Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Earthquakes are among the most impressive natural phenomena with very high potential to set off a chain of effects that significantly affects public health. Related disasters are attributed not only to the strong ground motion and coseismic phenomena but also to secondary effects, comprising mainly landslides and tsunamis, among others. All these can create harsh conditions favorable for the emergence of infectious diseases.
- infectious diseases
- earthquakes
- landslides
- respiratory infection
1. Introduction
Upper respiratory tract infections were observed quite frequently in the short-term period after disasters induced by earthquakes generated in several continents, including North America (the 1994 Northridge [68,69], 2001 El Salvador [70,71], and 2010 Haiti earthquakes [72,73,74,75,76,77], Europe (the 2009 L’Aquila earthquake [78] and 2014 Cephalonia Island earthquakes [79]), and Asia (the 1995 Kobe [80], 1999 Chi-Chi [81,82], 2003 Bam [83,84], 2004 Sumatra-Andaman [85], 2005 Kashmir [86,87], 2009 Sumatra [88], 2009 Samoa [85], 2011 Tōhoku [85,89], 2013 Lushan [90,91], 2013 Bohol [92,93], 2015 Gorkha [94,95,96,97,98,99] and 2016 Kumamoto earthquakes [100]) (Figure 1). Most of the earthquake-affected people lived in overcrowded evacuation shelters, with inadequate air ventilation, unsafe drinking water, and poor personal hygiene being among the possible predisposing factors of contracting respiratory infectious diseases [70,71,72,80,81,82,83,84,87,88,90,92,95,96,98,100]. More details on the respiratory infectious diseases transmitted during the post-earthquake period in earthquake-affected areas are presented in brief in Table 1 and in detail below.
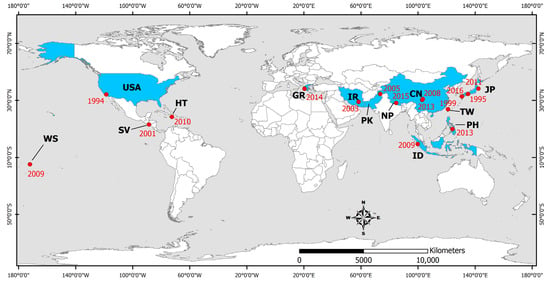
Figure 1. Distribution of countries affected by earthquakes that triggered the occurrence of respiratory tract infections. WS: Samoa, USA: United States, SV: El Salvador, HT: Haiti, GR: Greece, IR: Iran, PK: Pakistan, NP: Nepal, CN: China, JP: Japan, TW: Taiwan, PH: Philippines, ID: Indonesia. The epicenters of the studied earthquakes are also illustrated (red dots) along with the occurrence year (red numbers).
Table 1. Respiratory infectious diseases transmitted during the post-earthquake period in earthquake-affected areas.
| Earthquake Occurrence (DD/MM/YYYY) |
Earthquake Affected Area |
Infectious Diseases (Causative Factors–Cases, Outbreaks, Epidemics) |
References |
|---|---|---|---|
| 17/01/1994 | Northridge California, United States |
Outbreak of coccidioidomycosis (Coccidiodes immitis), 203 cases (including 3 deaths) | [68] |
| Outbreak of coccidioidomycosis (C. immitis) | [69] | ||
| 17/01/1995 | Kobe, Japan | Increase in the number of patients with respiratory diseases by 4.5 times | [80] |
| 21/09/1999 | Chi-Chi, Taiwan |
Acute respiratory infections | [81] |
| Upper respiratory tract infection | [82] | ||
| 13/01/2001 | El Salvador | Upper respiratory infections (30%) | [70] |
| Respiratory infections | [71] | ||
| 26/12/2003 | Bam, Iran | Respiratory infections (6.86% of the total population within 1 month) | [84] |
| Respiratory tract infections | [83] | ||
| 08/10/2005 | Kashmir, Pakistan |
Viral upper respiratory tract infection (23%) | [87] |
| 12/05/2008 | Sichuan, China | Increase of tuberculosis cases in hospitals of the affected area | [101] |
| 30/09/2009 | Sumatra, Indonesia |
Respiratory infections | [88] |
| 12/01/2010 | Haiti | Acute respiratory infection (16.3%) | [72] |
| Increase in tuberculosis in the affected population: 3-fold in a camp for internally displaced persons (693/100,000) and 5-fold in an urban slum (1165/100,000) | [75] | ||
| Tuberculosis | [76] | ||
| 11/03/2011 | Tōhoku, Japan | 43% of cases-community pneumonia (Streptococcus pneumoniae, Moraxella catarrhalis and Haemophilus influenzae) | [89] |
| 20/04/2013 | Lushan, China | Respiratory tract infections | [90] |
| Respiratory infection (45.7%) | [91] | ||
| 15/10/2013 | Bohol, Philippines |
Acute respiratory infections | [92] |
| 476/3555 children: positive to tuberculin skin reaction–TST, 16 with active tuberculosis | [93] | ||
| 26/01/2014 03/02/2014 |
Cephalonia, Greece | Increase of respiratory infection cases | [79] |
| 25/04/2015 | Gorkha, Nepal | Pneumonia and post-streptococcal glomerulonephritis: high incidence among children from affected areas | [98] |
| Upper respiratory tract infections | [95] | ||
| Infections of the respiratory tract (42.3%) | [96] | ||
| 1 case of tuberculous peritonitis (1 girl 14 years old with fever, abdominal pain and vomiting) | [99] | ||
| 14/04/2016, 16/04/2016 | Kumamoto, Japan |
Upper respiratory infections | [100] |
2. Viral-Associated Diseases
In addition to the number of injuries that increased due to the 1995 Kobe earthquake, the number of respiratory diseases, mainly pneumonia, increased about 4.5 times in one month [80]. In February 1995, 24 pneumonia patients with an average age of 79 years were admitted and the mortality rate was 25%. In contrast, one year earlier, the mortality rate was 14%, as only one of the seven pneumonia patients with an average age of 66.5 years died [80].
The number of acute respiratory infection cases detected in the affected area after the 1999 Chi-Chi (Taiwan) earthquake was higher than that of neighboring unaffected counties [81,82]. Most of the disaster victims lived in emergency camps [82]. It is noteworthy that the incidence of these infections decreased to normal expected levels four weeks after the earthquake [81] revealing the association between the earthquake occurrence and the emergence and transmission of infectious diseases among the affected people.
Surveillance of infections in the rural town of San Sebastian after the 2001 El Salvador earthquake showed that upper respiratory infections (30%) were the second most prevalent after skin infections [70].
Survivors of the 2003 Bam earthquake in Iran were temporarily housed in tents and received daily visits as part of an infectious disease surveillance system. Upper respiratory tract infections were recognized as the most common problem. Overall, 792 cases occurred 3 weeks after the earthquake due to the low temperatures, especially at night [83]. The study by Jafari et al. [84] confirmed that the most common cause of admission to health care centers was acute respiratory infection. Considering the total population of Bam after the earthquake (90,928 residents), the incidence of respiratory infection within 1 month was 686 per 10,000 inhabitants, corresponding to 6.86% of the total population [84].
A search of the medical records of all outpatients examined between August 2006 and December 2008, following the 2005 Kashmir earthquake in Pakistan, showed that the most common condition was viral upper respiratory tract infection (23%) [87].
After the 2009 Sumatra earthquake, 1015 patients were examined at two primary health care clinics. Respiratory diseases accounted for the most frequent diagnoses [88].
After the 2010 Haiti earthquake, approximately 42,361 cases were recorded during the period from 25 January to 24 April 2010. Nationally, the most commonly reported cases were acute respiratory infections (16.3%) [72].
Ten days after the 2013 Lushan earthquake in Sichuan Province (China), common infectious diseases recorded in children included respiratory infections, among others [90].
In the Philippines in 2013, disasters were attributed to different types of natural hazards: a flood, an earthquake, and a typhoon. Communicable infectious diseases were the predominant group of diseases recorded in all three types of disasters and included acute respiratory infections [92].
Cephalonia Island (Ionian Sea) is located in one of the most seismic active areas of Europe. It was affected by the early 2014 earthquakes, on January 26 and February 3 with Mw = 6.1 and Mw = 5.9, respectively. The earthquakes were generated during the winter period characterized by low temperatures and rainfall for several days between the two events, leading to an increase of respiratory infection cases [79].
Contagious airborne diseases were among the most common findings observed after the 2015 Gorkha earthquake [95]. Among the 108 pediatric patients examined, respiratory tract infections were observed in 42.3% of the patients [96]. The study conducted by Giri et al. [98] confirmed the results of Wang et al. [96]—that earthquakes can affect children in any age group and children are one of the most vulnerable population groups [98]. Among the 1057 patients examined, the percentage of patients requiring admission for pneumonia was significantly higher among children from areas and families significantly affected by the earthquake [98]. Therefore, ensuring well-functioning water and sanitation systems, temporary shelter and housing assistance, functional primary health care services, and effective systems for surveillance and registration of infectious diseases are vital for the livelihoods of displaced populations [95].
The two earthquakes that struck Kumamoto (Japan) in April 2016 caused evacuation in the earthquake-affected area. Evacuees were forced to spend an extended period of time in temporary camps and experienced upper respiratory tract infections, among other gastrointestinal and skin infections [100].
As regards the impact of earthquake-induced tsunami on public health, it is demonstrated that the harsh conditions following the Indian Ocean tsunami caused by the Mw = 9.2, Sumatra–Andaman earthquake on 26 December 2004, the Samoa tsunami caused by the Mw = 8.1, Samoa earthquake on September 29, 2009, and the Great East Japan tsunami caused by the Mw = 9.0, Tohoku (Japan) earthquake on 11 March 2011, have favored the emergence and incidence increase of respiratory infectious diseases [85]. Among tsunami survivors who had narrowly avoided drowning, polymicrobial respiratory infections (RIs) were frequently found. Throughout the period of influenza transmission, influenza outbreaks were frequently detected. Increased incidence of acute RI, measles transmission, and tuberculosis detection were all impacted by overcrowding in evacuation facilities [85]. More details on the respiratory infections following earthquake-induced tsunami can be found in the review conducted by Mavrouli et al. [85].
3. Fungal-Associated Diseases
Coccidioidomycosis
After the Northridge earthquake, between 24 January and 15 March 1994, Ventura County (California) experienced a major epidemic of coccidioidomycosis, a respiratory disease caused by inhalation of airborne spores of the dimorphic fungus Coccidiodes immitis, which grows in the upper layers of soil in limited semi-arid areas of the western hemisphere (e.g., southwestern United States, Mexico, and parts of Central and South America). Approximately 60% of infected individuals are asymptomatic. The disease most commonly presents as an influenza-like respiratory illness, although a wide range of clinical symptoms may occur. Overall, only 1 in 200 people infected with C. immitis develop diffuse diseases [68].
Landslides that occurred after the earthquake and its strong aftershocks in the Santa Susana Mountains located north of Simi Valley resulted in dust clouds that were dispersed into nearby valleys by northeasterly winds [69]. Following the landslides, the number of coccidioidomycosis cases in the region increased dramatically and peaked 2 weeks after the earthquake as 203 cases of coccidioidomycosis or valley fever were identified, of which 56% occurred in the town of Simi Valley.
Individuals who reported physical presence in dust clouds were 3 times more likely to be diagnosed with acute coccidioidomycosis than those who did not. The risk of being diagnosed with acute coccidioidomycosis increased with increasing duration of exposure and staying in dust clouds [68].
Both the location and timing of the outbreaks strongly suggest that the outbreak of coccidioidomycosis in Ventura County was caused when arthrospores of C. immitis spread with dust clouds due to landslides caused by the 1994 Northridge earthquake [69].
4. Mycobacterial-Associated Diseases
Tuberculosis
Following the 2013 Bohol (Philippines) earthquake, an assessment of the risk of Mycobacterium tuberculosis infection in children from earthquake-affected areas showed that of the 5476 children tested, 355 were positive for the tuberculin skin test, used to diagnose latent tuberculosis, and 16 had active tuberculosis. Although the prevalence of tuberculosis did not differ significantly between areas that were severely or less severely affected by the earthquake, living in a shelter with >25 people was found to have a significant effect on the tuberculosis incidence. Tuberculin skin test positivity appeared to be associated with older age, previous tuberculosis treatment, known contact with a person with tuberculosis, and living on a geographically isolated island. These data should be taken seriously in the design of national tuberculosis control programs, particularly with regard to the role that children’s vulnerability and geographically isolated communities play in the transmission and maintenance of tuberculosis [93].
In 2010, Haiti suffered a devastating earthquake that destroyed the healthcare infrastructure in the capital Port-au-Prince and left 1.5 million people homeless. Subsequently, there was an increase in reported tuberculosis in the affected population [75]. Even before the earthquake, Haiti had the highest incidence of tuberculosis in the Americas. About half of the tuberculosis cases occur in the Port-au-Prince area. The number of reported tuberculosis cases in Haiti increased after the earthquake, which may be due to an increase in the incidence of tuberculosis and/or improved methods of detecting cases [75].
Compared to previous national estimates (230 per 100,000 population), undiagnosed tuberculosis was three times higher in a shelter with internal displaced people (693 per 100,000) and five times higher in an urban slum (1165 per 100,000) [75]. Early detection of rising tuberculosis rates is a challenge, and data collection should be integrated into realistic disease response programs [75]. From January to June 2013, active tuberculosis was detected among residents of a slum in Port-au-Prince. Of the approximately 7500 residents screened, 394 (5%) had a cough lasting ≥2 weeks and 100 (25%) were diagnosed with active tuberculosis. In total, 144 tuberculosis cases were identified in 6 months (1920/100,000—national estimate 200/100,000) and a high rate of undiagnosed tuberculosis was found in Port-au-Prince even 3 years after the earthquake [76].
Six months after the 2008 Sichuan earthquake, tuberculosis cases recorded in hospitals in the affected Wenchuan region have increased compared to the same period of the previous year. Overall, 88.27% of patients lived in simply constructed temporary shelters in the affected area, among which only 58.06% met adequate sanitary conditions. Poor living conditions, overcrowding, excessive fatigue and stress, treatment interruption, and temporary inability to manage patients resulting from the disaster likely contributed to the worsening of tuberculosis epidemiology [101].
A 14-year-old girl, who was living with her family in a temporary emergency shelter, presented with fever, abdominal pain, and vomiting at a temporary health center in the earthquake-affected city of Bhakatpur in Gorkha (Nepal). Clinical abdominal examination indicated acute peritonitis. On laparotomy, three ileal perforations were identified, and histopathological examination showed cystic granulomas. Combined with the fact that her father had pulmonary tuberculosis with positive sputum, the child was diagnosed with tuberculous peritonitis and responded well to the administered anti-tuberculosis chemotherapy [99].
This entry is adapted from the peer-reviewed paper 10.3390/microorganisms11020419
This entry is offline, you can click here to edit this entry!
