Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Biology
Cancer is a serious problem affecting human health and the second most common reason for death throughout human history. In 2014, the pervasiveness of cancer had increased tremendously; approximately 1,665,540 people were suffering from cancer just in the United States alone, and in 2014, 585,720 of them died due to cancer. Unfortunately, this condition manifests itself at the tissue level, making identification and treatment efficacy extremely difficult.
- cancer
- anticancer therapies
- therapeutics
1. Bladder Cancer
Bladder cancer affects approximately 3.2% of the world’s population, making it the most common type of cancer. The RB (retinoblastoma) pathways and the p53 gene are altered in bladder cancer. With the help of Ras-mitogen-activated protein kinase, these genetic pathways promote proper cell development. When the tyrosine kinase receptor is activated by RAS pathways, HARS (Histidyl-tRNA Synthetase) and FGFR3 (fibroblast growth factor receptor 3) mutations cause tumors. The EGFR (epidermal growth factor receptor) and ERBB2 (erb-b2 receptor tyrosine kinase 2) are both activated by the tyrosine kinase. As a result of the receptors’ overexpression, auto phosphorylation and dimerization occur and the tumor-suppressor gene RASSF1A becomes dormant. The p53 gene turns into the TP53 gene in this malignancy, and p53 governs the cell cycle all over the G1-S conversion. The treatment’s chief goal is to reduce gene mutations by inactivating pathways and boosting the transition of the p53 gene to TP53 [32]. The PI3K/Akt/mechanistic target of rapamycin and receptor tyrosine kinase/related RAS viral (r-ras) oncogene homolog 2 (RRAS2) are the main pathways disrupting cell proliferation and survival. The key signaling pathways implicated in bladder cancer are Ras-MAPK and PKC. To improve therapeutic effectiveness, the EGFR (epidermal growth factor receptors) family (ERBB1, ERBB2, ERBB3, ERBB4) targets are employed. The tyrosine kinase domain of the intracellular EGFR is inhibited by small molecules, and the extracellular ligand-binding area is blocked by monoclonal antibodies [33,34]. Natural compounds, e.g., curcumin, sulforaphane, resveratrol, quercetin, etc., decrease VEGF binding and c-MYC and help to cure bladder cancer [35] (Table 1).
Table 1. Clinical trials and characteristics of anti-cancerous medications [29].
| Agent | Features |
|---|---|
| Bevacizumab (Phase III) | VEGF-A binding/inhibition |
| Ziv-aflibercept196 Phase I | VEGF binding/inhibiting agent |
| Cabozantinib (Phase II) | VEGFR-2 inhibitor |
| Pazopanib (Phase II) | inhibitor of several tyrosine kinases |
| Tamoxifen (Phase II) | An antagonist of estrogen receptors |
| Buparlisib (Phase II) | Pi3K inhibitor |
| Dovitinib (Phase II) | FGFR and veGFR inhibitor |
| MeK162 (Phase II) | MeK inhibitor |
| MGAH22 (Phase I) | HeR2-targeting antibody |
| Afatinib (Phase II) | eGFR and HeR2 inhibitor |
| AZD5312 (Phase I) | Androgen receptor antisense inhibitor |
| Everolimus (Phase I) (Phase II) | mTOR inhibitor (mTORC1 and mTORC2) |
| Rapamycin (Phase I) (Phase II) | mTOR inhibitor |
| ABi-009 (albumin-bound rapamycin) (Phase I) (Phase II) | mTOR inhibitor |
| ALT-801 (Phase I) (Phase II) | p53/HLA-A2-expressing tumor cells |
| HS-410 (Phase I) (Phase II) | immune activator along with BCG |
| ALT-803 (Phase I) (Phase II) | immune activator through iL-15 |
| Ipilimumab (Phase II) | CTLA-4 antibody |
| MeDi4736 (Phase I) | PDL1 antibody antagonist |
| Tremelimumab (Phase I) | CTLA-4antibodyDownregulationofT-reg cells |
| AGS15e (Phase I) | Slitrk6 targeting immunotherapy |
| MK-3745 (pembrolizumab) (Phase I) (Phase II) | PDL1 |
| Ad/HeR2/Neu vaccine (Phase I) | vaccination/immune activation |
| SAR566658 (Phase I) | Anti-CA6-DM4 immunotherapy |
| Lenalidomide (Phase I) | Immunomodulation |
| MPDL3280A (Phase I) | Anti-PDL1 immunotherapy |
| Eribulin mesylate (Phase I) (Phase II) | Microtubule formation/mitosis |
| Abraxane (Phase I) (Phase II) | Protein-bound paclitaxel—mitosis |
| Tesetaxel (Phase II) | Tubulin stabilization—antimitotic |
| ASG-22Ce (Phase I) | Inhibition of tubulin formation in cancer cells by targeting cells expressing adhesion molecule nectin-4 with monomethyl auristatin e |
| Amrubicin (Phase II) | Anthracycline targeting topoisomerase ii |
| Gemcitabine | Nucleoside analog targeting S phase |
| 5-Fluoro-2-deoxycytidine with Tetrahydrouridine (Phase II) |
inhibition of DNA methylation/cytosine deamination |
| Romidepsin (Phase I) | HDAC inhibitor |
| BBi608 (Phase I) (Phase II) | Cancer cell stemness |
| Ganetespib (Phase I) | inhibition of HSP90 |
| OGX-427 (Phase II) | HSP27 inhibitor |
| Veliparib (Phase I) | PARP inhibitor |
| Gefitinib (Phase II) | Inhibit EGFR TKI |
| Etunimab (Phase II) | Inhibit EGFR TKI |
| Erlotinib (Phase II) | Blocks EGFR |
| Trastuzumab (Phase II) | Blocks ErbB2 |
| Lapatinip | Reversed inhibition of EGFR and ErbB2 |
| Sunitinib (Phase II) | Inhibition of VEGFR1–3, PDGFR, C-Kit, and Flt3 |
| Pazopanib (Phase II) | Inhibition of VEGFR1–3, PDGFR, and C-Kit |
| Sorafenib (Phase II) | Inhibition of VEGFR2/3, PDGFR, Raf, C-Kit, and Flt3 |
| Ad CMV-TP53 (Phase I) | Delivery of functional TP53 into cells |
| Bevacizymab (Phase II) | Inhibits VEGF antibody |
| Aflibercept (Phase II) | VEGF binding to endothelial cells and blocking VEGFR interaction |
| Curcumin | decrease VEGF binding, c-MYC |
| Sulforaphane | decrease VEGF binding, c-MYC |
| Resveratrol | decrease c-MYC |
| Quercetin | decrease VEGF binding, c-MYC |
2. Breast Cancer
The glandular milk ducts’ or breast lobules’ epithelial cells give rise to the malignant tumor known as breast cancer. Around 2.08 million new cases of breast cancer are identified each year in women worldwide. Hormones have a significant influence on the shape and expansion of epithelial tumor cells in breast cancer. Oestradiol (E2) is the most essential regulator of hormonal changes. The aromatase enzyme transforms androgens most efficiently when it interacts with the cellular oestrogen receptor (ER), specifically with the hormones oestradiol, oestrone, and oestrone-sulfate. Stem cell proliferation, differentiation, and motility are regulated using ERs, HER2, and Wnt/ß-catenin, which are the main regulators for healthy breast development and mammary stem cells. Nevertheless, some evidence emphasizes the idea that noncoding RNAs and epigenetic regulators, particularly in triple-negative breast cancer, might serve crucial roles in breast cancer growth. [36]. There are several kinds of oestrogen receptors, the most prominent of which are ER and ERa. According to studies, almost two thirds of breast tumors express too much oestrogen receptor (ER), and more than 70% of them respond to oestrogen-blocking medications such as SERMs (selective oestrogen receptor modulators) and AIs (aromatase inhibitors). SERMs have tissue-specific action and their activity in different cell types and tissues is principally controlled by the recruitment of different cofactors, including co-activators and co-repressors, to ER target genes [37]. Tamoxifen and raloxifene, for example, oppose oestrogen in breast tissue. Tamoxifen, as opposed to raloxifene, behaves as oestrogen within the uterus and has a strong structural resemblance to that of E2, increasing the risk of uterine sarcoma and endometrial cancer [33]. Tamoxifen and raloxifene both raise the risk of thrombosis [38]. The second important molecular target in breast tumors is epidermal growth factor 2 (ERBB2, formerly HER2 or HER2/new), a transmembrane receptor tyrosine kinase of the epidermal growth factor receptor family. Patients with ERBB2 amplified or overexpressed breast cancer are treated with ERBB2-targeted therapies such as anti-ERBB2 antibodies (trastuzumab and pertuzumab) and small-molecule tyrosine kinase inhibitors (lapatinib and neratinib). The abnormal expression of the molecular targets, including ER, PR, or ERBB2, characterizes triple-negative breast cancer, which is found in nearly 15% of breast tumors. The targeted treatment uses drugs to specifically limit the progress of the disease cells without damaging healthy normal cells, in contrast to chemotherapy, which affects both cancerous and healthy cells equally (Table 2). Some of the approved medications to treat breast cancer include letrozole, ado-trastuzumab emtansine, anastrozole, ixabepilone, everolimus, gemcitabine, abemaciclib, fulvestrant, goserelin acetate, doxorubicin hydrochloride, epirubicin hydrochloride, lapatinib ditosylate, and 5-fluorouracil [36,37,38].Curcumin, epigallocatechin gallate, genistein, lycopene, and other natural compounds help in breast cancer treatment by regulating p53 gene expression, upregulating p21, and activating ERK, Akt, and p70S6 kinases [39].
Table 2. Breast cancer treatment with a specific targeted drugs.
| Target Agent | Process of Intervention |
|---|---|
| Trastuzumab | Suppresses downstream signaling involved in normal cell proliferation, motility, anti-apoptosis, along with malignant cell invasiveness and angiogenesis |
| Pertuzumab | Prevents dimerization among HER2 and further HER family members, particularly HER3, and stimulates ADCC (antibody-dependent cellular cytotoxicity), 16 whereas trastuzumab only averts dimerization among HER2 and other HER family members, particularly HER3 |
| Lapatinib | Hinder receptor phosphorylation and inhibit downstream pathways that affect tumor cell proliferation and survival. |
| T-DM1 (Trastuzumabemtansine) | Transmit the microtubule-inhibitory drug to HER2-positive cancer cells, reducing systemic toxicity along with improving anticancer efficacy |
| Everolimus | Suppress mTOR activation while also efficiently inhibiting upstream signal transmission, which is important for tumor cell development. |
| Ipatasertib | Inhibits AKT |
| Veliparib | PARP1 and PARP2 inhibitors |
| Talazoparib | Inhibits PARP |
| Olaparib | PARP inhibitor with potential anticancer efficacy in BRCA1/2-mutated breast cancer patients |
| Palbociclib, abemaciclib, and ribociclib | CDK4/6 inhibitors |
| Atezolizummab and durvalumab pembrolizumab | Inhibit the PD-1 receptor-mediated negative immune regulatory signal |
| Bevacizumab | Inhibits VEGF |
| Curcumin | regulating p53gene expressions |
| EGCG | upregulation of p21 |
| Genistein | activation of ERK |
| Lycopene | activation of ERK, Akt, and p70S6 kinases |
HER: human epidermal growth factor; PARP: Poly (adenosine diphosphate-ribose) polymerase; CDK: cyclin-dependent kinase; PD: programmed Death; VEGF: vascular endothelial growth factor; AKT: v-akt urine thymoma viral oncogene homolog.
3. Colorectal Cancer (CRC)
Colorectal cancer is the leading cause of death worldwide. Changes in DNA and RNA characteristics caused by the gene mutation produce an imbalance in a biological process. MSI (microsatellite instability), CIMP (CpG island methylator phenotype), and chromosomal instability are all linked to DNA instability, which causes CRC. In the case of MSI, the repetition of DNA sequences base pair produces gene mutation. The DNA-repairing factor MMR (mismatch repair) (seven mismatched repair genes, such as PMS1, PMS2, MLH1, MLH3, MSH6, MSH3, and MSH2) becomes inactive which results in uncontrolled cell growth [40]. In case of CIN (chromosomal instability), the instability of DNA sequences produces a LOH (loss of heterozygosity), which decreases the allele sequencing and alters the tumor suppressor genes. For example, the p53 gene changes into TP53 in DNA, thus forming a tumor. The target is to stop the DNA mutation, deletion, and instability. Genes like C-Myc have an important role in colorectal cancer. The C-Myc gene normally controls different biological effects. Under normal conditions, C-Myc regulates cell growth, maturation, proliferation, cell cycle progression, cell size, and apoptosis [36]. In this case, the unstable gene is the main cause, but gene mutations (BRAF, RAS, TP53, PI3K, and PTEN) also cause tumor growth in the colon or rectum. The changing lifestyle that leads to tobacco use is an external factor in colorectal cancer [40,41]. When the expression of C-Myc gene increases, the signaling pathways are disturbed. Deregulation causes the cell growth to become uncontrolled, and the genomic changes produce cell metastasis. This gene shows a downstream effect on Wnt-Ras-dependent signaling [42] (Figure 3). Chemotherapies are now often utilized to treat colorectal cancer. The most significant motive of the drugs is to decrease tumor formation and inhibit the signaling molecular pathways that increase rapid cell division. Among the drugs used for colorectal cancer, therapies include aflibercept, bevacizumab, ramucirumab, and regorafenib. A monoclonal antibody called bevacizumab has a strong affinity for vascular endothelial growth factor (VEGF). VEGF binds to VEGF-A receptors and inhibits intracellular signaling pathways, such as KIT, B-RAF, RAF-1, P38 MAPK, and Wnt signaling. The Ramucirumab drug is a member of the Ig G1 class. The main target of this drug is VEGFR-2, which helps to inhibit angiogenesis [43]. Curcumin, a natural compound, inhibits NF-κB, reduces TNF production, and inhibits cancer cell proliferation. Chrysin inhibits p53, p38, MAPK, and apoptosis. Quercetin inhibits cell proliferation by suppressing RASA1 (RAS p21 protein activator) expression [44].
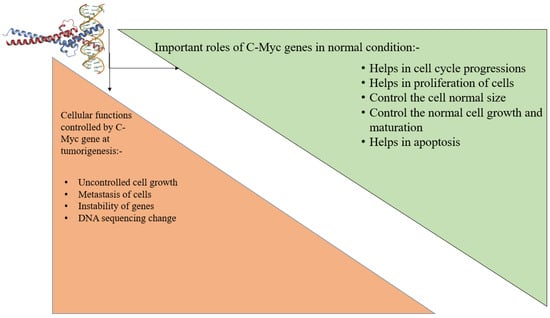
Figure 3. Role of C-Myc gene in normal conditions.
4. Kidney Cancer
In general nephrology, kidney cancer is a very common disease that is also called renal cell carcinoma (RCC) [45]. In this case, tumor formation occurs in the renal epithelial cells and can be cured by damaging or removing the tumors. Here, the mutation of the gene takes place in the homonymous gene, causing Von Hippel-Lindau (VHL) syndrome. VHL genes encode the protein pVHL. The pVHL protein governs the transcription factor of the hypoxia-inducible factor (HIF). In conditions of low oxygen, the pVHL proteins lead to HIF and transcription [40]. Cell growth, vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and transforming growth factor (TGF) are enhanced by its transcription. The genes involved in chromatin modulation are KDM5C, BAP1, SETD2, and PBRM1 [46]. The PI3K/mTOR/AKT signaling pathways are also hampered [47,48]. Studies reported that a high level of CD68+ increases tumor-associated macrophages (TAM). VEGF genes amplify cell growth. The main goal of therapeutics is to block VEGF with a monoclonal antibody. Some drugs are given orally to inhibit the VEGFR with kinase inhibitors. Some drugs target the mTOR pathway and control the pathways by introducing serine-threonine kinases [49]. There are different types of chemotherapy used for the treatment of kidney cancer, e.g., sorafenib, sunitinib, pazopanib, tivozanib, cediranib, dovitinib, and regorafenib (Table 3) [50]. Natural compounds such as quercetin reduce lipid ROS and increase glutathione; luteolin increases the p53 gene and decreases PUMA (p53 up-regulated modulator of apoptosis); and kaempferol suppresses TNF and activates NF-κB [51].
Table 3. Drugs used for Kidney cancer and their targets.
| Name of Drugs | Targets | Reference |
|---|---|---|
| Sorafenib | VEGFR 1–3, C-Kit, PDGFR | [52] |
| Sunitinib | VEGFR 1–3, C-Kit, PDGFR and Fit-3 | [50] |
| Bevacizumab | VEGF | [50] |
| Pazopanib | VEGFR 1–3, C-Kit and PDGFR | [53] |
| Temsirolimus | mTOR | [50] |
| Everolimus | mTOR | [50] |
| Axitinib | VEGFR1–3 | [50] |
| Nivolumab | PD1 | [50] |
| Cabozamtinib | MET, RET and VEGFR2 | [50] |
| Lenvatinib | VEGFR1–3, PDGFRβ, RET, FGFR1–4 and KIT | [50] |
| Regorafenib | VEGFR | [54] |
| Cediranib | VEGFR 1–3 | [55] |
| Dovitinib | VEGFR and mTOR | [56] |
| Quercetin | reducing the lipid ROS | [51] |
| Luteolin | increase p53gene and decrease the PUMA-α | [51] |
| Kaempferol | suppressed TNF-α, activate NF-κB | [51] |
5. Lung Cancer
Lung cancer affects an estimated 1.8 million people annually. Tobacco inhalation, along with passive smoking, is the main cause of lung cancer. Non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) are the most common types of lung cancer. The majority of lung cancer patients have NSCLC, whereas the remaining 15% have SCLC. The three kinds of NSCLC recognized by the World Health Organization are adenocarcinoma, large cell carcinoma, and squamous cell carcinoma. In adenocarcinomas, tumors form inside an airway epithelial cell; large cell carcinoma tumors develop in the large nucleoli and cells of the tissue; and squamous cell carcinoma tumors form in the alveolar cell [49]. Lung cancer is associated with mutations in the AKT, ROS, p53, EFGR, MET, and BRAF genes (Table 4). The TKI-sensitizing mutation occurs at the site of exon 19 after tobacco intake. Rapid cell divisions are accelerated in tumors caused by genetic changes and changes in transducing signaling pathways. Several growth factors, including TGF-β, PDGF, FGF, Keratinocyte Growth Factor (KGF), and Hepatocyte Growth Factor (HGF), increase lung abnormalities by causing the unfolded protein response (UPR) [57,58]. The signaling of KGF promotes pulmonary fibrosis. KGF signaling aids in the upregulation of AKT signaling pathways, which in turn aids in the down regulation of PTEN in lung cells via increasing IKK and NF-ΚB. This results in negative signaling, and cell growth accelerates. As a result, excessive KGF secretion causes lung abnormalities and cancer [59]. Excess HGF synthesis raises the amount of Broncho-alveolar lavage fluid in the lungs [60]. AEC2 DNA synthesis is aided by HGH. The AEC2 typically regenerates lung cells that have been destroyed. As a result, numerous factors alter the nucleotide sequence for the AEC2 gene’s production, resulting in lung cancer. For instance, in endoplasmic reticulum stress, there is a high cellular response to protein expression. The UPR increases the number of mediators produced by DNA, which reduces apoptosis. TGF-1 activates the Wnt–Catenin signaling pathway, making apoptosis more difficult to achieve and leading to lung cancer. The medications’ main targets are PDGF, UPR, TGF and TGF, KGF, HGF, FGF, and Wnt–Catenin signaling [61]. Lirilumab, paclitaxel, pembrolizumab, and other medications are available for the treatment of lung cancer [62] (Table 4). Radiation therapy is also used to treat lung cancer. There are primarily two effective forms of radiation. A type of radiotherapy called intensity-modulated radiotherapy (IMRT) uses a solitary radiation beam to treat an afflicted region. The alternate option remains stereotactic body radiotherapy (SBRT), which involves delivering precise light in the direction of the affected region. Radiation aids in the destruction of damaged cells in particular [63]. Curcumin and β-elemene are natural compounds that inhibit the PI3K/Akt pathway and resist the A549/DPP multidrug [64].
Table 4. Medications regarding lung cancer therapy.
| Drugs | Drugs Mechanism | Tumors Name Which Is Treatable | References |
|---|---|---|---|
| Lirilumab | In CT phase I, halt KIR signaling | Solid-form tumors (Squamous cell carcinoma) | [65] |
| Paclitaxel | Work as Chemo and immune-cytokines | Melanoma, NSCLC | [66] |
| Pembrolizumab | Work against programmed death-ligand 1 by reprogramming NK cells. | NSCLC | [67] |
| Nvolumab | NK cell activation in CT phase II, activity against programmed death-ligand 1. | NSCLC | [65] |
| Curcumin | inhibiting PI3 K/Akt pathway | - | [64] |
| β-elemene | inhibiting PI3 K/Akt pathway | - | [64] |
6. Lymphoma
Lymphoma is a cancer of the lymphatic system. Diffuse large B-cell lymphoma (DLBCL) is perhaps the most prevalent lymphoma among the numerous types [68,69]. The lymphoma is produced by the translocation of MYC. The BCL6 gene is a repressor of transcription that works as a regulator of the germinal cellular process. BCL6 (B cell lymphoma 6) regulates B cell receptor activity as well as the expression of CD40 (clusters of differentiation 40) signaling, which activate NF-κB and MAPK signaling pathways. BCL6 is also involved in the regulation of B cell responses to chemokines and cytokines. BCL6 regulates CD8+ T cell activity in an immune response. After introducing the carcinoma factors to the body, the mutation happens at the gene level. For example, the expression of BCL6 becomes deregulated by the mutation of the BCL6 gene, which produces non-Hodgkin lymphomas. The interaction between the domain BCL6 and the POZ/BTB has decreased as a result of the gene mutation. This lack of interaction produces significant toxicity in the body. When the BCL6 levels decrease, the immune system becomes compromised by the inactivation of the T cell immune response. The cell–cell interaction also decreases, which hampers the transcription codon. The main drug targets for lymphoma are BCL6 and the PI3K delta protein [70]. Bleomycin, etoposide, doxorubicin, vincristine etc. are the medications for lymphoma cancer which are commercially available [70,71].
7. Melanoma Cancer
Melanoma is the most common form of skin cancer and is mainly caused by UV radiation. Every year, approximately 1.7% of new cases of melanoma are diagnosed [72]. In the early stages after sun exposure, the mutation of a normal gene produces an oncogene. The mutation produces the B-Raf proto-oncogene (BRAF) along with the NRAS proto-oncogene (NRAS) [73]. When the skin is exposed to the sun, the gene mutation occurs through the alteration of the gene sequencing and the copying of gene numbers. For example, after sun exposure, C changes to T (UV B) or G changes to T (UV A) [74,75,76]. For the gene mutation, the oncogene activates its signaling and produces BRAFv600, which is formed by the mutation of Val600. After UV radiation on the skin, the normal biological systems will be disturbed, the RAS pathways are activated, and it also activates the MEK1 and MEK2 pathways [77]. These pathways further activate pERK, through which the normal transcription program changes. It can increase cell proliferation and cause changes in glycolysis and mitochondrial metabolism [14]. Aimed at the gene mutation, the tumor protein p53 stimulates mitogen-activated protein kinase (MAPK) pathways. The skin loses its immune system as a result of the gene mutation [78,79]. For the treatment of melanoma cancer, the drug targets will be BRAF and MEK inhibition [71]. Chemotherapy is the most useful treatment for melanoma cancer. Some drugs are PD-1 blocking agents, e.g., Nivolumab and Permbrollizumab, used for melanoma cancer by inhibiting the tyrosine kinase BRAF (Table 5) [80]. The drugs that are much more effective for melanoma treatment are inhibitors of AKT, ERK-1, and ERK-2 activation [81,82]. Natural compounds, e.g., quercetin, kaempferol, and apigenin, inhibit the STAT3 (signal transducer and activator of transcription 3) oncogene and help treat cancer [83].
Table 5. Drugs used to treat melanoma cancer and their targets.
8. Oral and Oropharyngeal Cancer
Approximately 4% of all cancer cases are oral cancer, which remains the sixth most frequently diagnosed cancer worldwide. When the cancer is in the oral cavity, it is called “oral cancer”, and if the cancer is inside the throat, it is recognized as “oropharyngeal cancer”. The main risks factors associated with oral cancer are smoking, betel quid chewing, and alcohol intake [84]. The human papillomavirus (HPV) causes throat cancer, and this virus can be transmitted through sex. In oral cancer, malignant tumors form in the oral mucosal epithelium. When the HPV virus enters the body, it represses the TSS (transcriptional start site) with methylation and increases tumor-specific gene silencing [75]. HPV promotes endothelial cell proliferation, cytoskeletal reorganization, NF-κB activation, and inhibits cell apoptosis. T4SS promotes the proliferation of cells and triggers NF-κB signaling which promotes gene mutation. In other cases, the bacteria also secrete a toxin substance, e.g., cytolethal distending toxin (CDT), colibactin, and cytotoxic necrotizing factor 1, increasing carcinogenicity via genomic instability, decreasing DNA impairment response, and causing cell cycle arrest during G2 or M phase [85]. The drugs for oral and oropharyngeal cancer therapy are cisplatin, carboplatin, 5-fluorouracil (5-FU), docetaxel, paclitaxel, hydroxyurea, etc. [86,87].
9. Pancreatic Cancer
Pancreatic cancer is the most frequently diagnosed cancer globally. Pancreatic cancer patients have a very high fatality rate. In pancreatic cancer, MUC4 (membrane mucin) is among the overexpressed membrane-bound mucins. The MUC4 formation produces neoplastic transformation and tumorigenesis. MUC4 also moderates the interaction of tumor cells with normal cells [80]. MUC4 aids in the metastasis-promoting factor Galectin-3, which aids in gene mutation. In this case, the gene sequencing duplication in allelic produces a variable number of tandem repeat (VNTR) domains in cells. As a result, the cell cycle becomes uncontrollable, accelerates, and results in tumors in target cells. Hence, MUC4, the human mucin gene, has been targeted to treat pancreatic cancer. The inhibition of MUC4 by the RNAs produces a pharmacological effect in pancreatic cancer [88]. Other drugs that are used for this cancer treatment are capecitabine, erlotinib, fluorouracil, gemcitabine, leucovorin, etc. [89].
10. Prostate Cancer
Prostate cancer is a common type of cancer. Specifically, the secretion fluid, which protects sperm during reproduction, feeds and breeds prostate cancer. There are different signaling pathways, e.g., PI3K, PTEN, AKT, and mTOR signaling, that control the normal cell cycle, growth, as well as its proliferation [90]. Under normal conditions, the PI3K sends a signal to IRS-1 via positive feedback; however, in abnormal circumstances, negative feedback increases protein synthesis as well as cell growth. The drug’s main targets are PI3K, AKT, PTEN, and mTOR signaling [91]. The progression of prostate cancer is significantly influenced by androgen. Androgen produces some enzymes that produce cancer; the glycosylation enzymes are GALNT7, GCNT1, UAP1, ST6GalNAc1, ST6GAL1, CSGALNACT1, and EDEM3. The androgen receptor (AR) promotes gene mutation and amplification by activating these enzymes. The chief targets for prostate cancer are eight main enzymes, GALNT7, GCNT1, UAP1, CYP3A4, CYP2C9, ST6GalNAc1, ST6GAL1, CSGALNACT1, and EDEM3 [92]. Radiation therapy is currently being used to treat prostate cancer. Radiotherapy can be used to destroy specific tumor cells, but there is a slight risk of causing negative feedback to neighboring cells. One of the best radiotherapies is brachytherapy. In brachytherapy, iodine, iridium, cesium, and palladium types of radioactive material are inserted into the body to help cure prostate cancer [93]. Bicalutamide, Abiraterone, Enzalutamide, and other drugs are used to treat prostate cancer [94,95] (Table 6). The natural compound berberine is reported to promote p53 genes and ROS production and can be used to treat cancer. It also helps in paraptotis, particularly by causing mitochondrial swelling and ER dilatation [96].
Table 6. Drugs for Prostate cancer and their targets.
| Name of Drugs | Targets | References |
|---|---|---|
| Bicalutamide | CYP3A4, CYP2C9, CYP2D, CPY2C19, Binding of plasma protein | [97] |
| Abiraterone | CYP2C8, CYP1A2, CYP3D6 | [97] |
| Enzalutamide | CYP3A4, CTP2C9, CYP2C19, Pgp, BCRP, OATPs | [97] |
| Abiraterone Acetate | CYP2C8, CYP3D, CYP1A2 | [97,98] |
| Docetaxel | Binding of plasma protein | [87,97,98] |
| Cabazitaxel | CYP3A4, CYP2C8, BCRP, OATP1B1, OATP1B3, UGT, stabilize tubulin | [97,99] |
11. Thyroid Cancer
In thyroid cancer, the tumor forms in the thyroid gland, commonly known as papillary thyroid cancer (PTC). It is formed by PCT-RAS-BRAF molecular signaling. The BRAF gene mutation is most common in PTC [100]. Studies reported that the deregulation of microRNAs (miR-146b) produces the PTC in several ways. In the case of PTC, the genetic rearrangement in the RET/PTC and NTRK pathways produces tumors by activating the MAPK pathway. MAPK signaling mutates the BRAFV600E gene, which produces metastasis of lymph nodes and tumors. The miR-146a and miR-146b are post-transcriptional gene silencers that play an important role in the immune system [100]. For the gene mutation, the codon gene sequencing is changed. For that, miR-146a and miR-146b are changed into MIR146A and MIR146B. As a result, the chromosomal sequence changes and increases NF-κB signaling. This signaling helps to increase platelet-derived growth factor (PDGF), which increases cancer cell size with the help of growth factor receptor signaling. The Wnt/-catenin pathways are activated after genetic changes by modulating the epithelial-mesenchymal transition (EMT). Negative regulation of the miR-146b gene results in HDAC3 increasing and producing radioactive iodide sensitivity in thyroid cancer cells. As a result, the p21 gene produces a protein that controls tumor proliferation. Following numerous studies, researchers conclude that the main drug target for treating thyroid cancer is the PTC-RAS-BRAF/RET signaling pathways [101]. Drugs that are commercialized to treat thyroid cancer are Axitinib, Lenvatinib, Cabozantinib, etc. [100] (Table 7).
Table 7. Drugs utilized for various types of thyroid cancers along with their target.
| Drugs | Drugs Targets | Treatment for Various Cancer Types | References |
|---|---|---|---|
| Axitinib | TKI, VEGFR1–3 | ATC, MTC, and DTC | [102,103] |
| Lenvatinib | TKI, VEGFR1–3, FGFR1–4, RET, PDGFR | ATC, MTC, and DTC | |
| Cabozantinib | TKI, VEGFR2, MET, FLT3, RET, c-kit | DTC and MTC | |
| Dabrafenib | STKI, BRAF V600E, MEK1 &2 | ATC and DTC | |
| Everolimus | m-TOR | RCC, TS, SEGA | |
| Pazopanib | TKI, VEGFR1–3, FGFR1–4, RET, PDGFR, c-kit | ATC, MTC, and DTC | |
| Larotrectinib | NTRK | NTRK-fused thyroid cancer | |
| Sorafenib | TKI, VEGFR1–3, FGFR1–4, RET, PDGFR, c-kit, BRAF | ATC, MTC, and DTC | |
| Sunitinib | TKI, VEGFR1–3, FGFR1–4, RET, PDGFR, c-kit, CSF-1R | DTC and MTC | |
| Vandetanib | TKI, VEGFR2–3, RET, EGFR | Only MTC | |
| Vemurafenib | BRAF V600E | Only PTC |
12. Uterine Cancer
Uterine cancer is one of the most common cancer types in women of reproductive age. The formation of tumors in the uterus produces uterine cancer. In the case of lymphoma, the extracellular matrix (ECM) protein level increases, increasing Rho/ERK/p38 MAPK signaling. The ECM protein regulates cytokines and steroid hormones. In this case, TGF-s and activin-A play an important role in myofibroblasts’ production and promote fibrosis. ECM activation activates FAK (focal adhesion kinase) polymerization and AKAPI3, Rho A, which interacts with ROCK (Rho-associated kinase) receptors along with stimulating ERK and p38 MAPK signaling. The tumor formation in the uterus during reproductive age produces chronic inflammation. In that case, surgery is the first choice, but there is a risk because surgery can produce a negative effect on cell proliferation as well as gene mutation. As a result, primary drug targets are used to inhibit TGF-signaling and TGF-signaling [104].
13. Adenoid Cystic Carcinoma (ACC)
Adenoid cystic carcinoma happens to be an uncommon cancer with a slow pace of progression. This type of tumor has been discovered in approximately 1% of all cancers worldwide. This type of cancer affects the salivary glands of the head and neck region, tongue, palate, lacrimal gland, and so on. This type of tumor forms in epithelial cells [105]. These types of cancer form by the mutation or deletion of homozygous F-Box and the repeat domain of WD, comprising seven genes (FBXW7). The carcinoma cells are specially divided into two types: one is myoepithelial cells that are present in the periphery of tubules in a proper arrangement, and the other is ductal cells that are present in a pseudo-lumens way [106]. This type of cancer also depends on the mutation of the PTEN, FGFR4, FGF16, and 1LR17RD genes [107,108]. These tumors form via two main pathways, one of which is the activation of the Wnt/-catenin signaling pathway, which increases the transcription level factor Sox4 in RNA and results in tumor formation. The other pathway is the high level of tyrosine kinase c-KIT, whose overexpression increases FGFR1 (fibroblast growth factor receptor 1), HER2, and EGFR. They aid in the deletion of specific chromosomal sequencing, resulting in the production of MYB oncoproteins and a decrease in cell apoptosis [107]. Some of the apoptosis markers are BCL2, API5, BIRC3, and SET. These markers also increase the PI3K pathways for tumor production. So, the main drug target to treat this kind of cancer is the inhibition of the MYB oncoprotein [105]. Drugs, e.g., Axitinib, Dovitinib, and Nelfinavir, are used to treat this type of cancer (Table 8) [109,110].
Table 8. Drugs, their targets, and cause of Adenoid Cystic Carcinoma.
14. Amyloidosis Cancer
Amyloidosis cancer is among the rarest cancers in which the clonal disorder is shown in plasma cells. Here, the decreasing number of B cells produces organ dysfunction. The CD38 gene is activated and binds to daratumumab. After binding its Fc fragments, it produces a natural killer cell, damaging normal cells. The main target to treat this cancer is the CD38 gene [112]. This type of cancer is produced by genetic disorders, e.g., a mutation of gelsolin, apolipoprotein, and transthyretin (TTR). For that reason, tumors in the heart, kidney, nerves, and gastrointestinal tract also produce insoluble amyloid fibrils [113]. The drugs are targeted to inhibit the transcription of the TTR genes. This disease can be determined by measuring the level of monoclonal protein (MP) in serum and urine. Thalidomide, in combination with dexamethasone and cyclophosphamide, is the most commonly used drug. It aids in healing by inhibiting toxicity in the body. Other medications, e.g., lenalidomide and melphalan, are used to treat this form of cancer [114].
15. Anal Cancer
It is an extremely rare kind of cancer that mostly affects women. Each year, around 0.5 percent of cancer cases are of this kind. The HPV (Human papillomavirus) virus is mostly responsible for this form of cancer [115]. The HPV virus induces cancer in the cells of the squamous tissues. The major origin of cancer is the HPV virus transmitted during sexual contact. The cancer causes include tobacco inhalation, aging, and immunological suppression in HIV/AIDS patients. HPV virus contains E6 and E7 viral proteins as well as dsDNA. Viral protein E6 attaches to the tumor suppressor p53 in the cell, causing p53 to be damaged and cell proliferation to rise. Retinoblastoma attaches to E7 which prevents apoptosis, resulting in an unregulated cell cycle [116]. Anal cancer is caused by mutations in the TP53, PIK3CA, and FBXW1 genes, as well as MYC, RICTOR, SOX2 gene amplification, and PTEN gene deletion [117]. Fluorouracil is used to treat anal cancer. Mitomycin C or cisplatin is frequently combined with fluorouracil for anal cancer treatment [118]. Similarly, radiotherapy can be utilized to treat anal cancer since it aids in the destruction of particular tumor cells in specific regions [119].
16. Astrocytoma Cancer
Astrocytoma is a rare form of cancer that develops on its own. It is most commonly observed in children. The gene mutation in the cerebrospinal fluid is caused by NF2 (neurofibromatosis type 2). The SCH (schwannoma) gene is encoded by the NF2 gene, which causes mutations in the SMARCB1 gene and causes tumors. The MRI is used to diagnose this type of cancer [120]. The major goal is to inhibit the production of NF2 genes and prevent NF2 genes from causing gene mutations. Astrocytoma cancer is treated with medications, such as afinitor, everolimus, bevacizumab, carmustine, temodar, temozolomide, avastin, lomustine, etc. [121,122].
17. Bone Cancer
Bone cancer is becoming a more common malignancy. When the bone is destroyed, sufferers experience discomfort. An increase in gene mutations activates the mTOR pathway. The mTOR pathway regulates the phosphorylation of 4E-binding proteins. The phosphatidynositide 3-kinase transforms the p70 ribosomal S6 protein kinase (p-PI3K). A bone tumor results from an increase in protein kinase caused by PI3K-L signaling [123]. Sclerostin is another bone cancer route. It primarily acts by enhancing the connections between tumors and normal cells. It promotes the generation of cytokines that inhibit bone resorption. Sclerostin raises RANKL (Receptor activator of nuclear factor κB), resulting in an increase in osteoclasts and a reduction in bone remodeling [124]. Sclerostin and the mTOR pathways are the key therapeutic targets.
This entry is adapted from the peer-reviewed paper 10.3390/molecules28020750
This entry is offline, you can click here to edit this entry!
