Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Lung cancer remains the first cause of cancer worldwide. The main reason for this high rate of death from lung cancer is dissemination of the disease at the time of presentation to hospital due to late diagnosis. There is an urgent need to identify and validate non-invasive biomarkers for the early diagnosis, prognosis, and treatment of lung cancer for improved patient management.
- lung cancer
- biomarkers
- early detection
- screening
- microRNAs
- circulating tumour DNA
1. DNA Methylation in Sputum and Plasma for Early LC Detection
As epigenetic changes in LC are common, this offers several targets that can concurrently be probed [1]. LC genome analysis reports global hypomethylation that results in the destabilisation of DNA with the exception of CpG dense regions [2][3][4]. In NSCLC, epigenetic changes are associated with cigarette smoking and aggressive tumour behaviour, and as such these changes can be used for risk stratification and histological and molecular characterisation [5][6][7][8][9][10][11][12]. Non-invasive, sputum-based epigenetic testing for the detection of epigenetic changes/promoter DNA hypermethylation at early stages of tumorigenesis is well documented. Palmisano et al. showed that in sputum samples, collected 3 years prior to clinically detectable lung cancer, the hypermethylation of MGMT and/or CDKN2A genes could be effectively detected, indicating that epigenetic markers can indeed play a role in early cancer diagnosis [13]. This was validated in other studies as well [14][15][16]. Moreover, in a study of five participants, RASSF1A methylation, detected in sputum samples, correlated with the development of LCs within 12 to 14 months from the sputum test in three patients [17]. Similarly, a prospective study on 92 high risk individuals and a matched control group identified promoter methylation of 14 genes in the sputum that can be used for risk stratification. It was found that 6 of 14 genes correlated with a >50% increased LC risk. Furthermore, simultaneous methylation of three or more of these six genes correlated with 6.5-fold increased risk of LC [18]. These detected genes are involved in many important biological functions, such as cell cycle regulation (p16 and PAX5 β), apoptosis (DAPK and RASSF1A), signal transduction (GATA5), and DNA repair (MGMT) [18][19][20][21][22].
The detection of DNA methylation in plasma, as a tool for screening and diagnostic purposes in LC, has also shown promise. Bearzatto et al. reported an increased frequency in p16INK4A methylation in plasma samples of early-stage adenocarcinoma [23]. Similarly, methylations of RASSF1A and CDKN2A detected in blood samples were frequently identified in early-stage LC with a reported sensitivity of 22 to 66% and specificity of 57–100% [23][24][25]. Another study on 70 participants showed significant differences in the methylation pattern between LC and benign lung lesions. The participants who developed lung cancer showed methylation changes in four tumour suppressor genes, i.e., Kif1a, DCC, RARB, and NISCH. The differences were correlated with LC diagnosis, and it was observed that participants who were finally diagnosed with LC exhibited significant differences in methylation pattern [26]. Another, larger study on 360 participants showed similar results. The methylation status of PTGER4 and SHOX2 genes detected in the plasma of patients with indeterminate pulmonary nodules was distinct as compared to participants with benign lung nodules [27]. Therefore, integrating DNA methylation expression patterns (in plasma/sputum) as a screening tool in national LC screening programs is now needed to progress to novel algorithms for early LC detection. In lieu of this, Kang et al. developed a probabilistic method called Cancer Locator, based on cfDNA detected in blood samples. The study utilized data from a genome-wide DNA methylation profile and DNA methylation microarrays of solid tumour samples to train the model. The model was able to identify the histological type and the site of the tumour together with cancer load in NSCLC [28]. The study could not offer firm conclusions because of small sample numbers; however, the authors foresaw that when more paired samples (tumour sample and the matched adjacent non-tumour sample) become available, Cancer Locator could identify not just the existence but also the location of the tumour [28].
2. The Role of microRNAs in LC Detection
miRNAs are small non-coding RNAs of 18–25 nucleotides in length which are involved in the post-transcriptional regulation of gene expression [29][30]. They are found to be aberrantly expressed in many pathological conditions, including cancer, and can be detected in bodily fluids including urine, sputum, and blood, making them exciting biomarkers for cancer detection [31][32]. In 2002, their role in LC pathogenesis (proliferation of LC cells, invasion of basement membrane, and metastasis) was reported by Calin et al. [33]. Interestingly, based on the cellular context, miRNAs can act as tumour suppressors or oncogenes and even both [34][35]. Moreover, miRNAs preserve their stability throughout cancer progression from initiation to metastasis, because they are too small to degrade, and some miRNAs are further protected in exosomes. Hence, miRNAs are considered an appealing biomarker for cancer diagnosis and monitoring [36].
Another non-coding RNA type, circRNAs, which have a stable covalently closed circular structure and show a specific expression pattern in different tissues and cells, have also been implicated in LC growth and progression [37]. However, the exact mechanisms remain poorly understood and require more in-depth studies [38]. Using technologies such as RNA-seq and Ribo-Zero, thousands of circRNAs have been discovered ([37], and it is predicted that valid circRNA biomarkers for diagnosis, prognosis, and therapy in LC will increasingly be found. A better understanding of the exact role of circRNAs in the pathogenesis of LC will likely also lead to improvement of the detection of “clinically significant” circRNAs and understanding of the temporal relationship between such circRNAs and the development of preinvasive or early LC.
3. The Role of Circulating Tumour DNA (ctDNA) in LC
ctDNA (circulating tumour DNA) includes both encapsulated (in circulating vesicles) and non-encapsulated free DNA in the blood or other body fluids [39]. ctDNA escapes cancer cells via several mechanisms, namely apoptosis, necrosis, and secretion from extracellular vesicles as well as from CTCs [40][41]. Therefore, analysing ctDNA is a promising approach that could accelerate efforts for body fluid-based LC detection and overcome some of the challenges posed by invasive tissue biopsy, as summarised in Table 1.
Table 1. Important differences between LB (analysis of ctDNA) and tissue biopsy.
| Analysis of ctDNA | Tissue Biopsy | |
|---|---|---|
| Accessibility and convenience | Blood (and other body fluids)-based tests. This makes it more accessible for sample collection and acceptable by patients. | Invasive and often requires exposure to radiation. |
| Factors affecting SN and SP | ctDNA levels are also influenced by disease burden and many other factors such as tumour location, vascularity, and cellular turnover [42][43]. | Accessibility of the tumour, patient’s fitness and personal preference, tumour heterogeneity. |
| The effect of tumour type on the detection of ctDNA in blood and other body fluids | Tumours in the central nervous system or those with mucinous features (such as prostate and thyroid) frequently show low or undetectable ctDNA levels [44][45]. | Not applicable. |
| Cost effectiveness | More cost-effective and time-efficient than tissue biopsy [46]. | The cost could soar, especially if biopsy from difficult location requires operation, e.g., surgical brain biopsy. |
| Histological diagnosis | Provides no information regarding histology. | Is required to make a histological diagnosis. |
| Monitoring disease progression and response to treatment | Has an established role in treatment response monitoring or the early detection of relapse [47][48]. | Not always possible or practical due to its invasive nature. |
| As a screening biomarker | Can be used for population-based screening [49]. | Not possible or practical due to its invasive nature. |
| Detection of minimal residual disease (MRD) | The role in detecting MRD after curative treatment is growing. | Not applicable. |
| The effect of the location of metastasis on the accuracy of the result | The SN of analysis of ctDNA to detect EGFR mutation in the setting of NSCLC is greater in intrathoracic compared to extra-thoracic located tumours [50]. | Not applicable. |
An important feature of ctDNA is that it can be found in blood prior to clinical diagnosis [51]. Advances in technologies of DNA sequencing made it possible to detect cDNA before clinically evident LC [52]. However, a major challenge in using ctDNA is that most patients have ctDNA levels of less than 0.1% [53][54]. Nonetheless, new techniques have continuously been developed and tested to improve the detection of ctDNA in low concentrations in plasma. There is also evidence of a positive correlation between disease burden and the plasma concentration of ctDNA [52]. A study by Jacob et al. [51] used deep sequencing (CAPP-Seq) and improved protocol for the extraction of unique cfDNA fragments and the segment of cfDNA duplexes for sequencing of both strands [51]. The authors genotyped tumour tissue, analysed pre-treatment cfDNA in plasma and leukocyte DNA from 85 subjects diagnosed with stage I–III NSCLC using targeted deep sequencing of 255 frequently mutated genes in NSCLC, and reported that most somatic mutations in the cfDNA of LC patients and of risk-matched cohorts replicate clonal haematopoiesis and are not recurring. In contrast with mutation driving carcinogens, clonal haematopoiesis mutations are present on longer cfDNA fragments and do not show mutational marks that correlate with tobacco smoking. Incorporating these results with other tumour characteristics such as cell proliferation and lymphovascular invasion, the authors applied and prospectively validated a machine-learning-based method called “LC likelihood in plasma” (Lung-CLiP) [53]. Three control groups were used as a validation cohort: a low-risk group of 42 adult blood donors, a matched risk control group of 56 age, sex, and smoking status matched adults who had negative low-dose CT (LDCT) screening scans, and a third group comprising 48 risk-matched participants receiving LDCT screening recruited prospectively at a different centre.
One of the key shortcomings of molecular analysis by studying ctDNA is that it provides no information on histology; therefore, invasive biopsy will be required to make a histological diagnosis of LC. False-negative results from analysing ctDNA is a further important issue in the context of low tumour load or low rate of shedding of ctDNA to the systemic circulation [55]. Moreover, the precision of the data acquired by analysing ctDNA is affected by the location of the metastatic disease. A pooled analysis of EGFR-mutated NSCLC revealed that the detection rate of ctDNA EGFR mutation was considerably higher in patients with extrathoracic compared to intrathoracic lesions [50]. Furthermore, the false-positive results can be acquired using ctDNA as mentioned above (molecular alterations originated by clonal haematopoiesis rather than the tumour) [56]. Identification of unintended germline mutations during ctDNA evaluation that are not linked to the pathogenesis of LC is not an infrequent occurrence that mandates disclosure to the patient and referral for genetic counselling clinics [57]. For example, in the molecular analysis using ctDNA of 10,888 unselected patients with metastatic cancer (41% were lung malignancies), 1.4% were discovered to have possible hereditary cancer mutations in 11 genes [57]. Finally, technical aspects in relation to ctDNA specimen acquisition and handling can affect the quality of the data. Despite the many advantages of LBs compared to tissue biopsies, the SN and SP of detecting specific molecular changes in NSCLC from LB remain affected by technology, clinical trial methodologies, and logistics, which in turn affect the safe and effective integration of LB into clinical practice [58]. In a first published systematic review of 34 studies involving 1141 patients with NSCLC by Esagian et al., the positive percent agreement (PPA) in detecting common mutations using targeted NGS between LB and tissue biopsy was provided [59]. The authors stated that they used PPA rather than SN, SP, and PPV and NPV because NGS was not validated in all the studies they reviewed, and hence PPA was deemed more appropriate. The calculated PPA rates were 53.6% (45/84) for ALK, 53.9% (14/26) for BRAF, 56.5% (13/23) for ERBB2, 67.8% (428/631) for EGFR, 64.2% (122/190) for KRAS, 58.6% (17/29) for MET, 54.6% (12/22) for RET, and 53.3% (8/15) for ROS1. The above findings are consistent with other publications that concluded that the detection of specific mutations via NGS from LB is less sensitive compared to tissue biopsy [60][61].
4. Urine Cell-Free DNA (ucfDNA) in the Diagnosis of LC
Improvements in the knowledge and the technologies for the isolation and analysis of biomarkers from urine provide novel opportunities for the clinical applications of cancer urine biomarkers. The presence of biomarkers such as exfoliated bladder cancer cells, ctDNA, proteins, miRNAs, and exosomes in the urine have been investigated in the context of different primary cancers such as bladder, prostate, pancreas, and lung; the cost-effectiveness and convenience of use make urine biomarkers attractive choices for patients and physicians alike [62][63][64][65]. Using urine biomarkers for assessing treatment efficacy and resistance is a major advantage when compared to tissue biopsies and radiological imaging [66]. Furthermore, another advantage of urine biomarker analysis is that cfDNA extraction is technologically easier [66][67][68], when compared with plasma, as urine contains a lower concentration of interfering proteins [69]. The evidence for the reliability and sensitivity of the detection of gene mutations and DNA methylation in the urine is growing, especially as the technologies used are consistently undergoing refinement [70][71][72].
Methods associated with the extraction and classification of urinary constituents are multifarious and diverse and can vary from methods for protein and genomic profiling to microfluidic techniques [73]. In recent years, the detection of EGFR mutation and the subsequent mutation profile in patients with metastatic NSCLC who might be eligible to receive first and second lines of anti-EGFR tyrosine kinase inhibitors (TKIs) has grown rapidly. A study by Reckamp et al. showed that EGFR mutations (T790M, L858R, and exon 19 deletions) were successfully identified in the urine of NSCLC patients and the results were congruent with the EGFR mutation state identified through tissue biopsy [74]. A comparative study was reported by Ren et al., who measured the concentration of ucfDNA, using qPCR, in 55 LC patients and a cohort of 35 healthy participants [75]. The study reported that the concentration of ucfDNA is consistently higher in LC patients, especially with lymph node involvement, compared to the healthy cohort, suggesting that ucfDNA could potentially play a role in the early diagnosis of LC [75]. Another study compared the urine cell-free DNA (ucfDNA) of 55 NSCLC patients of different disease stages with 35 healthy volunteers by means of quantitative real-time PCR (qPCR) [76]. The study showed that concentrations of urinary cell-free DNA (ucfDNA) were considerably greater in individuals with stage III/IV than in those with stage I/II and the disease-free cohort. The receiver operating characteristic curves (ROCs) for distinguishing participants with stage III/IV from disease-free volunteers showed areas under the curve (AUCs) of 0.84 and 0.88, respectively. In another study [75], ucfDNA concentration and integrity indexes were explored as biomarkers for early LC detection. The cohort included 55 LC patients and 35 healthy participants. The study found that concentration and integrity indexes of ucfDNA were considerably higher in LC patients compared to the healthy individuals. Moreover, the ucfDNA integrity indexes in patients with metastasis to lymph nodes were significantly higher compared with patients without lymph node involvement, suggesting that ucfDNA could potentially play a role in the early diagnosis of LC [75].
5. RNA Airway and Nasal Signature
The approach of analysis of RNA acquired from airway samples centres on gene expression profiles of cancer-associated processes affecting the tracheobronchial tree [77]. A study identified a 23-gene biomarker panel from endobronchial brushings of patient who received bronchoscopy to investigate LC [78]. Consequently, two separate prospective cohorts showed an SN of 88% to 89% and an SP of 48% for such a gene-expression classifier. As biomarkers, these 23 genes were especially indicative of possible underlying cancer in patients with an intermediate (10–60%) pre-test risk of LC (91% negative predictive value, NPV). These results suggest that the NPV of a negative bronchoscopy could be improved if combined with the 23-gene panel, which could potentially circumvent the need for invasive lung biopsy by monitoring such patients with less invasive tests such as follow up CT scans [79].
6. Radiomics Signatures of Primary and Secondary Pulmonary Malignant Lesions
In the past decade, medical imaging has progressed from chiefly being a primary diagnostic tool to acquiring an important role in providing vital molecular data required for targeted based therapy through the adoption of advanced hardware, novel imaging agents, streamlined scanning protocols, and improvements in computational power [80]; thus, the researchers will briefly discuss its role here. The technological advances have enabled the extraction and processing of a large amount of data from quantitative imaging, in a process called radiomics [80]. By utilising a characterisation algorithm, radiomics has the potential to unveil disease features that cannot be seen by the naked eye [81]. The process of radiomics involves obtaining sub-visual, yet quantitative, image characteristics in order to produce usable datasets from radiological films [82]. Radiomics data extracted from medical scans (e.g., CT and MRI scans) can be utilised to discover diagnostic, predictive, and prognostic data in patients with malignancy through comparison with objective response criteria such as overall and progression-free survival, and can also be combined with tumour molecular and genetic profile (genotype); the latter is referred to as radiogenomics [83]. The process of converting medical imaging into meaningful data typically involves four steps: (a) image acquisition and reconstruction, (b) region of interest segmentation, (c) feature extraction and quantification, and (d) building predictive and prognostic models, as illustrated in Figure 1.
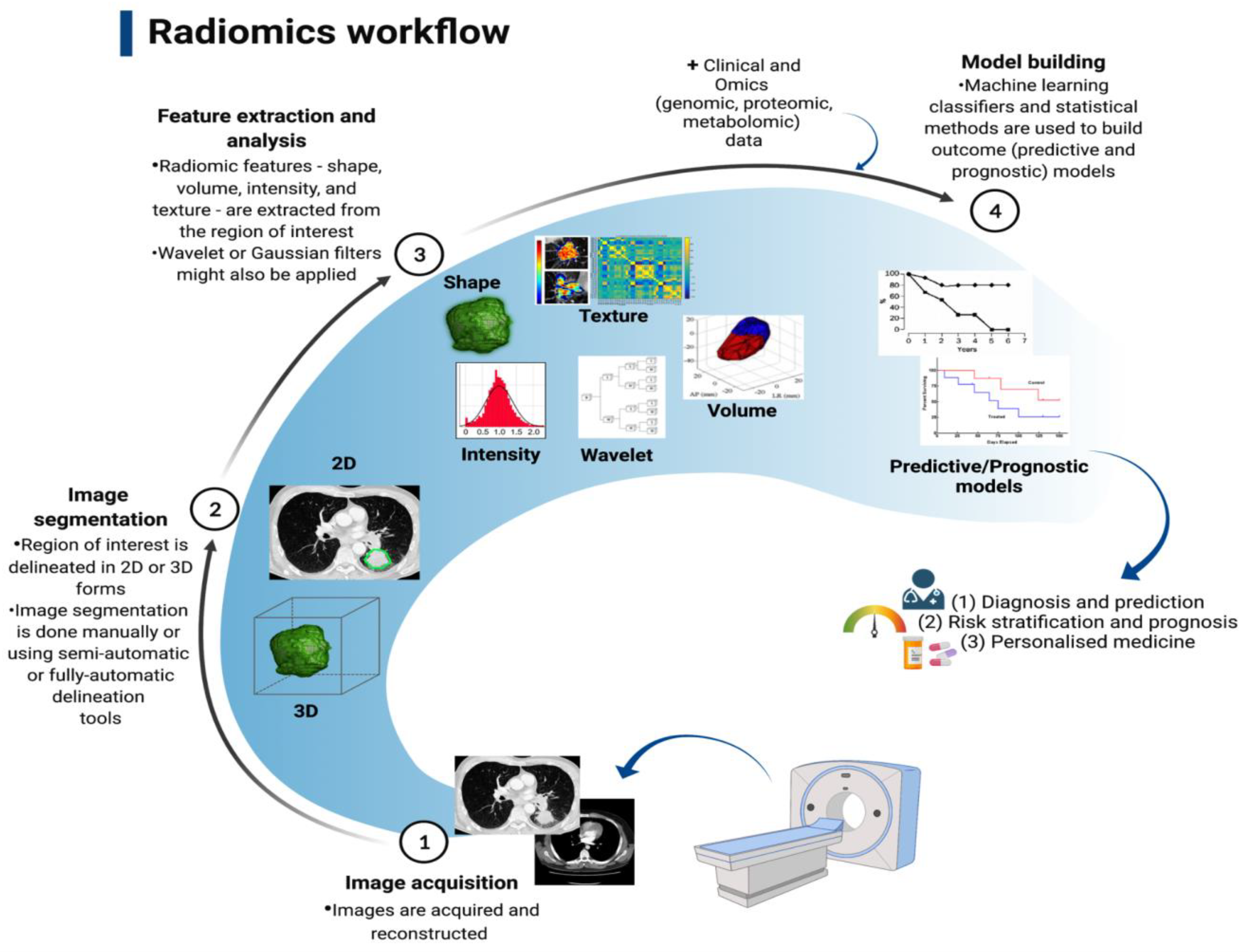
Figure 1. Radiomics workflow that involved four stages, Lambin et al. [81].
As a new technology, radiomics is in its infancy; therefore, its clinical application is still limited. In the context of primary LC, a significant interest in using radiomics to predict the histological and molecular characteristics, response to treatment, and overall prognosis is raised. Several studies have been able to identify specific radiomics signatures that differentiate NSCLC from other benign and pre-invasive lesions, including the prediction of EGFR status and response to treatment with TKI [84][85][86][87][88][89][90][91], as well as histological subtype. For example, a retrospective study of 148 patients with histologically confirmed NSCLC found thirteen radiomics features that predict histological subtype (ALC vs. SqCLC) with AUCs of 0.819 and 0.824, respectively [92]. Several studies of radiomics signatures have reported features distinguishing benign from cancerous lung pathologies and are shown in Table 2.
Table 2. Summary table showing studies of radiomics signatures to distinguish benign from cancerous lung pathologies.
| Name of Study | Number of CT Scans | Radiomics Feature | Statistical Tool Used to Assess Performance |
|---|---|---|---|
| Ardila et al. [93] | Data extracted from NLST: 6630 benign 86 malignant Independent validation set: 1112 benign 27 malignant |
1024 radiomics features were assessed and validated by expert radiologists. | AUC of training dataset: 0.944 AUC of validation dataset: 0.955 |
| Chen, et al. [94] | 33 benign 42 malignant |
Support vector machine (SVM) was used as the classifier. 76 out of 750 characteristics were appreciably distinctive between benign and malignant nodules. Accuracy for the selected 4-feature signature (SFS) was the maximum. |
SFS: Accuracy: 84% SN: 92.85% SP: 72.73% |
| Choi et al. [95] | 72 pulmonary nodules, 31 benign and 41 malignant |
103 radiomic signatures were tested. | Accuracy: 84.6% AUC: 0.89 |
| Delzell et al. [96] | 90 benign 110 malignant |
416 radiomic signatures. Combinations of the 6 feature selection methods and 12 classifiers were examined by applying a 10-fold repeated cross-validation framework with 5 repeats. |
AUC: 0.747 SN: 61.6% SP: 72.9% |
| Hawkins et al. [97] | Data extracted from NLST: 328 benign 170 malignant |
219 radiomic signature with best model finding 23 stable signatures. J48, JRIP (RIPPER), Naïve Bayes, support vector machines (SVMs), and random forest(s) classifiers tested. |
Accuracy: 80% AUC: 0.83 |
| Peikert et al. [98] | Data extracted from NLST: 318 benign 408 malignant |
LASSO logistic regression model implemented. 8 out of 57 radiomic signatures utilised. |
AUC: 0.939 |
To conclude, radiomics offers a tangible opportunity for even wider use of medical imaging in oncology, especially in difficult to access lesions or lesions in patients in whom invasive lung biopsy could be detrimental.
This entry is adapted from the peer-reviewed paper 10.3390/cancers14235782
References
- Bird, A. DNA methylation patterns and epigenetic memory. Genes Dev. 2002, 16, 6–21.
- Darilmaz Yuce, G.; Ortac Ersoy, E. Lung cancer and epigenetic modifications. Tuberk Toraks 2016, 64, 163–170.
- Nakagawa, H.; Fujita, M. Whole genome sequencing analysis for cancer genomics and precision medicine. Cancer Sci. 2018, 109, 513–522.
- Parikh, A.R. Lung Cancer Genomics. Acta Med. Acad. 2019, 48, 78–83.
- Sato, T.; Arai, E.; Kohno, T.; Takahashi, Y.; Miyata, S.; Tsuta, K.; Watanabe, S.; Soejima, K.; Betsuyaku, T.; Kanai, Y. Epigenetic clustering of lung adenocarcinomas based on DNA methylation profiles in adjacent lung tissue: Its correlation with smoking history and chronic obstructive pulmonary disease. Int. J. Cancer 2014, 135, 319–334.
- Selamat, S.A.; Galler, J.S.; Joshi, A.D.; Fyfe, M.N.; Campan, M.; Siegmund, K.D.; Kerr, K.M.; Laird-Offringa, I.A. DNA methylation changes in atypical adenomatous hyperplasia, adenocarcinoma in situ, and lung adenocarcinoma. PLoS ONE 2011, 6, e21443.
- Brock, M.V.; Hooker, C.M.; Ota-Machida, E.; Han, Y.; Guo, M.; Ames, S.; Glöckner, S.; Piantadosi, S.; Gabrielson, E.; Pridham, G.; et al. DNA methylation markers and early recurrence in stage I lung cancer. N. Engl. J. Med. 2008, 358, 1118–1128.
- Sato, T.; Arai, E.; Kohno, T.; Tsuta, K.; Watanabe, S.; Soejima, K.; Betsuyaku, T.; Kanai, Y. DNA methylation profiles at precancerous stages associated with recurrence of lung adenocarcinoma. PLoS ONE 2013, 8, e59444.
- Robles, A.I.; Arai, E.; Mathe, E.A.; Okayama, H.; Schetter, A.J.; Brown, D.; Petersen, D.; Bowman, E.D.; Noro, R.; Welsh, J.A.; et al. An Integrated Prognostic Classifier for Stage I Lung Adenocarcinoma Based on mRNA, microRNA, and DNA Methylation Biomarkers. J. Thorac. Oncol. 2015, 10, 1037–1048.
- Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 2014, 511, 543–550.
- Hawes, S.E.; Stern, J.E.; Feng, Q.; Wiens, L.W.; Rasey, J.S.; Lu, H.; Kiviat, N.B.; Vesselle, H. DNA hypermethylation of tumors from non-small cell lung cancer (NSCLC) patients is associated with gender and histologic type. Lung Cancer 2010, 69, 172–179.
- Carvalho, R.H.; Hou, J.; Haberle, V.; Aerts, J.; Grosveld, F.; Lenhard, B.; Philipsen, S. Genomewide DNA methylation analysis identifies novel methylated genes in non-small-cell lung carcinomas. J. Thorac. Oncol. 2013, 8, 562–573.
- Palmisano, W.A.; Divine, K.K.; Saccomanno, G.; Gilliland, F.D.; Baylin, S.B.; Herman, J.G.; Belinsky, A.S. Predicting lung cancer by detecting aberrant promoter methylation in sputum. Cancer Res. 2000, 60, 5954–5958.
- Kersting, M.; Friedl, C.; Kraus, A.; Behn, M.; Pankow, W.; Schuermann, M. Differential frequencies of p16(INK4a) promoter hypermethylation, p53 mutation, and K-ras mutation in exfoliative material mark the development of lung cancer in symptomatic chronic smokers. J. Clin. Oncol. 2000, 18, 3221–3229.
- Destro, A.; Bianchi, P.; Alloisio, M.; Laghi, L.; Di Gioia, S.; Malesci, A.; Cariboni, U.; Gribaudi, G.; Bulfamante, G.; Marchetti, A.; et al. K-ras and p16(INK4A)alterations in sputum of NSCLC patients and in heavy asymptomatic chronic smokers. Lung Cancer 2004, 44, 23–32.
- Zochbauer-Muller, S.; Lam, S.; Toyooka, S.; Virmani, A.K.; Toyooka, K.O.; Seidl, S.; Minna, J.D.; Gazdar, A.F. Aberrant methylation of multiple genes in the upper aerodigestive tract epithelium of heavy smokers. Int. J. Cancer 2003, 107, 612–616.
- Honorio, S.; Agathanggelou, A.; Schuermann, M.; Pankow, W.; Viacava, P.; Maher, E.R.; Latif, F. Detection of RASSF1A aberrant promoter hypermethylation in sputum from chronic smokers and ductal carcinoma in situ from breast cancer patients. Oncogene 2003, 22, 147–150.
- Belinsky, S.A.; Liechty, K.C.; Gentry, F.D.; Wolf, H.J.; Rogers, J.; Vu, K.; Haney, J.; Kennedy, T.C.; Hirsch, F.R.; Miller, Y.; et al. Promoter hypermethylation of multiple genes in sputum precedes lung cancer incidence in a high-risk cohort. Cancer Res. 2006, 66, 3338–3344.
- Lukas, J.; Parry, D.; Aagaard, L.; Mann, D.J.; Bartkova, J.; Strauss, M.; Peters, G.; Bartek, J. Retinoblastoma-protein-dependent cell-cycle inhibition by the tumour suppressor p16. Nature 1995, 375, 503–506.
- Cohen, O.; Feinstein, E.; Kimchi, A. DAP-kinase is a Ca2+/calmodulin-dependent, cytoskeletal-associated protein kinase, with cell death-inducing functions that depend on its catalytic activity. EMBO J. 1997, 16, 998–1008.
- Cohen, O.; Inbal, B.; Kissil, J.L.; Raveh, T.; Berissi, H.; Spivak-Kroizaman, T.; Feinstein, E.; Kimchi, A. DAP-kinase participates in TNF-alpha- and Fas-induced apoptosis and its function requires the death domain. J. Cell Biol. 1999, 146, 141–148.
- Eckfeld, K.; Hesson, L.; Vos, M.D.; Bieche, I.; Latif, F.; Clark, G.J. RASSF4/AD037 is a potential ras effector/tumor suppressor of the RASSF family. Cancer Res. 2004, 64, 8688–8693.
- Bearzatto, A.; Conte, D.; Frattini, M.; Zaffaroni, N.; Andriani, F.; Balestra, D.; Tavecchio, L.; Daidone, M.G.; Sozzi, G. p16(INK4A) Hypermethylation detected by fluorescent methylation-specific PCR in plasmas from non-small cell lung cancer. Clin. Cancer Res. 2002, 8, 3782–3787.
- Ponomaryova, A.A.; Rykova, E.Y.; Cherdyntseva, N.V.; Skvortsova, T.E.; Dobrodeev, A.Y.; Zav’yalov, A.A.; Bryzgalov, L.O.; Tuzikov, S.; Vlassov, V.; Laktionov, P.P. Potentialities of aberrantly methylated circulating DNA for diagnostics and post-treatment follow-up of lung cancer patients. Lung Cancer 2013, 81, 397–403.
- Nunes, S.P.; Moreira-Barbosa, C.; Salta, S.; Palma de Sousa, S.; Pousa, I.; Oliveira, J.; Soares, M.; Rego, L.; Dias, T.; Rodrigues, J.; et al. Cell-Free DNA Methylation of Selected Genes Allows for Early Detection of the Major Cancers in Women. Cancers 2018, 10, 357.
- Ostrow, K.L.; Hoque, M.O.; Loyo, M.; Brait, M.; Greenberg, A.; Siegfried, J.M.; Grandis, J.R.; Davis, A.G.; Bigbee, W.L.; Rom, W.; et al. Molecular analysis of plasma DNA for the early detection of lung cancer by quantitative methylation-specific PCR. Clin. Cancer Res. 2010, 16, 3463–3472.
- Weiss, G.; Schlegel, A.; Kottwitz, D.; Konig, T.; Tetzner, R. Validation of the SHOX2/PTGER4 DNA Methylation Marker Panel for Plasma-Based Discrimination between Patients with Malignant and Nonmalignant Lung Disease. J. Thorac. Oncol. 2017, 12, 77–84.
- Kang, S.; Li, Q.; Chen, Q.; Zhou, Y.; Park, S.; Lee, G.; Grimes, B.; Krysan, K.; Yu, M.; Wang, W.; et al. CancerLocator: Non-invasive cancer diagnosis and tissue-of-origin prediction using methylation profiles of cell-free DNA. Genome. Biol. 2017, 18, 53.
- Vafadar, A.; Shabaninejad, Z.; Movahedpour, A.; Mohammadi, S.; Fathullahzadeh, S.; Mirzaei, H.R.; Namdar, A.; Savardashtaki, A.; Mirzaei, H. Long Non-Coding RNAs As Epigenetic Regulators in Cancer. Curr. Pharm. Des. 2019, 25, 3563–3577.
- Shabaninejad, Z.; Vafadar, A.; Movahedpour, A.; Ghasemi, Y.; Namdar, A.; Fathizadeh, H.; Pourhanifeh, M.H.; Savardashtaki, A.; Mirzaei, H. Circular RNAs in cancer: New insights into functions and implications in ovarian cancer. J. Ovarian Res. 2019, 12, 84.
- Naeli, P.; Yousefi, F.; Ghasemi, Y.; Savardashtaki, A.; Mirzaei, H. The Role of MicroRNAs in Lung Cancer: Implications for Diagnosis and Therapy. Curr. Mol. Med. 2020, 20, 90–101.
- Wang, K. The Ubiquitous Existence of MicroRNA in Body Fluids. Clin. Chem. 2017, 63, 784–785.
- Calin, G.A.; Dumitru, C.D.; Shimizu, M.; Bichi, R.; Zupo, S.; Noch, E.; Aldler, H.; Rattan, S.; Keating, M.; Rai, K.; et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc. Natl. Acad. Sci. USA 2002, 99, 15524–15529.
- Zhang, B.; Pan, X.; Cobb, G.P.; Anderson, T.A. microRNAs as oncogenes and tumor suppressors. Dev. Biol. 2007, 302, 1–12.
- Croce, C.M. Causes and consequences of microRNA dysregulation in cancer. Nat. Rev. Genet. 2009, 10, 704–714.
- Movahedpour, A.; Ahmadi, N.; Ghasemi, Y.; Savardashtaki, A.; Shabaninejad, Z. Circulating microRNAs as potential diagnostic biomarkers and therapeutic targets in prostate cancer: Current status and future perspectives. J. Cell Biochem. 2019, 120, 16316–16329.
- Alberg, A.J.; Brock, M.V.; Ford, J.G.; Samet, J.M.; Spivack, S.D. Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143 (Suppl. 5), e1S–e29S.
- Wood, D.E.; Kazerooni, E.A.; Baum, S.L.; Eapen, G.A.; Ettinger, D.S.; Hou, L.; Jackman, D.M.; Klippenstein, D.; Kumar, R.; Lackner, R.P.; et al. Lung Cancer Screening, Version 3.2018, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2018, 16, 412–441.
- Fleischhacker, M.; Schmidt, B. Circulating nucleic acids (CNAs) and cancer—A survey. Biochim. Biophys. Acta 2007, 1775, 181–232.
- Stroun, M.; Lyautey, J.; Lederrey, C.; Olson-Sand, A.; Anker, P. About the possible origin and mechanism of circulating DNA apoptosis and active DNA release. Clin. Chim. Acta 2001, 313, 139–142.
- Anker, P.; Stroun, M.; Maurice, P.A. Spontaneous release of DNA by human blood lymphocytes as shown in an in vitro system. Cancer Res. 1975, 35, 2375–2382.
- Jahr, S.; Hentze, H.; Englisch, S.; Hardt, D.; Fackelmayer, F.O.; Hesch, R.D.; Knippers, R. DNA fragments in the blood plasma of cancer patients: Quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res. 2001, 61, 1659–1665.
- Diehl, F.; Schmidt, K.; Choti, M.A.; Romans, K.; Goodman, S.; Li, M.; Thornton, K.; Agrawal, N.; Sokoll, L.; Szabo, S.A.; et al. Circulating mutant DNA to assess tumor dynamics. Nat. Med. 2008, 14, 985–990.
- Bettegowda, C.; Sausen, M.; Leary, R.J.; Kinde, I.; Wang, Y.; Agrawal, N.; Bartlett, B.R.; Wang, H.; Luber, B.; Alani, R.M.; et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl. Med. 2014, 6, 224ra24.
- Seoane, J.; De Mattos-Arruda, L.; Le Rhun, E.; Bardelli, A.; Weller, M. Cerebrospinal fluid cell-free tumour DNA as a liquid biopsy for primary brain tumours and central nervous system metastases. Ann. Oncol. 2019, 30, 211–218.
- Sacher, A.G.; Paweletz, C.; Dahlberg, S.E.; Alden, R.S.; O’Connell, A.; Feeney, N.; Mach, S.L.; Jänne, P.A.; Oxnard, G.R. Prospective Validation of Rapid Plasma Genotyping for the Detection of EGFR and KRAS Mutations in Advanced Lung Cancer. JAMA Oncol. 2016, 2, 1014–1022.
- Schmiegel, W.; Scott, R.J.; Dooley, S.; Lewis, W.; Meldrum, C.J.; Pockney, P.; Draganic, B.; Smith, S.; Hewitt, C.; Philimore, H.; et al. Blood-based detection of RAS mutations to guide anti-EGFR therapy in colorectal cancer patients: Concordance of results from circulating tumor DNA and tissue-based RAS testing. Mol. Oncol. 2017, 11, 208–219.
- Siravegna, G.; Mussolin, B.; Venesio, T.; Marsoni, S.; Seoane, J.; Dive, C.; Papadopoulos, N.; Kopetz, S.; Corcoran, R.B.; Siu, L.L.; et al. How liquid biopsies can change clinical practice in oncology. Ann. Oncol. 2019, 30, 1580–1590.
- Doria-Rose, V.P.; White, M.C.; Klabunde, C.N.; Nadel, M.R.; Richards, T.B.; McNeel, T.S.; Rodriguez, J.L.; Marcus, P.M. Use of lung cancer screening tests in the United States: Results from the 2010 National Health Interview Survey. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1049–1059.
- Passiglia, F.; Rizzo, S.; Rolfo, C.; Galvano, A.; Bronte, E.; Incorvaia, L.; Listi, A.; Barraco, N.; Castiglia, M.; Calo, V.; et al. Metastatic Site Location Influences the Diagnostic Accuracy of ctDNA EGFR- Mutation Testing in NSCLC Patients: A Pooled Analysis. Curr. Cancer Drug Targets 2018, 18, 697–705.
- Chabon, J.J.; Hamilton, E.G.; Kurtz, D.M.; Esfahani, M.S.; Moding, E.J.; Stehr, H.; Schroers-Martin, J.; Nabet, B.Y.; Chen, B.; Chaudhuri, A.A.; et al. Integrating genomic features for non-invasive early lung cancer detection. Nature 2020, 580, 245–251.
- Abbosh, C.; Birkbak, N.J.; Swanton, C. Early stage NSCLC—Challenges to implementing ctDNA-based screening and MRD detection. Nat. Rev. Clin. Oncol. 2018, 15, 577–586.
- Chaudhuri, A.A.; Chabon, J.J.; Lovejoy, A.F.; Newman, A.M.; Stehr, H.; Azad, T.D.; Khodadoust, M.S.; Esfahani, M.S.; Liu, C.L.; Zhou, L.; et al. Early Detection of Molecular Residual Disease in Localized Lung Cancer by Circulating Tumor DNA Profiling. Cancer Discov. 2017, 7, 1394–1403.
- Abbosh, C.; Birkbak, N.J.; Wilson, G.A.; Jamal-Hanjani, M.; Constantin, T.; Salari, R.; Le Quesne, J.; Moore, D.A.; Veeriah, S.; Rosenthal, R.; et al. Phylogenetic ctDNA analysis depicts early-stage lung cancer evolution. Nature 2017, 545, 446–451.
- Sacher, A.G.; Komatsubara, K.M.; Oxnard, G.R. Application of Plasma Genotyping Technologies in Non-Small Cell Lung Cancer: A Practical Review. J. Thorac. Oncol. 2017, 12, 1344–1356.
- Hu, Y.; Ulrich, B.C.; Supplee, J.; Kuang, Y.; Lizotte, P.H.; Feeney, N.B.; Guibert, N.M.; Awad, M.M.; Wong, K.K.; Jänne, P.A.; et al. False-Positive Plasma Genotyping Due to Clonal Hematopoiesis. Clin. Cancer Res. 2018, 24, 4437–4443.
- Slavin, T.P.; Banks, K.C.; Chudova, D.; Oxnard, G.R.; Odegaard, J.I.; Nagy, R.J.; Tsang, K.W.K.; Neuhausen, S.L.; Gray, S.W.; Cristofanilli, M.; et al. Identification of Incidental Germline Mutations in Patients With Advanced Solid Tumors Who Underwent Cell-Free Circulating Tumor DNA Sequencing. J. Clin. Oncol. 2018, 36, 3459–3465.
- Ignatiadis, M.; Sledge, G.W.; Jeffrey, S.S. Liquid biopsy enters the clinic—Implementation issues and future challenges. Nat. Rev. Clin. Oncol. 2021, 18, 297–312.
- Esagian, S.M.; Grigoriadou, G.; Nikas, I.P.; Boikou, V.; Sadow, P.M.; Won, J.K.; Economopoulos, K.P. Comparison of liquid-based to tissue-based biopsy analysis by targeted next generation sequencing in advanced non-small cell lung cancer: A comprehensive systematic review. J. Cancer Res. Clin. Oncol. 2020, 146, 2051–2066.
- Rolfo, C.; Mack, P.C.; Scagliotti, G.V.; Baas, P.; Barlesi, F.; Bivona, T.G.; Herbst, R.S.; Mok, T.S.; Peled, N.; Pirker, R.; et al. Liquid Biopsy for Advanced Non-Small Cell Lung Cancer (NSCLC): A Statement Paper from the IASLC. J. Thorac. Oncol. 2018, 13, 1248–1268.
- Li, B.T.; Janku, F.; Jung, B.; Hou, C.; Madwani, K.; Alden, R.; Razavi, P.; Reis-Filho, J.S.; Shen, R.; Isbell, J.M.; et al. Ultra-deep next-generation sequencing of plasma cell-free DNA in patients with advanced lung cancers: Results from the Actionable Genome Consortium. Ann. Oncol. 2019, 30, 597–603.
- He, M.; Zeng, Y. Microfluidic Exosome Analysis toward Liquid Biopsy for Cancer. J. Lab. Autom. 2016, 21, 599–608.
- Panagiotara, A.; Markou, A.; Lianidou, E.S.; Patrinos, G.P.; Katsila, T. Exosomes: A Cancer Theranostics Road Map. Public Health Genom. 2017, 20, 116–125.
- Li, G.; Tang, W.; Yang, F. Cancer Liquid Biopsy Using Integrated Microfluidic Exosome Analysis Platforms. Biotechnol. J. 2020, 15, e1900225.
- Garcia-Cordero, J.L.; Maerkl, S.J. Microfluidic systems for cancer diagnostics. Curr. Opin. Biotechnol. 2020, 65, 37–44.
- Chen, C.K.; Liao, J.; Li, M.S.; Khoo, B.L. Urine biopsy technologies: Cancer and beyond. Theranostics 2020, 10, 7872–7888.
- Kowal, J.; Arras, G.; Colombo, M.; Jouve, M.; Morath, J.P.; Primdal-Bengtson, B.; Dingli, F.; Loew, D.; Tkach, M.; Théry, C. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc. Natl. Acad. Sci. USA 2016, 113, E968–E977.
- Zhang, W.; Zhang, X.J.; Chao, S.Y.; Chen, S.J.; Zhang, Z.J.; Zhao, J.; Lv, Y.N.; Yao, J.J.; Bai, Y.Y. Update on urine as a biomarker in cancer: A necessary review of an old story. Expert Rev. Mol. Diagn. 2020, 20, 477–488.
- Su, Y.H.; Wang, M.; Brenner, D.E.; Ng, A.; Melkonyan, H.; Umansky, S.; Syngal, S.; Block, T.M. Human urine contains small, 150 to 250 nucleotide-sized, soluble DNA derived from the circulation and may be useful in the detection of colorectal cancer. J. Mol. Diagn. 2004, 6, 101–107.
- Su, Y.H.; Song, J.; Wang, Z.; Wang, X.H.; Wang, M.; Brenner, D.E.; Block, T.M. Removal of high-molecular-weight DNA by carboxylated magnetic beads enhances the detection of mutated K-ras DNA in urine. Ann. N. Y. Acad. Sci. 2008, 1137, 82–91.
- Woodson, K.; O’Reilly, K.J.; Hanson, J.C.; Nelson, D.; Walk, E.L.; Tangrea, J.A. The usefulness of the detection of GSTP1 methylation in urine as a biomarker in the diagnosis of prostate cancer. J. Urol. 2008, 179, 508–511, Discussion 11–12.
- Ghanjati, F.; Beermann, A.; Hermanns, T.; Poyet, C.; Arauzo-Bravo, M.J.; Seifert, H.H.; Schmidtpeter, M.; Goering, W.; Sorg, R.; Wernet, P. Unreserved application of epigenetic methods to define differences of DNA methylation between urinary cellular and cell-free DNA. Cancer Biomark. 2014, 14, 295–302.
- Normanno, N.; Cervantes, A.; Ciardiello, F.; De Luca, A.; Pinto, C. The liquid biopsy in the management of colorectal cancer patients: Current applications and future scenarios. Cancer Treat. Rev. 2018, 70, 1–8.
- Reckamp, K.L.; Melnikova, V.O.; Karlovich, C.; Sequist, L.V.; Camidge, D.R.; Wakelee, H.; Perol, M.; Oxnard, G.R.; Kosco, K.; Croucher, P.; et al. A Highly Sensitive and Quantitative Test Platform for Detection of NSCLC EGFR Mutations in Urine and Plasma. J. Thorac. Oncol. 2016, 11, 1690–1700.
- Ren, S.; Ren, X.; Guo, H.; Liang, L.; Wei, K.; Guo, L.; Qu, X.; Dai, X.; Huang, Q. Concentration and integrity indexes of urine cell-free DNA as promising biomarkers for early lung cancer diagnosis. Pers. Med. 2021, 18, 129–139.
- Ren, S.; Ren, X.D.; Guo, L.F.; Qu, X.M.; Shang, M.Y.; Dai, X.-T.; Huang, Q. Urine cell-free DNA as a promising biomarker for early detection of non-small cell lung cancer. J. Clin. Lab. Anal. 2020, 34, e23321.
- Billatos, E.; Vick, J.L.; Lenburg, M.E.; Spira, A.E. The Airway Transcriptome as a Biomarker for Early Lung Cancer Detection. Clin. Cancer Res. 2018, 24, 2984–2992.
- Hu, Z.; Whitney, D.; Anderson, J.R.; Cao, M.; Ho, C.; Choi, Y.; Huang, J.; Frink, R.; Porta Smith, K.; Monroe, R.; et al. Analytical performance of a bronchial genomic classifier. BMC Cancer 2016, 16, 161.
- Silvestri, G.A.; Vachani, A.; Whitney, D.; Elashoff, M.; Porta Smith, K.; Ferguson, J.S.; Parsons, E.; Mitra, N.; Brody, J.; Lenburg, M.E.; et al. A Bronchial Genomic Classifier for the Diagnostic Evaluation of Lung Cancer. N. Engl. J. Med. 2015, 373, 243–251.
- Parekh, V.; Jacobs, M.A. Radiomics: A new application from established techniques. Expert Rev. Precis. Med. Drug Dev. 2016, 1, 207–226.
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.L.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J Cancer 2012, 48, 441–446.
- Thawani, R.; McLane, M.; Beig, N.; Ghose, S.; Prasanna, P.; Velcheti, V.; Madabhushi, A. Radiomics and radiogenomics in lung cancer: A review for the clinician. Lung Cancer 2018, 115, 34–41.
- Han, F.; Wang, H.; Zhang, G.; Han, H.; Song, B.; Li, L.; Moore, W.; Lu, H.; Zhao, H.; Liang, Z. Texture feature analysis for computer-aided diagnosis on pulmonary nodules. J. Digit Imaging 2015, 28, 99–115.
- Wilson, R.; Devaraj, A. Radiomics of pulmonary nodules and lung cancer. Transl. Lung Cancer Res. 2017, 6, 86–91.
- Alahmari, S.S.; Cherezov, D.; Goldgof, D.; Hall, L.; Gillies, R.J.; Schabath, M.B. Delta Radiomics Improves Pulmonary Nodule Malignancy Prediction in Lung Cancer Screening. IEEE Access 2018, 6, 77796–77806.
- Wang, Z.; Li, N.; Zheng, F.; Sui, X.; Han, W.; Xue, F.; Xu, X.; Yang, C.; Hu, Y.; Wang, L.; et al. Optimizing the timing of diagnostic testing after positive findings in lung cancer screening: A proof of concept radiomics study. J. Transl. Med. 2021, 19, 191.
- Khawaja, A.; Bartholmai, B.J.; Rajagopalan, S.; Karwoski, R.A.; Varghese, C.; Maldonado, F.; Peikert, T. Do we need to see to believe?-radiomics for lung nodule classification and lung cancer risk stratification. J. Thorac. Dis. 2020, 12, 3303–3316.
- Mao, L.; Chen, H.; Liang, M.; Li, K.; Gao, J.; Qin, P.; Ding, X.; Li, X.; Liu, X. Quantitative radiomic model for predicting malignancy of small solid pulmonary nodules detected by low-dose CT screening. Quant. Imaging Med. Surg. 2019, 9, 263–272.
- Akinci D’Antonoli, T.; Farchione, A.; Lenkowicz, J.; Chiappetta, M.; Cicchetti, G.; Martino, A.; Ottavianelli, A.; Manfredi, R.; Margaritora, S.; Bonomo, L.; et al. CT Radiomics Signature of Tumor and Peritumoral Lung Parenchyma to Predict Nonsmall Cell Lung Cancer Postsurgical Recurrence Risk. Acad. Radiol. 2020, 27, 497–507.
- Tu, W.; Sun, G.; Fan, L.; Wang, Y.; Xia, Y.; Guan, Y.; Li, Q.; Zhang, D.; Liu, S.; Li, Z. Radiomics signature: A potential and incremental predictor for EGFR mutation status in NSCLC patients, comparison with CT morphology. Lung Cancer 2019, 132, 28–35.
- Song, J.; Wang, L.; Ng, N.N.; Zhao, M.; Shi, J.; Wu, N.; Li, W.; Liu, Z.; Yeom, K.W.; Tian, J. Development and Validation of a Machine Learning Model to Explore Tyrosine Kinase Inhibitor Response in Patients With Stage IV EGFR Variant-Positive Non-Small Cell Lung Cancer. JAMA Netw. Open 2020, 3, e2030442.
- Tang, X.; Xu, X.; Han, Z.; Bai, G.; Wang, H.; Liu, Y.; Du, P.; Liang, Z.; Zhang, J.; Lu, H.; et al. Elaboration of a multimodal MRI-based radiomics signature for the preoperative prediction of the histological subtype in patients with non-small-cell lung cancer. Biomed. Eng. Online 2020, 19, 5.
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G.; et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961.
- Chen, C.H.; Chang, C.K.; Tu, C.Y.; Liao, W.C.; Wu, B.R.; Chou, K.T.; Chiou, Y.R.; Yang, S.N.; Zhang, G.; Huang, T.C. Radiomic features analysis in computed tomography images of lung nodule classification. PLoS ONE 2018, 13, e0192002.
- Choi, W.; Oh, J.H.; Riyahi, S.; Liu, C.J.; Jiang, F.; Chen, W.; White, C.; Rimner, A.; Mechalakos, J.G.; Deasy, J.O.; et al. Radiomics analysis of pulmonary nodules in low-dose CT for early detection of lung cancer. Med. Phys. 2018, 45, 1537–1549.
- Delzell, D.A.P.; Magnuson, S.; Peter, T.; Smith, M.; Smith, B.J. Machine Learning and Feature Selection Methods for Disease Classification With Application to Lung Cancer Screening Image Data. Front. Oncol. 2019, 9, 1393.
- Hawkins, S.; Wang, H.; Liu, Y.; Garcia, A.; Stringfield, O.; Krewer, H.; Li, Q.; Cherezov, D.; Gatenby, R.A.; Balagurunathan, Y.; et al. Predicting Malignant Nodules from Screening CT Scans. J. Thorac. Oncol. 2016, 11, 2120–2128.
- Peikert, T.; Duan, F.; Rajagopalan, S.; Karwoski, R.A.; Clay, R.; Robb, R.A.; Qin, Z.; Sicks, J.; Bartholmai, B.J.; Maldonado, F. Novel high-resolution computed tomography-based radiomic classifier for screen-identified pulmonary nodules in the National Lung Screening Trial. PLoS ONE 2018, 13, e0196910.
This entry is offline, you can click here to edit this entry!
