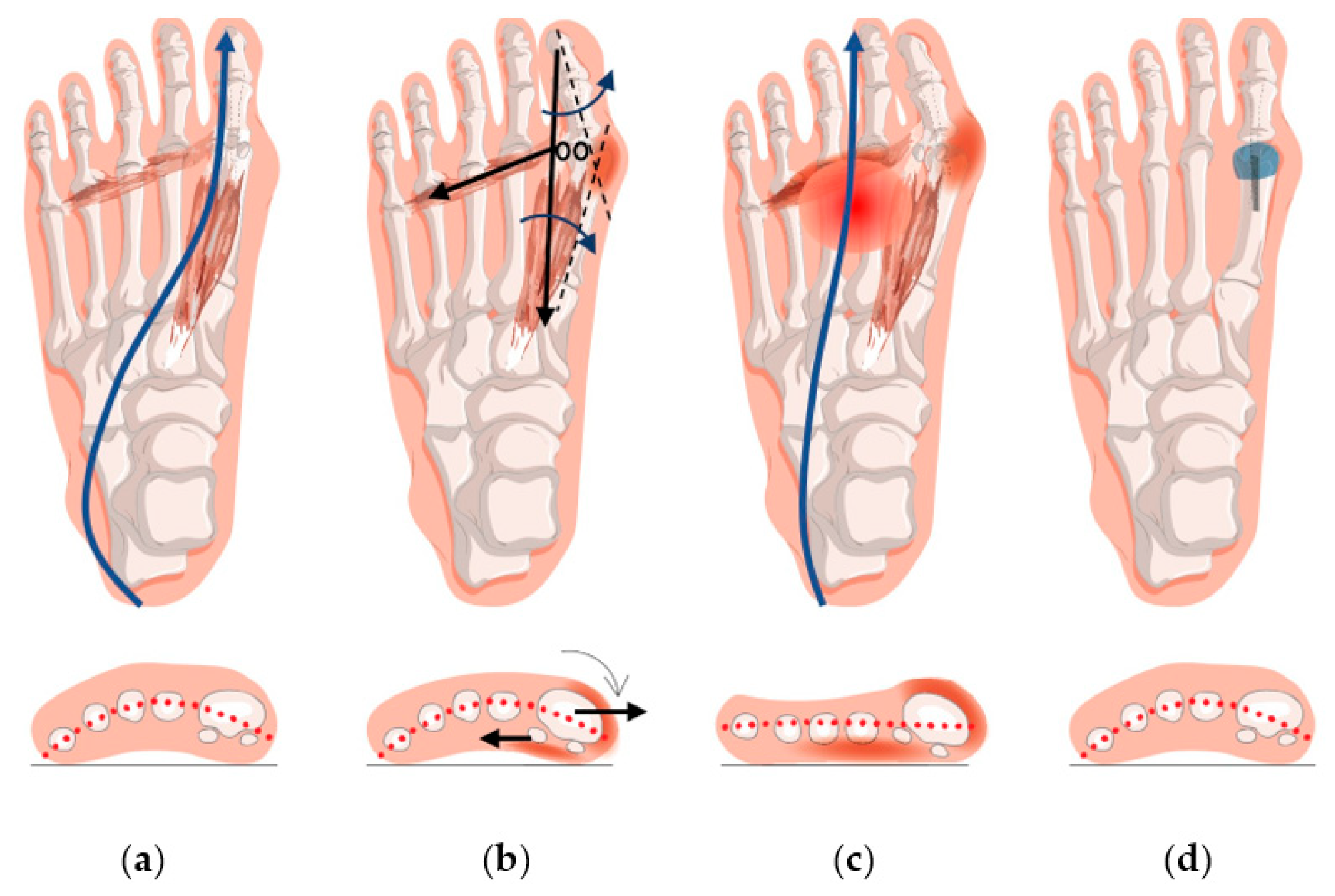
A meta-analysis showed that there was a reduction in hallux and medial forefoot load/impulse that implicated the failure of surgeries to restore forefoot functions [25]. Besides, the pain-causing load at the central forefoot was not lessened. The pathomechanics that manifested transfer metatarsalgia was thus not resolved.
Although substantial heterogeneity was observed in the meta-analysis [25], most of the individual studies did not favor surgeries, and some did admit that surgical interventions failed to restore normative plantar functions or produced no significant biomechanical improvement [26][27][28][29][30][31]. One possible explanation for the finding is that some of the included studies were old, and the surgical technique or plantar pressure instrument might have been flawed at that time. Nevertheless, subgroup analyses by year of publication indicated that this lack of effectiveness was unlikely due to whether the surgical methods were old or relatively new. Another reason for the failure could be premature ambulation with pain, stiffness, and weakened intrinsic muscles [28][31]. Indeed, a significantly worse load distribution on the hallux and central metatarsal region was observed in the studies with a shorter follow-up period (<12 months). A third reason could be related to the elevation of first metatarsal head in the surgical procedure in some studies, which might produce negative impact on the plantar pressure. Elevated or a more dorsal position of the first metatarsal head might reduce the load-carrying capacity of the first ray, which was recognized as the cause of metatarsalgia and poor surgical outcomes [32]. Some osteotomy techniques, such as Crescentic [26], closing wedge [33], and Weil [34] are vulnerable to the elevation of the first metatarsal. Nevertheless, the analysis did not support this fact as the source of heterogeneity. A fourth reason is that the surgeries may not correct or ameliorate hypermobility or instability of the forefoot, which is the etiology of HV [35]. Besides, mainstream surgical techniques may fail to repair the stabilizing soft tissue structures and the underlying soft tissue deficiency or imbalance, which adversely affect the load-carrying capacity [36].
The “negative” biomechanical effects of HV surgeries demonstrated seem to contradict the positive clinical improvement after surgeries. It hypothesizes that immediate pain relief and restoration of daily functions might not necessarily complement the resumption of normal foot kinematics and walking capability, which is a secondary measure to contemplate potential deformity recurrence, complications, compensatory foot problems, and falling risks. Surgeries treat the bone misalignment of HV but might not be treating the root cause of the problem.
In fact, HV surgeries could remedy bunion (swollen joint) problems, shoe-fitting issues, and facilitate immediate pain relief. Moreover, the restoration of bone alignment ameliorates push-off functions by correcting the position of the sesamoid bones and muscle directions. Radiographic assessment and patient-reported outcomes are undoubtedly the primary outcomes, reflecting deformity correction and immediate pain relief. Yet, these evaluation measures are insufficient, and perceived pain relief may not necessarily be associated with restoration of biomechanical functions [37]. Plantar load measurements examine whether the corrected foot could resume normal foot kinematics and walking capability and could serve as a secondary measure to contemplate potential deformity recurrence, complications, compensatory foot problems, and falling risks. Thus, it would be desirable to have surgeries that are effective in improving plantar load distribution. Some surgeons endeavor to develop alternative surgical methods, including metatarsal suturing techniques (e.g., mini-tightrope) that could reinforce the site stability and minimize the risk of traumatizing osseous procedures [38]. However, the effectiveness of these methods warrants further investigation.
Postoperative rehabilitation, such as orthosis and muscle training, plays an important role in load redistribution and regaining foot functions. Postoperative muscle retraining could strengthen hallux functions, restore joint mobility and thus physiological gait patterns [39][40]. Schuh et al. [39] commented that the strengthening of peroneus longus muscle can facilitate a better midfoot pronation control and therefore direct load to the first ray correctly. Foot orthosis with arch support could also help control pronation [41], while a metatarsal pad could relieve pain and maintain the integrity of the transverse arch, in cases of first ray insufficiency [42][43][44]. Besides, despite that an increase (or a restoration) of first ray load indicated the restoration of biomechanical functions, it should be noted that unloading the first ray by immobilization or partial weight bearing in the early postoperative stage is essential to facilitate pain management and mitigate risks of non-union [45][46][47].
Besides the variations of surgical techniques, the intrinsic features of HV, such as spring ligament insufficiency [48], first ray hypermobility [49], hypermobility due to malpractice in amateur ballet dancers [50], generalized ligament laxity [51], medial column instability, and posterior tibial tendon dysfunction [52], may have contributed to clinical heterogeneity as well. Moreover, HV was often compounded with other foot problems that were infeasible to isolate [35][53], such as flatfoot [54], plantar fasciitis [55], transfer metatarsalgia [18], and claw toes [56]. There is limited research on the impact of plantar pressure under such circumstances. Those additional foot problems may contribute to variations in plantar loading pattern or postoperative compensatory gait [18][57]. For example, individuals with flat feet might not have sufficient load under the medial forefoot during push-off [58], while those with valgus hindfoot deformities might have higher medial forefoot pressures [59].
3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/jcm12041384
References
- Nix, S.; Smith, M.; Vicenzino, B. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. J. Foot Ankle Res. 2010, 3, 21.
- Nakagawa, R.; Yamaguchi, S.; Kimura, S.; Sadamasu, A.; Yamamoto, Y.; Muramatsu, Y.; Sato, Y.; Akagi, R.; Sasho, T.; Ohtori, S. Efficacy of foot orthoses as nonoperative treatment for hallux valgus: A 2-year follow-up study. J. Orthop. Sci. 2019, 24, 526–531.
- Menz, H.B.; Morris, M.E. Footwear characteristics and foot problems in older people. Gerontology 2005, 51, 346–351.
- Simonsen, E.B.; Svendsen, M.B.; Nørreslet, A.; Baldvinsson, H.K.; Heilskov-Hansen, T.; Larsen, P.K.; Alkjær, T.; Henriksen, M. Walking on high heels changes muscle activity and the dynamics of human walking significantly. J. Appl. Biomech. 2012, 28, 20–28.
- Roddy, E. Epidemiology and impact of hallux valgus: More than just bunions. J. Foot Ankle Res. 2011, 4, 1.
- Roan, L.-Y.; Tanaka, Y.; Taniguchi, A.; Tomiwa, K.; Kumai, T.; Cheng, Y.-M. Why do lesser toes deviate laterally in hallux valgus? A radiographic study. Foot Ankle Int. 2015, 36, 664–672.
- Coughlin, M.J.; Anderson, R.B. Hallux Valgus. In Mann’s Surgery of the Foot and Ankle; Coughlin, M.J., Saltzman, C.L., Anderson, R.B., Eds.; Elsevier: Philadelphia, PA, USA, 2014; Volume 1, pp. 168–321.
- Partio, N.; Mäenpää, H.; Huttunen, T.; Haapasalo, H.; Laine, H.-J.; Mattila, V.M. Incidence of hallux valgus primary surgical treatment. Finnish nationwide data from 1997 to 2014. Foot Ankle Surg. 2019, 25, 761–765.
- Miranda, M.A.M.; Martins, C.; Cortegana, I.M.; Campos, G.; Pérez, M.F.M.; Oliva, X.M. Complications on percutaneous hallux valgus surgery: A systematic review. J. Foot Ankle Surg. 2021, 60, 548–554.
- Malagelada, F.; Sahirad, C.; Dalmau-Pastor, M.; Vega, J.; Bhumbra, R.; Manzanares-Céspedes, M.C.; Laffenêtre, O. Minimally invasive surgery for hallux valgus: A systematic review of current surgical techniques. Int. Orthop. 2019, 43, 625–637.
- Trnka, H.-J. Percutaneous, MIS and open hallux valgus surgery. EFORT Open Rev. 2021, 6, 432–438.
- Lee, K.T.; Park, Y.U.; Jegal, H.; Lee, T.H. Deceptions in hallux valgus: What to look for to limit failures. Foot Ankle Clin. 2014, 19, 361–370.
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353.
- Guyton, G.P. Theoretical limitations of the AOFAS scoring systems: An analysis using Monte Carlo modeling. Foot Ankle Int. 2001, 22, 779–787.
- Mayich, D.J. Life without the AOFAS score: A critical problem in a time of scarcity. Foot Ankle Int. 2012, 33, 689–691.
- Raikin, S.M.; Miller, A.G.; Daniel, J. Recurrence of hallux valgus: A review. Foot Ankle Clin. 2014, 19, 259–274.
- Menz, H.B.; Lord, S.R. Gait instability in older people with hallux valgus. Foot Ankle Int. 2005, 26, 483–489.
- Geng, X.; Huang, D.; Wang, X.; Zhang, C.; Huang, J.; Ma, X.; Chen, L.; Wang, C.; Yang, J.; Wang, H. Loading pattern of postoperative hallux valgus feet with and without transfer metatarsalgia: A case control study. J. Orthop. Surg. Res. 2017, 12, 120.
- Abdul Razak, A.H.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot plantar pressure measurement system: A review. Sensors 2012, 12, 9884–9912.
- Deepashini, H.; Omar, B.; Paungmali, A.; Amaramalar, N.; Ohnmar, H.; Leonard, J. An insight into the plantar pressure distribution of the foot in clinical practice: Narrative review. Pol. Ann. Med. 2014, 21, 51–56.
- Wafai, L.; Zayegh, A.; Woulfe, J.; Aziz, S.M.; Begg, R. Identification of foot pathologies based on plantar pressure asymmetry. Sensors 2015, 15, 20392–20408.
- Hofmann, U.K.; Götze, M.; Wiesenreiter, K.; Müller, O.; Wünschel, M.; Mittag, F. Transfer of plantar pressure from the medial to the central forefoot in patients with hallux valgus. BMC Musculoskelet. Disord. 2019, 20, 149.
- Galica, A.M.; Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Casey, V.A.; Hannan, M.T. Hallux valgus and plantar pressure loading: The Framingham foot study. J. Foot Ankle Res. 2013, 6, 42.
- Yu, J.; Cheung, J.T.-M.; Wong, D.W.-C.; Cong, Y.; Zhang, M. Biomechanical simulation of high-heeled shoe donning and walking. J. Biomech. 2013, 46, 2067–2074.
- Wong, D.W.-C.; Cheung, J.C.-W.; Zhao, J.-G.; Ni, M.; Yang, Z.-Y. Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. J. Clin. Med. 2023, 12, 1384. https://doi.org/10.3390/jcm12041384
- Brodsky, J.W.; Beischer, A.D.; Robinson, A.H.; Westra, S.; Negrine, J.P.; Shabat, S. Surgery for hallux valgus with proximal crescentic osteotomy causes variable postoperative pressure patterns. Clin. Orthop. Relat. Res. 2006, 443, 280–286.
- Cancilleri, F.; Marinozzi, A.; Martinelli, N.; Ippolito, M.; Spiezia, F.; Ronconi, P.; Denaro, V. Comparison of plantar pressure, clinical, and radiographic changes of the forefoot after biplanar Austin osteotomy and triplanar Boc osteotomy in patients with mild hallux valgus. Foot Ankle Int. 2008, 29, 817–824.
- Costa, J.M.; Avila, A.O.V.; Kleinowski, D.N.; Kroth, L.M.; Contreras, M.E.K. Modified Chevron Osteotomy: Preliminary Analysis of Baropodometric Behavior. Acta Ortop. Bras. 2010, 18, 191–196.
- Kernozek, T.W.; Sterriker, S.A. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: Comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002, 23, 503–508.
- Klemola, T.; Leppilahti, J.; Laine, V.; Pentikainen, I.; Ojala, R.; Ohtonen, P.; Savola, O. Effect of First Tarsometatarsal Joint Derotational Arthrodesis on First Ray Dynamic Stability Compared to Distal Chevron Osteotomy. Foot Ankle Int. 2017, 38, 847–854.
- King, C.M.; Hamilton, G.A.; Ford, L.A. Effects of the lapidus arthrodesis and chevron bunionectomy on plantar forefoot pressures. J. Foot Ankle Surg. 2014, 53, 415–419.
- Seki, H.; Oki, S.; Suda, Y.; Takeshima, K.; Kokubo, T.; Nagura, T.; Ishii, K. Three-dimensional analysis of the first metatarsal bone in minimally invasive distal linear metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2020, 41, 84–93.
- Zembsch, A.; Trnka, H.-J.; Ritschl, P. Correction of hallux valgus: Metatarsal osteotomy versus excision arthroplasty. Clin. Orthop. Relat. Res. 2000, 376, 183–194.
- Huerta, J.P.; Lorente, C.A.; Carmona, F.J.G. The Weil osteotomy: A comprehensive review. Rev. Española Podol. 2017, 28, e38–e51.
- Perera, A.; Mason, L.; Stephens, M. The pathogenesis of hallux valgus. JBJS 2011, 93, 1650–1661.
- Wu, D.Y.; Lam, K. Osteodesis for hallux valgus correction: Is it effective? Clin. Orthop. Relat. Res. 2015, 473, 328–336.
- Saro, C.; Andrén, B.; Felländer-Tsai, L.; Lindgren, U.; Arndt, A. Plantar pressure distribution and pain after distal osteotomy for hallux valgus. A prospective study of 22 patients with 12-month follow-up. Foot 2007, 17, 84–93.
- Ponnapula, P.; Wittock, R. Application of an interosseous suture and button device for hallux valgus correction: A review of outcomes in a small series. J. Foot Ankle Surg. 2010, 49, 159.e121–159.e126.
- Schuh, R.; Hofstaetter, S.G.; Adams, S.B., Jr.; Pichler, F.; Kristen, K.H.; Trnka, H.J. Rehabilitation after hallux valgus surgery: Importance of physical therapy to restore weight bearing of the first ray during the stance phase. Phys. Ther. 2009, 89, 934–945.
- Polastri, M. Postoperative rehabilitation after hallux valgus surgery: A literature review. Foot Ankle Online J. 2011, 4, 4.
- Glasoe, W.M.; Nuckley, D.J.; Ludewig, P.M. Hallux valgus and the first metatarsal arch segment: A theoretical biomechanical perspective. Phys. Ther. 2010, 90, 110–120.
- Charen, D.A.; Markowitz, J.S.; Cheung, Z.B.; Matijakovich, D.J.; Chan, J.J.; Vulcano, E. Overview of metatarsalgia. Orthopedics 2019, 42, e138–e143.
- Zeidan, H.; Ryo, E.; Suzuki, Y.; Iijima, H.; Kajiwara, Y.; Harada, K.; Nakai, K.; Shimoura, K.; Fujimoto, K.; Takahashi, M. Detailed analysis of the transverse arch of hallux valgus feet with and without pain using weightbearing ultrasound imaging and precise force sensors. PLoS ONE 2020, 15, e0226914.
- Kang, J.-H.; Chen, M.-D.; Chen, S.-C.; Hsi, W.-L. Correlations between subjective treatment responses and plantar pressure parameters of metatarsal pad treatment in metatarsalgia patients: A prospective study. BMC Musculoskelet. Disord. 2006, 7, 95.
- Moerenhout, K.; Chopra, S.; Crevoisier, X. Outcome of the modified Lapidus procedure for hallux valgus deformity during the first year following surgery: A prospective clinical and gait analysis study. Clin. Biomech. 2019, 61, 205–210.
- Togei, K.; Shima, H.; Yasuda, T.; Tsujinaka, S.; Nakamura, G.; Neo, M. Plantar pressure distribution in hallux valgus feet after a first metatarsal proximal crescentic osteotomy with a lesser metatarsal proximal shortening osteotomy. Foot Ankle Surg. 2021, 27, 665–672.
- Wong, D.W.-C.; Wang, Y.; Zhang, M.; Leung, A.K.-L. Functional restoration and risk of non-union of the first metatarsocuneiform arthrodesis for hallux valgus: A finite element approach. J. Biomech. 2015, 48, 3142–3148.
- Pasapula, C.; Al-Sukaini, A.; Band, H.; Fawi, H.; Cutts, S. Spring Ligament Insufficiency and Hallux Valgus as an independent risk factors for First Ray Instability. Foot 2021, 48, 101818.
- Wong, D.W.-C.; Zhang, M.; Yu, J.; Leung, A.K.-L. Biomechanics of first ray hypermobility: An investigation on joint force during walking using finite element analysis. Med. Eng. Phys. 2014, 36, 1388–1393.
- Biz, C.; Favero, L.; Stecco, C.; Aldegheri, R. Hypermobility of the first ray in ballet dancer. Muscles Ligaments Tendons J. 2012, 2, 282.
- Wong, D.W.-C.; Wang, Y.; Chen, T.L.-W.; Yan, F.; Peng, Y.; Tan, Q.; Ni, M.; Leung, A.K.-L.; Zhang, M. Finite element analysis of generalized ligament laxity on the deterioration of Hallux valgus deformity (bunion). Front. Bioeng. Biotechnol. 2020, 8, 1062.
- Blackwood, S.; Gossett, L. Hallux valgus/medial column instability and their relationship with posterior tibial tendon dysfunction. Foot Ankle Clin. 2018, 23, 297–313.
- Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Menz, H.B.; Casey, V.A.; Hannan, M.T. Foot disorders, foot posture, and foot function: The Framingham foot study. PLoS ONE 2013, 8, e74364.
- Heyes, G.J.; Vosoughi, A.R.; Weigelt, L.; Mason, L.; Molloy, A. Pes planus deformity and its association with hallux valgus recurrence following scarf osteotomy. Foot Ankle Int. 2020, 41, 1212–1218.
- Cobden, A.; Camurcu, Y.; Sofu, H.; Ucpunar, H.; Duman, S.; Kocabiyik, A. Evaluation of the Association Between Plantar Fasciitis and Hallux Valgus. J. Am. Podiatr. Med. Assoc. 2020, 110.
- Wu, W.-L.; Liang, J.-M.; Cheng, Y.-M.; Huang, P.-J.; Wu, J.-H. The foot plantar pressures for patients with hallux valgus combines with or without claw toe. J. Foot Ankle Res. 2014, 7, A110.
- Richie, D.H., Jr. First Ray Function, Metatarsalgia, and Hammertoes: How Are They Connected? In Hammertoes; Springer: Cham, Switzerland, 2019; pp. 33–55.
- Han, J.T.; Koo, H.M.; Jung, J.M.; Kim, Y.J.; Lee, J.H. Differences in plantar foot pressure and COP between flat and normal feet during walking. J. Phys. Ther. Sci. 2011, 23, 683–685.
- Yamada, S.; Hirao, M.; Tsuboi, H.; Akita, S.; Matsushita, M.; Ohshima, S.; Saeki, Y.; Hashimoto, J. Involvement of valgus hindfoot deformity in hallux valgus deformity in rheumatoid arthritis. Mod. Rheumatol. 2014, 24, 851–854.
