Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
The COVID-19 pandemic created the need for telerehabilitation development, while Industry 4.0 brought the key technology. As motor therapy often requires the physical support of a patient’s motion, combining robot-aided workouts with remote control is a promising solution. This may be realised with the use of the device’s digital twin so as to give it an immersive operation. Such technology may be used for manual remote kinesiotherapy, combined with the safety systems predicting potentially harmful situations. The concept is universally applicable to rehabilitation robots.
- digital twin
- exoskeletons
- home rehabilitation
- human–machine interaction
- IoT
- motor therapy
- robot-aided rehabilitation
- remote treatment
1. Introduction
Often, ideas about the future include the ability to control objects over long distances, visiting shops without leaving home, interactive, engaging games or meetings with loved ones anywhere and anytime thanks to a remote connection [1]. Within the last few years, there has been a strong need to bring these closer to the present. The COVID-19 pandemic has proved the need to revitalise the health service and create a new approach to patient treatment during crises. Hospitals, medical centres, and rehabilitation facilities have been crippled, mainly by a shortage of health workers who cannot maintain an adequate level of health services to meet the population’s growing needs. As urbanisation has led to the rapid spread of infectious diseases, while the population is ageing, the number of people requiring constant medical care is increasing [2]. Such challenges are met by telemedicine and telerehabilitation, intensively developed within recent years [3]. With the rise of digital technologies, remote monitoring of patients’ progress in therapy and the assessment of their health has been enabled. This is possible thanks to ECG, blood pressure, and glucose level measurements, among others [4]. Often, rehabilitation of people who cannot sit or stand independently requires the help of up to three physiotherapists, as it is too difficult for one [5]. Digital twins seem to be the solution in such situations. Initially, they were developed as digital equivalents of machines and industrial elements, such as engines or turbines [6]. They may be used to predict the system’s response in critical events and detect previously unidentified problems by comparing the predicted and actual responses [7]. Currently, attempts are being made to introduce this technology into healthcare to forecast potential outcomes of different treatment approaches [8]. Digital twins seem to be an ideal solution for the personalised therapy for each individual with a specific disease or condition [2]. Such models can consider many variables regarding the given case and predict their impact on a patient [9].
2. Robot-Aided Rehabilitation
The demand for physical support of older physiotherapists and preparing methodology of remote motor treatment led to the need for the overtaking of tiring activities by machines. Hence, an operator-less robotic solution must be implemented for home-based kinesiotherapy. However, current commercial devices are typically either too simple or too complex for self-in-house workouts. The first type of these machines is the one that mechanically supports a small number of DOFs or triggers the motion by the end effector attached to the body in series only [10][11]. With such an approach, a comprehensive treatment of patients with serious diseases may be given, and neither is monitoring their kinematics parameters possible [12][13]. An insufficient number of DOFs do not support tasks with genuine limb motion patterns. For example, a mechanism with three DOFs cannot be used for lifting a glass along a natural trajectory.
The complex rehabilitation robots are typically too large, heavy, and expensive to be purchased and applied by single users [5]. Moreover, they typically require operational space expanding beyond that available in most flats [14]. Hence, they are not applicable for home use, even though their advanced automation systems allow the generation of customised workout routines and the monitoring of performance continuously [15].
According to the aspects presented beforehand, the device for remote home motor therapy should be relatively simple in terms of mechanics, while remaining technologically advanced. Its structure has to enable easy putting on and training within the limited space. Moreover, it must enable control over the dynamic parameters of rehabilitated body parts—either by monitoring corresponding parameters in all the DOFs of machines or by involving an additional bio-signals tracking system. For these reasons, the exoskeleton lightweight structures are considered. They allow direct mobilisation of particular DOFs. Therefore, kinematics of corresponding joints may be calculated based on the data from encoders and impedance-based torque estimations [16].
At present, multiple various designs of exoskeletons for all the body parts have been developed [17][18][19]. As an addition, the ongoing research is focused on reducing the exoskeleton’s mass by computational optimisation and the application of new materials or manufacturing methods [20].
3. Remote Treatment
With the development of Information and Communication Technologies (ICT), new potential was unlocked for motor treatment. So-called telerehabilitation is a process of clinical therapy provided remotely using ICT [21]. However, so far, it has been mainly focused on non-robotised applications. An example of such an approach is implementing serious games based on different Virtual Reality scenarios. This allows a patient with motor difficulties to perform highly interactive and non-intrusive exercises. Furthermore, such interactive tools could also contribute to the automation of training assessments [22], which may be comparably effective to the co-located method [23]. Nevertheless, the described treatment may be introduced only to patients with minor injuries or diseases, as they need to move independently.
Providing distant treatment at a patient’s place of residence is a critical aspect of future physiotherapy. Moreover, this should be complementary to the robot-aided treatment. Hence, it is crucial to develop a stable and efficient method of remote kinesiotherapy using a mechatronic rehabilitation system.
Telerehabilitation can be synchronous (connecting patient and therapist in real-time via dedicated devices), asynchronous (computer-based interventions, which are remotely monitored and adapted offline by a therapist) or a combination of both [24]. The considered exoskeleton should enable onsite and remote treatment. The desired trajectories of the rehabilitated segments should be either programmed numerically or registered with the healthy body parts [14]. Moreover, a list of the standard exercises self-adjusting for the anatomical characteristics of a user should be provided within the system. A physiotherapist should be able to connect remotely and select the settings for the workout routine or use the automated database and optionally modify the suggested set. As for asynchronous telerehabilitation, they should be able to monitor patients’ performance with the minimum latency and possibly react to dangerous situations.
During the session, the robot should either support or resist the intended motion [25]. Some commercial companies investigate even more advanced methods, such as error enhancement [26]. A patient is supposed to act in order to follow the desired trajectory. With the automated settings, the therapy could be realised without the active intervention of a professional, who could supervise multiple persons simultaneously.
However, sometimes the treatment requires unpredictable means. Continuous non-anatomical motion patterns resulting in unequal loads distribution within the musculoskeletal system and extensive efforts [27], or the diseases affecting the neurological system [28][29][30], may create the need for another approach to treatment. In such a case, temporarily leading the body segments manually to find the optimal rehabilitation paths can be inevitable. The synchronous telerehabilitation with the robot could contribute to this. Nevertheless, such an application requires developing a control methodology to enable intuitive programming of the device’s motion mobilising patient regarding anatomical patterns.
4. Digital Twin in VR Based Control
The concept of the presented solution includes the industrial-like application of the digital twin to robot-aided motor therapy. The rehabilitation robots currently used for kinesiotherapy support or resist the motion of a patient. They may be either attached to the body segments in series (by end-effectors) or parallel (as exoskeletons) [31][32]. They are mainly operated by regulators of the motors controlling them so as to follow the pre-programmed trajectories within the time and under unknown loads. This brings higher accuracy and repeatability than the manual treatment with a physiotherapist, but does not give flexibility within the workouts. On the contrary, manual therapy may bring superior outcomes during specific cases which require real-time modification of exercises or experimental search of the optimal motion pattern [32]. Hence, the combination of both is the most effective when dealing with complex diseases, especially as both may be superior in particular cases [11][33].
While performing the physiotherapy in a clinic, it may be realised by combining manual therapy sessions and training with rehabilitation robots [34]. The real challenge is to transfer this approach to distant therapy.
The presented idea considers using the exoskeleton in the home of a patient connected with the remote control module. The treatment is initially based on the automatically generated routines based on the registered performance. However, all the adjustments may be modified online by the physiotherapist. Moreover, they have an opportunity to constantly monitor patients’ activity based on the impedance of the mechatronic device or additional sensors (e.g., EMG or EEG tracking).
The rehabilitation system is complemented with its digital twin. Additionally, the model contains schematic geometry of the rehabilitated body segment. The digital twin may be displayed in the VR goggles of the physiotherapist, as this provides the best immersion. AR or MR technologies are not considered because the patient is treated remotely, and the real-life environment of the physiotherapist is not connected with the rehabilitation process. Thanks to this, the professional can monitor the actual activity of the patient not only via registered signals but also based on the observed multibody model. As for the manual remote therapy, the physiotherapist should be able to drag the body segments to the desired configurations. This is realised by control over the virtual multibody model. Thanks to the kinematics formulas, the motion of the body segment may be recalculated into the desired motion of the motors. With the presented approach, manual therapy may be performed remotely in an intuitive and immersive way.
The concept of such an application is visualised in Figure 1. The presented method is not limited only to extremities and may be scalable even to the whole body or a group of patients, not necessarily located in the same room.
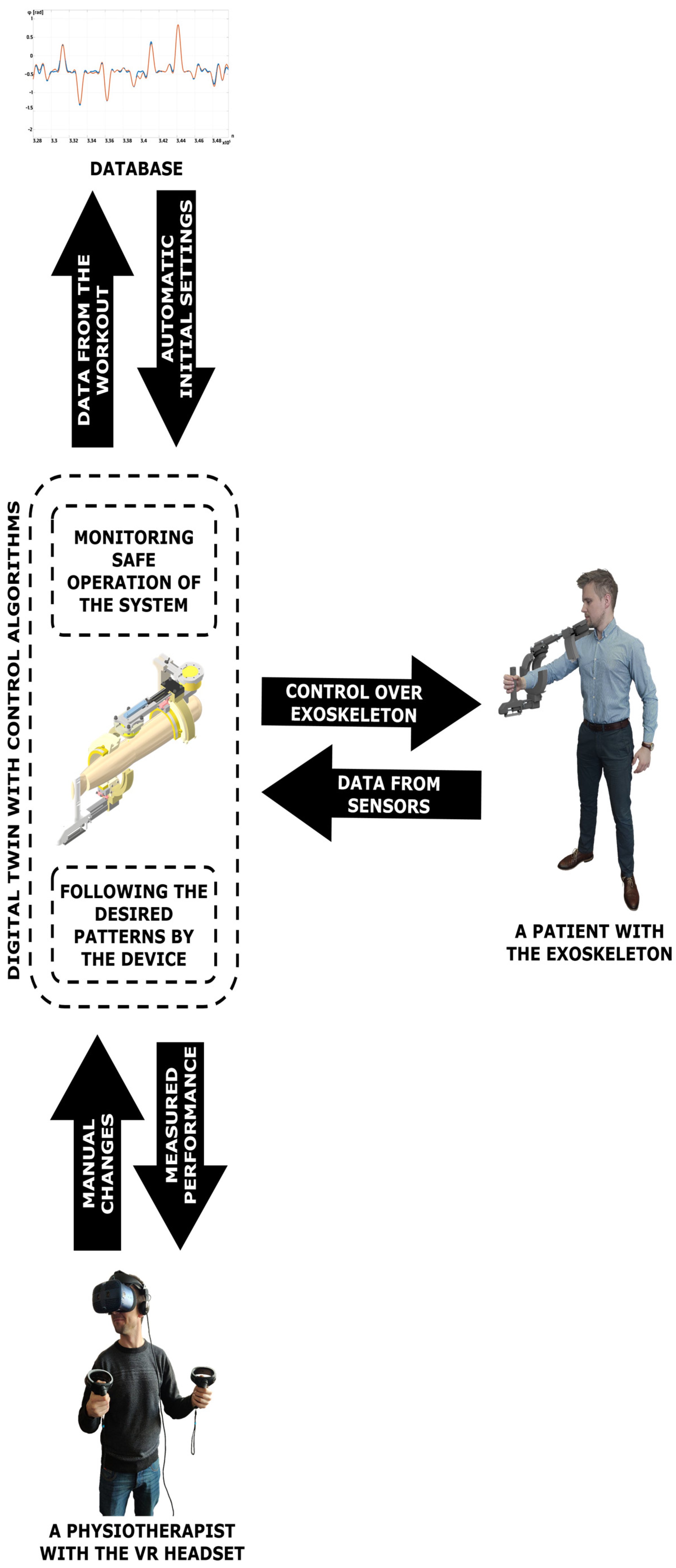
Figure 1. Block scheme of the system for digital twin based remote motor rehabilitation.
This entry is adapted from the peer-reviewed paper 10.3390/s23020911
References
- Orlosky, J.; Sra, M.; Bektaş, K.; Peng, H.; Kim, J.; Kos’Myna, N.; Höllerer, T.; Steed, A.; Kiyokawa, K.; Akşit, K. Telelife: The Future of Remote Living. Front. Virtual Real. 2021, 2, 763340.
- Boulos, M.K.; Zhang, P. Digital Twins: From Personalised Medicine to Precision Public Health. J. Pers. Med. 2021, 11, 745.
- DeFre Galea, M. Telemedicine in Rehabilitation. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 473–483.
- Volkov, I.; Radchenko, G.; Tchernykh, A. Digital Twins, Internet of Things and Mobile Medicine: A Review of Current Platforms to Support Smart Healthcare. Program. Comput. Softw. 2021, 47, 578–590.
- Díaz, I.; Gil, J.J.; Sánchez, E. Lower-Limb Robotic Rehabilitation: Literature Review and Challenges. J. Robot. 2011, 2011, 759764.
- Braun, M. Represent me: Please! Towards an ethics of digital twins in medicine. J. Med. Ethics 2021, 47, 394–400.
- Bruynseels, K.; de Sio, F.S.; Hoven, J.V.D. Digital Twins in Health Care: Ethical Implications of an Emerging Engineering Paradigm. Front. Genet. 2018, 9, 31.
- Rieke, N.; Hancox, J.; Li, W.; Milletarì, F.; Roth, H.R.; Albarqouni, S.; Bakas, S.; Galtier, M.N.; Landman, B.A.; Maier-Hein, K.; et al. The future of digital health with federated learning. NPJ Digit. Med. 2020, 3, 119.
- Björnsson, B.; on behalf of the Swedish Digital Twin Consortium; Borrebaeck, C.; Elander, N.; Gasslander, T.; Gawel, D.R.; Gustafsson, M.; Jörnsten, R.; Lee, E.J.; Li, X.; et al. Digital twins to personalize medicine. Genome Med. 2019, 12, 4.
- Macovei, S.; Doroftei, I. A short overview of upper limb rehabilitation devices. IOP Conf. Ser. Mater. Sci. Eng. 2016, 145, 052014.
- Chang, W.H.; Yun-Hee, K. Robot-assisted Therapy in Stroke Rehabilitation. J. Stroke 2013, 15, 174–181.
- Coote, S.; Murphy, T.B.; Harwin, W.; Stokes, E. The effect of the GENTLE/s robot-mediated therapy system on arm function after stroke. Clin. Rehabil. 2008, 22, 395–405.
- Lum, P.S.; Burgar, C.G.; Van der Loos, M.; Shor, P.C.; Majmundar, M.; Yap, R. Undefined 2006, “MIME Robotic Device for Upper-Limb Neurorehabilitation in Subacute Stroke Subjects: A Follow-Up Study,” books.google.com. Available online: https://www.google.com/books?hl=pl&lr=&id=O2y3AAAAIAAJ&oi=fnd&pg=PA631&dq=MIME+robotic+device+for+upper-limb+neurorehabilitation+in+subacute+stroke+subjects:+A+follow-up+study&ots=0uBlXrFRkA&sig=Hp18z8l79EfoI0Nca-FD56upOOw (accessed on 25 February 2022).
- Wang, H.; Feng, Y.; Yu, H.; Wang, Z.; Vladareanuv, V.; Du, Y. Mechanical design and trajectory planning of a lower limb rehabilitation robot with a variable workspace. Int. J. Adv. Robot. Syst. 2018, 15, 1729881418776855.
- Oña, E.D.; Cano-de La Cuerda, R.; Sánchez-Herrera, P.; Balaguer, C.; Jardón, A. A Review of Robotics in Neurorehabilitation: Towards an Automated Process for Upper Limb. J. Healthc. Eng. 2018, 2018, 9758939.
- Arciniegas-Mayag, L.; Rodriguez-Guerrero, C.; Rocon, E.; Múnera, M.; Cifuentes, C.A. Impedance Control Strategies for Lower-Limb Exoskeletons. In Interfacing Humans and Robots for Gait Assistance and Rehabilitation; Springer: Cham, Switzerland, 2022; pp. 213–236.
- Olar, M.-L.; Leba, M.; Risteiu, M. Exoskeleton—Wearable devices. Literature review. MATEC Web Conf. 2021, 342, 05005.
- Lee, H.; Ferguson, P.W.; Rosen, J. Lower Limb Exoskeleton Systems—Overview. Wearable Robot. 2020, 207–229.
- Ferraro, E.I.; Orofino, F.; Parisi, M.C.; Bellomo, M.; Francavilla, V.C.; Crescimanno, C. Artificial musculature: An overview of the different exoskeleton models and their applications. J. Hum. Sport Exerc. 2021, 16, S892–S904.
- Falkowski, P. Light Exoskeleton Design with Topology Optimisation and FEM Simulations for FFF Technology. J. Autom. Mob. Robot. Intell. Syst. 2022, 16, 14–19.
- Brennan, D.M.; Mawson, S.; Brownsell, S. Telerehabilitation: Enabling the Remote Delivery of Healthcare, Rehabilitation, and Self Management. Stud. Health Technol. Inform. 2009, 145, 231–248.
- Postolache, O.; Hemanth, D.J.; Alexandre, R.; Gupta, D.; Geman, O.; Khanna, A. Remote Monitoring of Physical Rehabilitation of Stroke Patients Using IoT and Virtual Reality. IEEE J. Sel. Areas Commun. 2020, 39, 562–573.
- Durfee, W.K.; Savard, L.; Weinstein, S. Technical Feasibility of Teleassessments for Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 23–29.
- Bettger, J.P.; Resnik, L.J. Telerehabilitation in the Age of COVID-19: An Opportunity for Learning Health System Research. Phys. Ther. 2020, 100, 1913–1916.
- Kahn, L.E.; Lum, P.S.; Rymer, W.Z.; Reinkensmeyer, D.J. Robot-assisted movement training for the stroke-impaired arm: Does it matter what the robot does? J. Rehabil. Res. Dev. 2006, 43, 619–630.
- Givon-Mayo, R.; Simons, E.; Ohry, A.; Karpin, H.; Israely, S.; Carmeli, E. A preliminary investigation of error enhancement of the velocity component in stroke patients’ reaching movements. Int. J. Ther. Rehabil. 2014, 21, 160–168.
- Khatib, O.; Demircan, E.; De Sapio, V.; Sentis, L.; Besier, T.; Delp, S. Robotics-based synthesis of human motion. J. Physiol. 2009, 103, 211–219.
- De Carvalho, M.; Swash, M. Motor unit recruitment in myopathy: The myopathic EMG reconsidered. J. Electromyogr. Kinesiol. 2019, 45, 41–45.
- Chen, Y.-T.; Li, S.; Magat, E.; Zhou, P.; Li, S. Motor Overflow and Spasticity in Chronic Stroke Share a Common Pathophysiological Process: Analysis of Within-Limb and between-Limb EMG-EMG Coherence. Front. Neurol. 2018, 9, 795.
- Morris, J. Amyotrophic Lateral Sclerosis (ALS) and Related Motor Neuron Diseases: An Overview. Neurodiagnostic J. 2015, 55, 180–194.
- Lee, S.H.; Park, G.; Cho, D.Y.; Kim, H.Y.; Lee, J.-Y.; Kim, S.; Park, S.-B.; Shin, J.-H. Comparisons between end-effector and exoskeleton rehabilitation robots regarding upper extremity function among chronic stroke patients with moderate-to-severe upper limb impairment. Sci. Rep. 2020, 10, 1806.
- Rodgers, H.; Bosomworth, H.; Krebs, H.I.; van Wijck, F.; Howel, D.; Wilson, N.; Aird, L.; Alvarado, N.; Andole, S.; Cohen, D.L.; et al. Robot assisted training for the upper limb after stroke (RATULS): A multicentre randomized controlled trial. Lancet 2019, 394, 51–62.
- Straudi, S.; Tramontano, M.; Russo, E.F.; Perrero, L.; Agostini, M.; Gandolfi, M.; Aprile, I.; Paci, M.; Casanova, E.; Marino, D.; et al. Robot-Assisted Upper Limb Training for Patients with Multiple Sclerosis: An Evidence-Based Review of Clinical Applications and Effectiveness. Appl. Sci. 2021, 12, 222.
- Mazzoleni, S.; Duret, C.; Grosmaire, A.G.; Battini, E. Combining Upper Limb Robotic Rehabilitation with Other Therapeutic Approaches after Stroke: Current Status, Rationale, and Challenges. BioMed Res. Int. 2017, 2017, 8905637.
This entry is offline, you can click here to edit this entry!
