The international community has recognized global warming as an impending catastrophe that poses significant threat to life on earth. In response, the signatories of the Paris Agreement (2015) have committed to limit the increase in global mean temperature to < 1.5 oC, from pre-industry period, which is defined as 1850 - 1890. Considering that the protection of human life is a central focus in the Paris Agreement, the naturally endowed properties of the human body to protect itself from environmental extremes should form the core of an integrated and multifaceted solution against global warming. Scholars believe that heat and thermoregulation play important roles in the evolution of life and continue to be a central mechanism that allow humans to explore, labor and live in extreme conditions. However, the international effort against global warming has focused primarily on protecting the environment and on the reduction of greenhouse gases by changing human behavior, industrial practices, and government policies, with limited consideration given to the nature and design of the human thermoregulatory system. Global warming is projected to challenge the limits of human thermoregulation, which can be enhanced by complementing innate human thermo-plasticity with the appropriate behavioral changes and technological innovations. Therefore, the fundamental concepts and physiology of human thermoregulation should form the underlying bases for human adaptation to global warming and for designing behavioral adaptations and technological innovations to enhance human capacity to function in a warmer environment. A potential behavioral adaptation to global warming is that sleep-wake cycle would gravitate towards a sub-nocturnal pattern, especially for outdoor activities, to avoid the heat of the day. Technologically, the current concept of cooling the space in the room, would likely steer towards targeted body surface cooling. Solar energy is likely to overtake fossil fuel-based energy as the main source of electrical supply globally and more manual labor tasks would need to be replaced by machines and robots to reduce metabolic heat production. There should be more integrated solutions between biologists, behavioral scientists, and technologists, so that man and machine can enhance each other to bring about better solutions against the threat of global warming.
- Thermoregulation
- global warming
- heat
- exercise
- hydration
- fluid
- heat acclimatization
- heat acclimation
- heat stroke
- heat exhaustion
1. Introduction
The ability to sense, respond and adapt to external environmental threats is one of the key attributes that supported the evolution of life, from a single protocell unit to vertebrates, spanning about 500 million years [1]. This innate property of thermo-plasticity, though limited in extent, forms the underlying physiological functions that allow humans to explore, live, socialize, and labor under extremes of environmental temperature (Tev) [2]. Some scholars postulated that heat provided the energy that drove the organization and formation of protocells from polypeptides, which evolved into unicellular and multicellular organisms over time [3][4][5]. Even as life evolved from multicellular organisms into biological organs and systems, the ability to regulate temperature within a physiological range remains a key requirement for survival and daily functions [2]. Although primitive by time of existence, the thermoregulatory system continues to play vital roles in supporting human life and daily functions in present time [6].
Body temperature (Tb) is regulated centrally by the brain to function within a narrow range of about 3–4 °C, from a resting Tb of ≈ 36.8 °C [7][8]. Scholars subscribe to the multi-century consensus that the upper limit for normal Tb is about 40 °C [7][9], but evidence derived from cancer patients [10][11] and endurance runners [12][13][14][15] showed that humans can tolerate a higher core temperature (Tc) of up to 42 °C without any health consequences. Within this Tb range, the thermoregulatory system also exhibits some degree of thermo-plasticity that is capable of semi-permanent adaptation to heat through the process of heat acclimatization (HA) [2][16][17][18] Daily exposure to moderate intensity work under sub-lethal heat stress for up to 14 days enhances the heat dissipation mechanisms to result in lower Tb under the same workload and environmental condition [9][19][20][21][22][23]. These adaptations can be reversed with prolonged absence of heat and exercise exposures [18][24]. Long term passive exposure to warm and humid weather conditions, such as natives in tropical regions, also induces some degree of HA [20][25]. The highly adaptable attributes of Tb regulation has played critical roles in allowing man to survive and function in the heat since the evolution of mankind [1][2][5], but its limits are likely to be challenged by the impending threat of global warming in the near future.
2. Fundamental Concepts and Physiology of Human Thermoregulation
2.1. Definitions and Indicators of Thermoregulation
Tb is the general term used to describe the state of heat storage in the body and mean Tb was defined as the composite of core (Tc, 64%) and skin (Tsk, 37%) temperatures [1][7]. Mean Tsk is estimated from the composite of body-surface temperatures measured at the chest (30%), arm (30%), thigh (20%) and leg (20%) [26]. However, these indicators of Tb are seldom used in thermoregulation research mainly because Tsk is subjected to the influenced of Tev and not Tb alone [7][27][28][29][30]. Tc, on the other hand, is regulated centrally by the brain to respond in a controlled manner to changes in thermal balance (heat production, absorption and dissipation) within the body [1][8]. For more than a century, Tc has been used as the main Tb indicator for diagnosing fever, defining hypothermia and hyperthermia, and for indicating the associated risk of heat and cold injuries [7][29].
2.1.1. Core Temperature
Tc refers to the deep body temperature in the internal environment of the body, i.e., the abdominal, thoracic, and cranial cavities [1][8]. From a measurement perspective, Tc refers to the temperature of venous blood returning to the heart, which stores excess metabolic heat produced in the organs [31][32][33]. The temperature of venous blood and afferent signals from thermo-sensitive nerves on the body surface are used by the brain as reference temperatures for regulating autonomic and behavioral responses around a Tb set-point [8]. As the measurement of venous blood temperature is invasive and impractical to perform in research and clinical settings, the most common sites for indirect measurement of Tc are the rectum, esophagus, and gastrointestinal tract [34][35][36][37] for research, and the axillar, sub-lingual, ear canal, and forehead for diagnosis of fever [7]. In this review, and unless specified, Tc is used generically to encompass temperatures measured in the sites used for research [1][7][38][39].
2.1.2. Heat Tolerance
Heat tolerance was defined as cellular adaptation caused by a single sublethal heat exposure that allows the organism to survive a subsequent exposure to lethal heat stress [40]. This definition of heat tolerance was based on the protective effects of heat shock proteins on cellular structures against lethal heat stress, following a single dose of exposure to sub-lethal heat stress a.k.a. heat shock response. However, the heat shock response was never subjected to human experimentation due to the need for exposure to lethal heat stress. This review takes a “whole-human” approach and defines heat tolerance as the ability to tolerate heat stress without physiological and work failures. Physiological or work failures could range from the inability to sustain workload (i.e., fatigue) to the occurrence of heat illness. Such a definition of heat tolerance is applicable to public health, occupational, and sport settings.
2.1.3. Heat Strain and Heat Stress
Heat strain and heat stress are used interchangeably sometimes to describe a state of positive heat storage in the body, although these are different indexes of thermoregulation. From a physiological perspective, a “strain” refers to a stretch or departure from an original state of existence. Therefore, heat strain is defined as the magnitude of departure from resting Tc, i.e., difference between peak and resting Tc. The physiological concept of “stress,” on the other hand, refers to the sum of physiological demands for an adaptation to maintain homeostasis and to protect the survival of the host [41]. Consistent with this concept, heat stress is defined as the total heat load that the thermoregulatory system has to cope with to maintain physiological homeostasis and is indicated by the peak Tc. For example, if Tc increased from 37 °C to 39.8 °C during a 10-km run, heat strain would be 2.8 °C and heat stress would be 39.8 °C. Therefore, an improvement in heat tolerance would be due mainly to the ability to tolerate a higher level of heat stress and not necessarily due to a higher level of heat strain tolerance.
2.2. The Physical Properties of Heat Transfer and Storage
The net amount of heat stored in the body is a function of the balance between heat gain and loss. This thermal balance is driven the amount of metabolic heat produced, heat exchange between the skin and the environment through conduction convection, and radiation, as well as through evaporative heat loss. Heat transfer between the skin and the environment is bi-directional and down the temperature gradient for conductive, convective and radiation heat exchanges. Heat transfer is
unidirectional for evaporative heat loss, moving from the skin to the environment, and the magnitude of evaporative heat loss is inversely associated with the water vapor pressure in the environment. Metabolic heat production, on the other hand, only adds heat to the body because energy is produced continuously to sustain life. The sum of these channels of heat transfer and production determines the state of thermal balance in the body, which can be expressed in the following equation [6,8]:
Heat Storage = + M +/- Ra +/- Cv +/-Cd - E (1)
where M = metabolic heat production, Ra = radiative heat exchange, Cv = convective heat exchange,
Cd = conductive heat exchange, and E = heat loss due to evaporation.
2.2.1. Metabolic Heat Production
The energy produced in the metabolic process is stored in adenosine triphosphate (ATP). When energy is needed to sustain basal metabolic rate or to perform physical work, one of the phosphate bonds in ATP is split to result in a unit of phosphate and an adenosine diphosphate (ADP). The splitting of the phosphate bond produces about 7.3 Kcal of heat, which is harnessed as energy to drive muscle contraction to produce mechanical work [42]. However, only about 25–30% of metabolic heat produced is used by muscles to perform mechanical work [43][44]. The remaining >70% of metabolic heat is stored in the body with no physiological functions, which explains the increase in body temperature when performing physical work [45][46]. The excess metabolic heat needs to be removed from the muscles to maintain intramuscular thermal balance and to prevent thermolysis of muscle cells. As heat is transferred down the temperature gradient, the excess metabolic heat in the muscle is transferred to the cooler arterial blood flowing into the capillary bed [46] and stored in the venous blood flowing out of the muscle. Heat stored in venous blood is circulated back to the heart and conserved within the body to promote heat storage or transported to the skin surface for dissipation into the environment [47]. Because the metabolic system functions continuously to meet energy demands in the body and heat is a byproduct of metabolism, metabolic heat production is always positive in the heat storage equation, i.e., only adds heat to the body. During intense exercise, metabolic rate can increase acutely by >10-fold [6][46], which is an important attribute for meeting energy demands to increase work output quickly. However, an acute increase in metabolic heat production also puts a strain on the thermoregulatory system to maintain thermal balance [44][48][49]. During prolonged intense physical work, metabolic heat production can outweigh heat removal and Tc can increase to >40 °C, even in cool conditions [15][50][51][52]. The moderation of metabolic heat production and an increase in the rate of heat removal can have significant impact on thermoregulation homeostasis during physical work in hot environment.
2.2.2. Radiative Heat Exchange
Radiative heat exchange refers to the physical transfer of heat between two non-contacting surfaces through the movement of heat in the air. In humans, radiative heat exchange occurs between the skin and the environment and the direction of heat transfer depends on the gradient between Tsk and Tev [6][7]. In the outdoors, the main source of radiative heat is the sun [53], which can be trapped in, as well as reflected from, ground and building surfaces to people in the environment [6][54][55][56]. Heat-producing machineries, such as compressors for air-conditioner, car engines, and power generators, can also be sources of radiative heat transfer from the environment to people in the surrounding. Performing physical work under direct sunlight or near to heat-producing machineries would promote radiative heat transfer from the environment to the skin. On the other hand, the skin can lose heat to the environment through radiation if the Tsk is higher than Tev, such as during exposure to winter conditions or when sitting in a cold room. Exposure to radiative heat from the environment is expected to increase significantly under global warming conditions. Besides behavioral changes, the design of the urban environment can also help to moderate radiative heat exposure from the environment [57][54]. More than half the world population currently live in cities that are classified as urban heat islands (UHI) [58], and global warming is expected to increase the intensity and impact of UHI [59]. UHI refers to the higher Tev in cities than rural areas due to urbanization, and a significant source of UHI is heat radiated from building and road surfaces [60][61]. An increase in vegetation and trees in the environment and changes to the materials used for pavements and buildings can potentially help to reduce the UHI effect by shading the heat emitted from these surfaces [58]. However, the effectiveness of these measures in coping with the full impact of global warming remains unknown currently.
2.2.3. Conductive Heat Exchange
Conductive heat exchange occurs when heat is transferred through contact between two static surfaces [8]. This form of heat exchange is also bi-directional and down the heat gradient, from the warmer to the cooler surface. In occupational settings, conductive heat exchange can occur between the surfaces of heat-emitting equipment and the skin [7], such as communication and electronic equipment carried by soldiers and outdoor workers. In contrast, Conductive heat exchange provides an important channel for rapid removal of body heat when resuscitating heat injury victims using cold-water immersion, because of the acute gradient between Tsk (>37.5 °C) and cold water temperature (~4 °C) [62][63]. During winter, the use of electric thermal blankets conducts heat from the surface of the blanket to the skin to maintain Tb at a comfort zone. The same concept of the thermal blanket may be used for reverse application in the context of global warming, by installing cooling mechanisms in sofas, beds, blankets, and mattresses to keep the body cool through conductive heat transfer (discussed later). This approach to body cooling would be more efficient than the current air conditioning (AC) systems, which emit heat and carbon to environment and may not be sustainable under global warming conditions [64][65][66].
2.3. The Physiology of Thermoregulation and Adaptation
The physical attributes of heat transfer inform us on the channels of heat transfer between the body and the external environment. The next section will explain the mechanisms regulating the body’s responses and adaptations to heat in both the acute and chronic timeframes.
Central Regulation of Body Temperature
Humans are both endotherms and homeotherms by nature. The endothermic property refers to the ability to produce heat endogenously (heat gain) through the metabolic pathway and the homeothermic property refers to the innate regulation of heat gain and loss to maintain homeostasis of Tb. The endothermic property acts in concert with the physical channels of heat transfer (heat absorption or loss), and as part of the homeothermic processes, to achieve homeostasis of Tb [1]. Both the endothermic and homeothermic functions are coordinated centrally through a Tc set-point by a “thermostat” mechanism in the hypothalamus, which is part of the limbic system in the brain [1][8][67][68] (Figure 1). The limbic system regulates emotions and motivation, which drives behavior to avoid pain and to seek reward. The hypothalamus is part of the limbic system and serves as common point of consolidation for efferent outputs to preserve physiological homeostasis through autonomic regulation [67][69][70]. The central thermostat receives afferent feedback on Tev from thermal-sensitive nerves distributed all over the surface of the body (i.e., Tsk), and feedback on Tc from blood flowing to the brain [71]. This feedback mechanism demonstrates the dual-thermic property of human thermoregulation, which comprises the shell (Tsk) and the core (Tc) [1]. Signals from Tsk and Tc are integrated and matched against a Tc set-point that is regulated centrally in the brain [8].
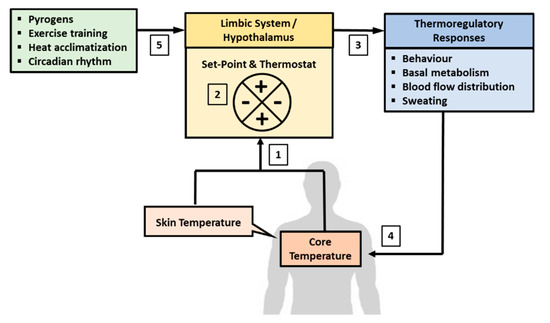
Figure 1. Central regulation of body temperature. Body temperature is regulated autonomously in the limbic system, which includes the hypothalamus. (1) The brain receives afferent signals on the state of body temperature from core (Tc) and skin (Tsk) temperatures. Tc is sensed from temperature of blood flowing to the brain and Tsk is derived from thermal sensitive nerves distribute all over the surface of the body. (2) The signals from Tsk and Tc are matched against the temperature set-point, which is about 36.8 °C in resting condition. (3) A departure from the set-point would activate a “thermostat” response through the autonomic nervous system to recalibrate body temperature back to the set-point. (4) The recalibration of body temperature may involve changes in behavior, blood flow distribution, basal metabolic rate adjustments, and the induction of sweating if heat loss is needed. (5) The temperature set-point can also fluctuate due to the influence of circadian rhythm, adaption to physical training, heat acclimatization, and pyrogens.
3. Conclusions
The impending threat of global warming will have significant impact on human life and would demand significant adjustments at the social, personal, industrial, and government levels to reduce carbon footprint in the next 10–20 years. The search for novel solutions to protect the environment from global warming needs to consider both the physical and physiological bases for human thermoregulation. The key concepts of human thermoregulation should form the bases for exploiting the potential of thermal plasticity to protect human life and functions in the context of global warming. For example, the benefits of hydration strategies, HA and physical fitness to enhance thermoregulation in the heat should be further exploited and implemented systematically to optimize the innate mechanisms of heat tolerance in education, sport, and occupation settings.
The innate capacity for heat dissipation, though limited, would serve as the foundation strategy to cope with elevated Tev. Other strategies involving behavioral adaptations and technological innovations can be designed around the human thermoregulatory system, to provide a holistic approach in protecting human life and functions from the impact of global warming. For example, the physical properties of heat transfer would be important considerations in the design of clothing materials to promote heat removal and the development of body cooling devices. Data on the metabolic demands of occupational tasks would also be valuable for guiding innovations on mechanization of physical labor. The combination of these human-centered innovations with behavioral adaptations would have great potential in delivering solutions to protect human survival and functions as the world faces an increasing GMT. This review serves to draw the attention of the global warming conversation to include the human and its physiology as part of the wider effort to protect the earth from the effects of global warming. There should be more integrated solutions between biologists and technologists, so that man and machine can enhance each other to bring about better solutions against the threat of global warming. Going back to the basics of appreciating the thermoregulatory system may serve as the foundation needed for future solution and human survival in a hotter environment.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17217795
References
- Gisolfi, C.V.; Mora, F. The Hot Brain: Survival, Temperature and the Human Body; MIT Press: Cambridge, MA, USA, 2000; pp. 1–20, 94–119, 157–163, 171–174, 191–215.
- Folk, E.G.; Riedesel, M.L.; Thrift, D.L. Principles of Integritive Environmental Physiology; Austin and Winfield Publishers: Bethesda, MD, USA, 1998.
- Fox, S.W.; Dose, K. Molecular Evolution and the Origins of Life; Freeman: San Francisco, CA, USA, 1972.
- Muller, A.W. Were the first organisms heat engines? A new model for biogenesis and the early evolution of biological energy conversion. Prog. Biophys. Mol. Biol. 1995, 63, 193–231.
- Van Holde, K.E. The Origins of Life; Alan R. Liss: New York, NY, USA, 1980.
- Haymes, E.M.; Wells, C.L. Environment and Human Performance; Human Kinetics Publishers: Champaign, IL, USA, 1986; pp. 1–10.
- Lim, C.L.; Byrne, C.; Lee, J. Human thermoregulation and measurement of body temperature in exercise and clinical settings. Ann. Acad. Med. Singap. 2008, 37, 347–353.
- Stitt, J. Central regulation of body temperature. In Perspectives in Exercise Science and Sports Medicine; Gisolfi, C.V., Lamb, D.R., Nadel, E.R., Eds.; Cooper Publishing Group: Traverse, IN, USA, 1993; Volume 6, pp. 2–39.
- Gisolfi, C.V.; Robinson, S. Relations between physical training, acclimatization, and heat tolerance. J. Appl. Physiol. 1969, 26, 530–534.
- Pettigrew, R.T.; Galt, J.M.; Ludgate, C.M.; Horn, D.B.; Smith, A.N. Circulatory and biochemic al effects of whole body hyperthermia. Br. J. Surg. 1974, 61, 727–730.
- Bynum, G.D.; Pandolf, K.B.; Schuette, W.H.; Goldman, R.F.; Lees, D.E.; Whang-Peng, J.; Atkinson, E.R.; Bull, J.M. Induced hyperthermia in sedated humans and the concept of critical thermal maximum. Am. J. Physiol. 1978, 235, R228–R236.
- Byrne, C.; Lee, J.; Chew, S.A.N.; Lim, C.L.; Tan, Y.M. Continuous thermoregulatory responses to mass-participation distance running in heat. Med. Sci. Sports Exerc. 2006, 38, 803–810.
- Lee, J.K.W.; Nio, A.Q.X.; Lim, C.L.; Teo, Y.N.E.; Byrne, C. Thermoregulation, pacing and fluid balance during mass participation distance running in a warm and humid environment. Eur. J. Appl. Physiol. 2010, 109, 887–898.
- Pugh, L.G.C.E.; Corbett, J.L.; Johnson, R.H. Rectal temperatures, weight losses and sweat rates in marathon running. J. Appl. Physiol. 1967, 23, 347–352.
- Racinais, S.; Moussay, S.; Nichols, D.; Travers, G.; Belfekih, T.; Schumacher, Y.O.; Periard, J.D. Core temperature up to 41.5 °C during UCI road cycling world championships in the heat. Br. J. Sports Med. 2019, 53, 426–429.
- Aoyagi, Y.; McLellan, T.M.; Shephard, R.J. Effects of 6 versus 12 days of heat acclimation on heat tolerance in lightly exercising men wearing protective clothing. Eur. J. Appl. Physiol. 1995, 71, 187–196.
- Wyndham, C.H. The physiology of exercise under heat stress. Ann. Rev. Physiol. 1973, 35, 193–220.
- Hein, A.; Daanen, M.; Racinais, S.; Periard, J.D. Heat acclimation decay and re-induction: A systematic review and meta analysis. Sports Med. 2018, 48, 409–430.
- Brearley, M.B. Pre-deployment Heat Acclimatization Guidelines for Disaster Responders. Prehosp. Disaster. Med. 2016, 31, 85–89.
- Hanna, E.G.; Tait, P.W. Limitations to Thermoregulation and Acclimatization Challenge Human Adaptation to Global Warming. Int. J. Environ. Res. Public Health 2015, 12, 8034–8074.
- Aoyagi, Y.; McLellan, T.M.; Shephard, R.J. Effects of training and acclimation on heat tolerance in exercising men wearing protective clothing. Eur. J. Appl. Physiol. 1994, 68, 234–245.
- Aoyagi, Y.; McLellan, T.M.; Shephard, R.J. Interaction of physical training and heat acclimation. Sports Med. 1997, 23, 173–210.
- Nadel, E.R.; Pandolf, K.B.; Roberts, M.F.; Stolwijk, J.A.J. Mechanisms of thermal acclimation to exercise and heat. J. Appl. Physiol. 1974, 37, 515–520.
- Armstrong, L.E.; Maresh, C.M. The induction and decay of heat acclimatisation in trained athletes. Sports Med. 1991, 12, 302–312.
- Lim, C.L.; Ng, K.K.C.; Lee, L.K.H. The effects of prolonged passive heat exposure and Basic Military Training on thermoregulatory and cardiovascular responses in recruits from a tropical country. Mil. Med. 1997, 162, 623–627.
- Ramanathan, N.L. A new weighting system for mean surface temperature of the human body. J. Appl. Physiol. 1964, 19, 531–533.
- Eggenberger, P.; MacRae, B.A.; Kemp, S.; Burgisser, M.; Rossi, R.M.; Annaheim, S. Prediction of core body temperature based on skin temperature, heat flux, and heart rate under different exercise and clothing conditions in the heat in young adult males. Front. Physiol. 2018, 9, 1780.
- Te Lindert, B.H.W.; Van Someren, E.J.W. Skin temperature, sleep, and vigilance. Handb. Clin. Neurol. 2018, 156, 353–365.
- Chen, W. Thermometry and interpretation of body temperature. Biomed. Eng. Lett. 2019, 9, 3–17.
- Childs, C. Body temperature and clinical thermometry. Handb. Clin. Neurol. 2018, 157, 467–482.
- Rupp, M.E.; Heermann, J.; Uphoff, M.E. Need for a reliable system to measure body temperature. Am. J. Infect. Control 2004, 32, 184.
- Farnell, S.; Maxwell, L.; Tan, S.; Rhodes, A. Temperature measurement: Comparison of non-invasive methods used in adult critical care. J. Clin. Nurs. 2005, 14, 632–639.
- El Radhi, A.S.; Barry, W. Thermometry in paediatric practice. Arch. Dis. Child. 2006, 91, 351–356.
- Mundel, T.; Carter, J.M.; Wilkinson, D.M.; Jones, D.A. A comparison of rectal, oesophageal and gastro-intestinal tract temperatures during moderate-intensity cycling in temperate and hot conditions. Clin. Physiol. Funct. Imaging 2016, 36, 11–16.
- Miller, K.C.; Hughes, L.E.; Long, B.C.; Adams, W.M.; Casa, D.J. Validity ofcore temperature measurements at 3 rectal depths during rest, exercise, cold-water immersion, and recovery. J. Athl. Train. 2017, 52, 332–338.
- Vardasca, R.; Magalhaes, C.; Marques, D.; Moreira, J.; Frade, R.A.; Seixas, A.; Mendes, J.G.; Ring, F. Bilateral assessment of body core temperature through axillar, tympanic and inner canthi thermometers in a young population. Physiol. Meas. 2019.
- Yeoh, W.K.; Lee, J.K.W.; Lim, H.Y.; Gan, C.W.; Liang, W.; Tan, K.K. Re-visiting the tympanic membrane vicinity as core body temperature measurement site. PLoS ONE 2017.
- Lim, C.L. Look beyond thermoregulatyion and hydration in the diagnosis of heat stroke. Med. Sci. Sports Exerc. 2016, 48, 2583.
- Byrne, C.; Lim, C.L. The ingestible telemetric body core temperature sensor: A review of validity and exercise applications. Br. J. Sports Med. 2007, 41, 126–133.
- Moseley, P.L. Heat shock proteins and heat adaptation of the whole organism. J. Appl. Physiol. 1997, 83, 1413–1417.
- Selye, H. Forty years of stress research: Principal remaining problems and misconceptions. Can. Med. Assoc. J. 1976, 115, 53–56.
- Brooks, G.A.; Fahey, T.D.; White, T.P. Exercise Physiology: Human Bioenergetics and its Applications, 2nd ed.; Mayfield Publishing Company: California, CA, USA, 1996; p. 504.
- Knochel, J.P.; Dotin, L.N.; Hamburger, R.C. Heat stress, exercise, and muscle: Effects on urate metabolism an drenal function. Am. J. Intern Med. 1974, 81, 321–328.
- Dube, P.A.; Imbeau, D.; Dubeau, D.; Auger, I. Worker heat stress prevention and work metabolism estimation: Comparing two assessment methods of the heart rate thermal component. Ergonomics 2019, 62, 1066–1085.
- Yu, F.C.; Lu, K.C.; Lin, S.H.; Chen, G.S.; Chu, P.; Gao, G.W.; Lin, Y.F. Energy metabolism in exertional heat stroke with acute renal failure. Nephrol. Dial. Transplant 1997, 12, 2087–2092.
- Febbraio, M.A. Alterations in energy metabolism during exercise and heat stress. Sports Med. 2001, 31, 47–59.
- Nadel, E.R.; Mack, G.W.; Nose, H.; Tripathi, A. Tolerance to severe heat and exercise: Peropheral vascular responses to body fluid changes. In Heat Stress: Physical Exertion and Environment; Hales, R.J.S., Richards, D.A.B., Eds.; Elsevier Science Publisher: Amsterdam, The Netherlands, 1987; pp. 117–131.
- Sawka, M.N. Human tolerance and heat strain during exercise: Influence of hydration. J. Appl. Physiol. 1992, 73, 368–375.
- Coggan, A.R.; Coyle, E.F. Carbohydrate ingestion during prolonged exercise: Effects on metabolism and performance. Exerc. Sport Sci. Rev. 1991, 19, 1–40.
- Costill, D.L.; Kammer, W.F.; Fisher, A. Fluid ingestion during distance running. Arch. Environ. Health 1970, 21, 520–525.
- Yeh, Y.J.; Law, L.Y.L.; Lim, C.L. Gastrointestinal response and endotoxemia during intense exercise in hot and cool environments. Eur. J. Appl. Physiol. 2013, 113, 1575–1583.
- American College of Sports Medicine, Position stand: Heat and cold illnesses during distance running. Med. Sci. Sports Exerc. 1996, 28, i–x.
- Otani, H.; Goto, T.; Goto, H.; Shirato, M. Time-of-day effects of exposure to solar radiation on thermoregulation during outdoor exercise in the heat. Chronobiol. Int. 2017, 34, 1224–1238.
- Taylor, J.; Wilkinson, P.; Picetti, R.; Symonda, P.; Heaviside, C.; Macintyre, H.; Davies, M.; Mavrogianni, A.; Hutchinson, E. Comparison of built environment adaptations to heat exposure and mortality during hot weather, West Midlands region, UK. Environ. Int. 2017, 111, 287–294.
- Werner, J. Temperature Regulation during Exercise: An Overview; Cooper Publishing Group: Michigan, IN, USA, 1993; Volume 6, pp. 49–79.
- Zamanian, Z.; Sedaghat, Z.; Hemehrezaee, M.; Khajehnasiri, F. Evaluation of environmental heat stress on physiological parameters. J. Environ. Health Sci. Eng. 2017, 15, 24.
- Tait, P.W.; Hannah, E.G. A conceptual framework for planning systemic human adaptation to global warming. Int. J. Environ. Res. Public Health 2015, 12, 10700–10722.
- Li, D.; Liao, W.; Rigden, A.J.; Liu, X.; Wang, D.; Malyshev, S.; Shevliakova, E. Urban heat island: Aerodynamics or imperviousness? Sci. Adv. 2019, 5, eeau4299.
- Masson, V.; Bonhomme, M.; Salagnac, J.L.; Briottet, X.; Lemonsu, A. Solar panels reduce both global warming and urban heat island. Front. Environ. Sci. 2014, 2.
- Sharma, R.; Hooyberghs, H.; Lauwaet, D.; De Ridder, K. Urban heat island and future climate change—Implications for Delhi’s heat. J. Urban Health 2019, 96, 235–251.
- Scott, A.A.; Waugh, D.W.; Zaitchik, B.F. Reduced Urban Heat Island intensity under warmer conditions. Environ. Res. Lett. 2018, 13, 064003.
- Costrini, A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med. Sci. Sports Exerc. 1990, 22, 15–18.
- Armstrong, L.E.; Crago, A.E.; Adams, R.; Roberts, W.O.; Maresh, C.M. Whole-body cooling of hyperthermic runners: Comparison of two field therapies. Am. J. Emerg. Med. 1996, 14, 355–358.
- Gao, C.; Kuklane, K.; Östergren, P.O.; Kjellstrom, T. Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 2018, 62, 359–371.
- Davis, L.W.; Gertlera, P.J. Contribution of air conditioning adoption to future energy use under global warming. Proc. Natl. Acad. Sci. USA 2015, 112, 5962–5967.
- Kownacki, K.L.; Hornyanszky, E.D.; Chu, T.A.; Olsson, J.A.; Becker, P. Challenges of using air conditioning in an increasingly hot climate. Int. J. Biometeorol. 2018, 62, 401–412.
- Madden, C.J.; Morrison, S.F. Central nervous system circuits that control body temperature. Neurosci. Lett. 2019, 696, 225–232.
- Zalewski, P.; Bitner, A.; Slomko, J.; Szrajda, J.; Klawe, J.J.; Tafil-Klawe, M.; Newton, J.L. Whole-body cryostimulation increases parasympathetic outflow and decreases core body temperature. J. Therm. Biol. 2014, 45, 75–80.
- Hissa, R. Central control of body temperature. Arct. Med. Res. 1990, 49, 315.
- Morrison, S.F.; Nakamura, K. Central Mechanisms for Thermoregulation. Annu. Rev. Physiol. 2019, 81, 285–308.
- Tansey, E.A.; Johnson, C.D. Recent advances in thermoregulation. Adv. Physiol. Educ. 2015, 39, 139–148.
