Cesarean section is a surgical procedure, which is the most frequently performed in gynecology and obstetrics. It is commonly believed that an operative delivery is a less painful and safer mode of delivery, which translates into an increasing number of the procedures performed without medical indications.
The maternal sequelae of cesarean sections are well elucidated and widely discussed in the literature, while long-term neonatal consequences still remain the issue of research and scientific dispute.
- cesarean section
- neonatal outcomes
- respiratory disorders
- neurological disorders.
1. Introduction
Cesarean section is the most common surgical procedure performed in women worldwide. Notably, a high percentage of surgical deliveries did not translate into reduced maternal or neonatal mortality [1,2,3,4,5]. According to the recommendations of the World Health Organization (WHO) the rates of cesarean sections should range between 10 and 15% [6]. However, the fear of labor pains and simultaneous concern about the baby to be born, are more and more commonly leading to women choosing to deliver by cesarean section [7,8]. The probability of complications secondary to the implemented procedure increases with the increasing percentage of cesarean sections. Globally, perinatal mortality rates reach 19 out of 1000 children [9]. As regards African countries—1 in 23 neonates dies as a consequence of cesarean section [10], while in developed countries it is believed that the procedure may prevent severe perinatal complications.
According to an increasing number of epidemiologic studies, children delivered by cesarean section more commonly developed respiratory and neurological disorders (e.g., autism spectrum disorders [11], schizophrenia [12]) and immune-related diseases, such as asthma [13,14], skin atopy [15], juvenile arthritis, coeliac disease [16], type 1 diabetes (T1D) [17] or obesity [1,18,19,20,21,22,23]. It is worth noting differences between the occurrence of the above-mentioned conditions in cases when the surgical procedure was performed after delivery had started.
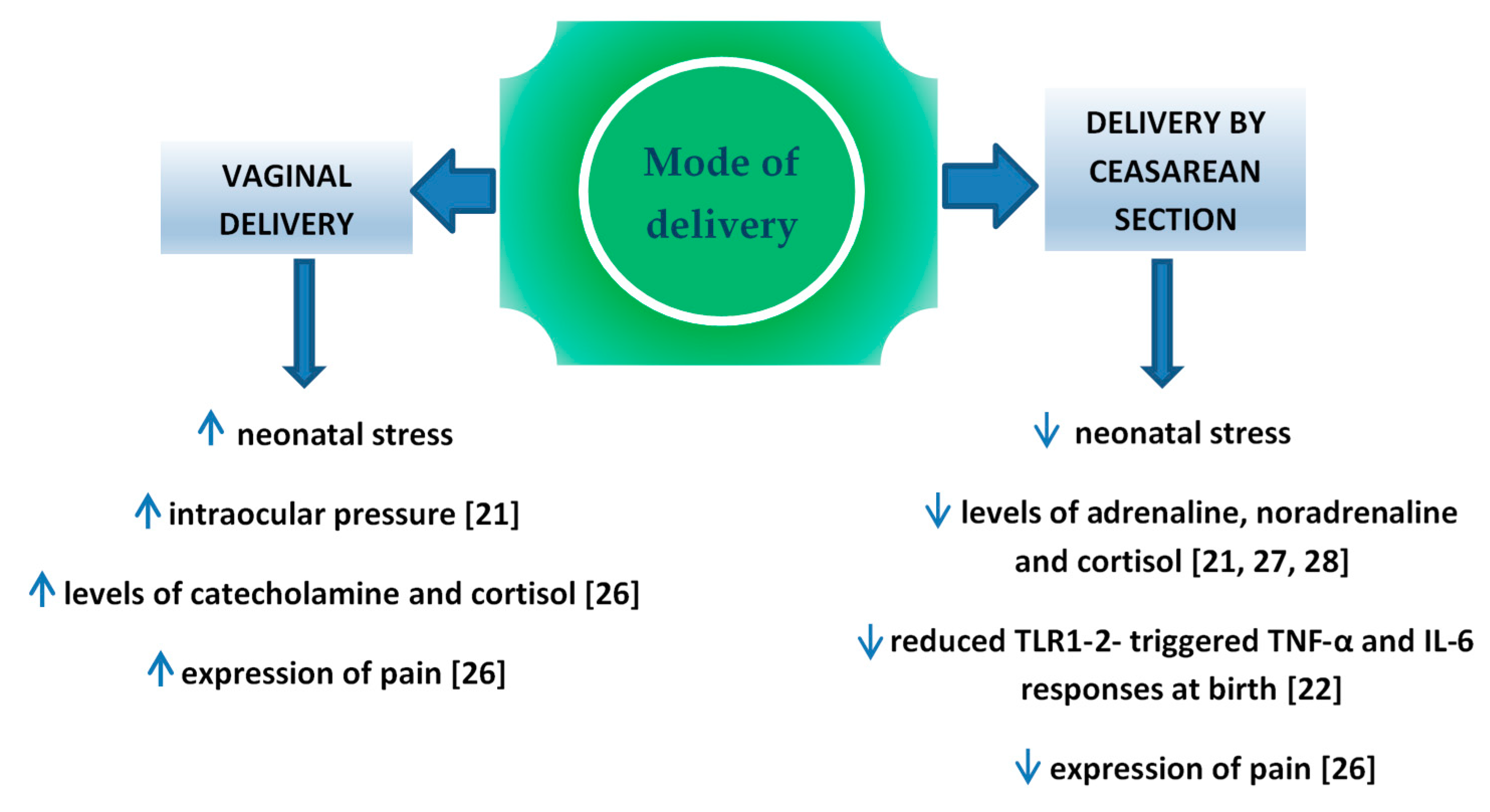
Perinatal stress leads to the increased production of catecholamine and cortisol in the infant’s blood [21]. It is important for the development of pulmonary maturity [24] and the adaptation of the circulatory system to extrauterine life [25]. The completion of pregnancy without associated neonatal stress (i.e., in case of an elective cesarean section) is a potential factor which may interfere in those processes. Schuller et al. claimed that neonates delivered vaginally were characterized by higher cortisol levels and presented higher expression of pain compared to children delivered by cesarean section [26]. In the case of infants delivered by cesarean section, the level of cortisol measured in the umbilical cord blood was significantly lower compared to vaginally delivered neonates [27,28,29] or to vacuum-assisted delivery [30], which might result in the increased percentage of adaptation complications, such as respiratory distress syndrome (RDS), persistent tachypnea or pulmonary hypertension which require hospitalization in the neonatal intensive care unit (NICU). In turn, prolonged NICU stay may be associated with a higher risk of the implementation of iatrogenic procedures [31,32] and longer total postnatal hospitalization. Delivery-related stress causes the activity of various cytokines, therefore changes in this process may have impact on the developing immune system. In the Taiwanese study, Liao et al. [22] reported also that TNF-α and IL-6 response toward TLR1–2 stimulation was significantly reduced in CS delivered neonates than in those delivered vaginally (Figure 1).
The disturbed colonization with bacterial microflora within the skin and digestive tract was the reason for a more frequent occurrence of immune diseases in children delivered by cesarean section [33]. The possibility of the transfer of those bacteria to the neonatal digestive tract is higher in case of long-term contact with the vaginal flora during vaginal delivery [34]. An increasing number of authors emphasized the contribution of maternal rectal microbiome to the optimal colonization of neonates [35,36]. The colonization is also promoted by pH in the stomach of neonates, which thanks to the swallowing of the amniotic fluid in utero, becomes neutral and provides conditions for the survival of aspirated bacteria. Lactobacillus, Bifidobacterium and Bacteroides are the dominant species of intestinal bacteria occurring at the early postnatal period in vaginally delivered neonates [34]. The bacteria play an important part in the regulation of the immune system [37] influencing the level of NK (natural killer) cells [38], regulating the population of T lymphocytes [39,40] the secretion of IgA antibodies [41], and the synthesis of proinflammatory cytokines [42,43,44]. Lactobacillus bacteria may prevent airway hyperresponsiveness by limiting the presence of inflammatory cells in the peribronchial tissue [45], while Bifidobacterium species prevents intestinal necrosis and plays a role in the regulation of the body weight of an infant [46,47]. Numerous authors emphasized both quantitative and qualitative differences in the intestinal microflora depending on the mode of delivery completion. It was reported that the meconium of neonates delivered by cesarean section included reduced amounts of Lactobacillus, Bifidobacterium, Bacteroides and Prevotella bacteria, while the dominant ones included iatrogenic bacterial species or ones which colonized the skin, i.e., Staphylococcus [34], Streptococcus [48], Klebsiella, Enterococcus and Clostridium [49]. Bifidobacterium species, responsible for the synthesis of short-chain fatty acids (SCFA), undergo a relatively rapid elimination from the digestive tract of neonates delivered by cesarean section [34]. SCFAs are a type of communicators between the microbiome and the immune system contributing to the maintenance of balance between pro- and anti-inflammatory reactions, e.g., by transferring the signal with a group of G protein-coupled receptors (GPR), which are present not only on the cells of the gastrointestinal system, but also of the immune and nervous system. It is believed that SCFAs may modulate the weight and reduce the amount of consumed food by the stimulation of enteroendocrine L cells responsible for releasing peptide YY (PYY) and glucagon-like peptide 1 (GLP-1) [50]. Therefore, they may influence the body weight of neonates. However, the role of bacterial microflora is still ambiguous in the development of type 1 diabetes [51].
Numerous authors of epidemiological studies emphasized a correlation between environmental factors influencing the fetus prenatally and over the early postnatal period and the development of circulatory system diseases, diabetes, obesity, tumors [52,53,54,55] and schizophrenia [56] in adulthood. The Epigenetic Impact of Childbirth (EPIIC) study demonstrated that the use of oxytocin, antibiotics and cesarean section may lead to long-term health implications [57]. The authors suspected that epigenetic mechanisms which influenced gene expression modification might be responsible for the phenomenon [57]. DNA methylation is a well elucidated epigenetic mechanism. It consists in adding a methyl group to cytosine-5-carbon in a reaction catalyzed by deoxyribonucleic acid methyltransferase (DNMT). CpG island hypermethylation within a gene promoter most commonly results in the reduction or inactivation of its expression [58,59]. Research showed that tobacco smoking, malnutrition, and long-lasting maternal stress during pregnancy might lead to silencing the expression of some genes in the fetus resulting in a variety of clinical consequences [60,61,62]. According to some researchers, cesarean section changed the global DNA methylation and the methylation of individual genes. Schlinzing et al. demonstrated a higher global methylation in the leukocytes of the umbilical cord blood in a group of elective cesarean sections [63] while Słabuszewska et al. showed a significantly lower global methylation of DNA in the placenta of women following a cesarean section [64]. Franz et al. found no differences in the global methylation of DNA between vaginal deliveries and cesarean sections, although the methylation of individual genes was significantly higher in neonates delivered by cesarean section [65]. Notably, the above mentioned studies vary in terms of methodology which may contribute to differences in the results. Therefore, the issue of the influence of cesarean section on changes in DNA methylation and its clinical implications still remains the subject of research.
2. Influence of Cesarean Section on Fetuses' Health
The stimulation of the hypothalamic-pituitary-adrenal axis (HPA) in the fetus leads to the increase in stress hormones contributing to lung maturation [91], thereby reducing the postnatal manifestations of respiratory insufficiency [92]. Another analysis of a multicenter World Health Organization Multicounty Survey on Maternal and Newborn Health (WHOMCS) revealed that cesarean section increased morbidity in neonates [93]. The most common complications listed by researchers include respiratory disorders, transient tachypnea or postpartum hypoglycemia [94,95]. The frequency of those complications was influenced by the co-existence of childbirth which significantly decreased the occurrence rates of such disorders [66,96].
In the case of an elective cesarean section, the risk of respiratory morbidity including transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS), and persistent pulmonary hypertension (PPH) at 37 weeks of gestation reached 10%, while with vaginal delivery the risk was 2.8% [67]. Previously, infants delivered by caesarean section were demonstrated to have significantly lower compliance of the respiratory system at the age of 1 year than those after vaginal delivery [22]. The authors however, did not observe differences in the resistance of the respiratory system and maximal expiratory flow at functional residual capacity between the groups depending on the type of delivery. Hansen et al. [66] reported that the percentage of complications was affected by cesarean section procedures and by the duration of the pregnancy. The risk of developing RDS after cesarean section at 37 gestational weeks increased 4-fold (odds ratio (OR) 3.9, 95% confidence interval 2.4 to 6.5), while at 39 weeks it was half lower (OR 1.9, 95% confidence interval (CI) 1.2 to 3.0) [66]. Similar conclusions were reached following an Israel study including 132,054 cases. Hospitalizations of offspring involving respiratory morbidity were significantly common in offspring delivered caesarean section (5.2% vs. 4.3% in vaginal deliveries [67]. Table 1 presents characteristics of studies regarding the impact of cesarean section on offspring respiratory morbidity. Currently, a prophylactic dose of corticosteroids is used in everyday clinical practice in order to avoid respiratory complications associated with elective cesarean section and premature delivery [97,98,99]. Numerous epidemiological studies demonstrated a correlation between cesarean section and an increased risk of developing immune diseases, including bronchial asthma [68,69,70,100], allergic rhinitis [101], ulcerative colitis, type 1 diabetes mellitus [17,71], celiac disease [102] and obesity [72,103].
Cesarean section is supposed to protect the neonate and its neurological consequences may differ depending on obstetric indications. In case of an elective cesarean section performed because of breech presentation or a fetal-pelvic disproportion both the mother and the fetus are subjected to limited stress unlike with intrapartum acute cesarean section. Animal research attracted attention to behavioral disorders of the offspring of females who had undergone cesarean section [106]. However, studies concerning children delivered by cesarean section demonstrated contradictory results, which assessed the prevalence of autism spectrum disorders (ASD), ADHD or behavioral disorders [82,107], especially if the analyses comprised the effect of environmental factors. A meta-analysis of the neurological consequences of surgical deliveries published in 2019 confirmed a higher risk of developing autism spectrum disorders (OR 1.33; 95% CI, 1.25–1.41) and ADHD (OR 1.17; 95% CI, 1.07–1.26) in children delivered by cesarean section. However, findings concerning intellectual deficits, obsessive-compulsive disorders, tics and eating disorders were not so explicit. The study based on 300 children at pre-school age reported that mode of delivery has no impact on IQ score [108]. In turn, the study performed in sizeable group of 5000 pre-school children showed that children delivered by caesarean section had significantly higher IQ test scores.
However, the authors observed no significant difference in IQ scores between caesarean delivery and natural vaginal delivery groups after adjusting of among others maternal and paternal education, maternal age and parity [109]. Zhang et al. [110] reported no correlation between the procedure of cesarean section and the risk of developing depression, affective and non-affective psychosis. On the other hand, Baumfeld et al. conducted a prospective cohort study and demonstrated that cesarean section was an independent factor affecting neurological disorders in children along with birth weight, maternal age, Apgar score, gestational age and the sex of the neonate [83]. Recent data by Sadowska et al. [84] demonstrated that delivery by cesarean section increased the risk of epilepsy over two-fold (OR 2.17) in the patients with cerebral palsy. Deoni et al. [111] demonstrated for the first time that caesarean section may be related with changes in brain development, at least during early infancy. The authors observed delivery mode-related differences in white matter development during infancy, which involved the frontal, temporal, and parietal lobes as well as corpus callosum. Children delivered by cesarean section showed significantly lower white matter development in widespread brain regions and simultaneously lower functional connectivity in the brain [112].
3. Summary
According to literature children delivered by cesarean section more commonly develop respiratory disorders and manifest the asthma, while the risk of developing obesity or neurological disorders is still under discussion.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17218031
