Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Dental implants or prosthetics are used to replace missing teeth and treat partially or fully damaged teeth. The dental implant success rate is more than 90% after ten years, ensuring long-term reliability. There are three primary types of dental implants: endosteal or endosseous, subperiosteal, and transosteal. Dental implants are a continuously growing market for both medical and cosmetic purposes. Modern science has allowed dentists to offer a wide variety of implants, such as crowns, screws, dental bridges, dentures, and braces. Implant reliability and proper design are essential for patient comfort and usage. The selection of suitable materials, depending on the patient’s oral health and implant objectives, is the primary criteria for proper implant design.
- dental implants
- metals
- mechanical properties
- Wear
- Additive Manufacturing
- Biotribology
1. Endosteal or Endosseous Dental Implants
Endosseous dental implants are inserted within the mandible or maxilla and serve as the dental root (Figure 1). Titanium is typically used as the base material for this kind of implant. Cp (commercially pure) grade 4 titanium is used in many implants; however, titanium alloys are often used because of their higher corrosion resistance, strength, and biocompatibility. Ti-6Al-4V and TiZr are the two primary alloys used [1][2]. There are two types of endosteal implants: root and blade implants.
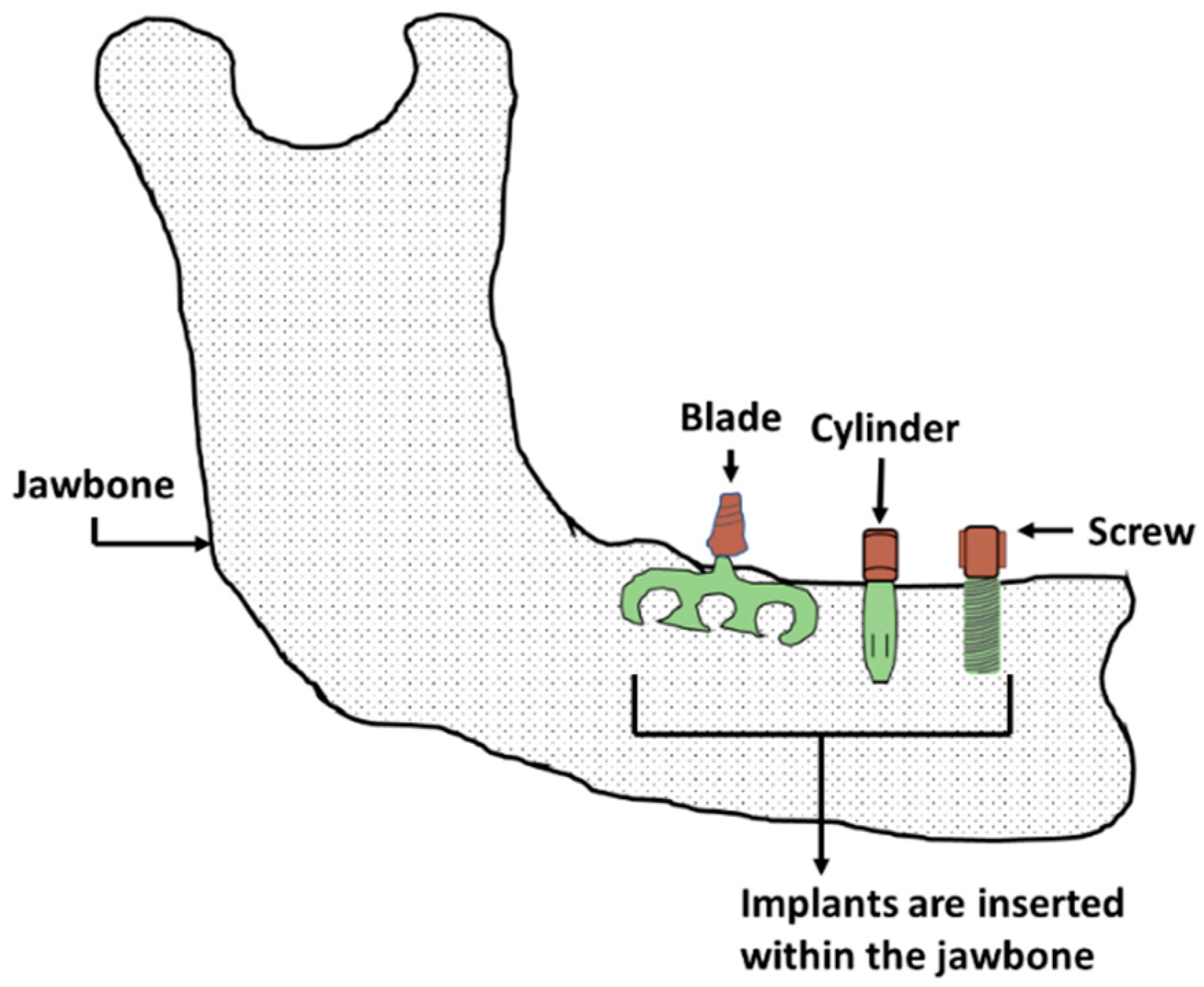
Figure 1. Endosteal or endosseous dental implants.
1.1. Root Implants
Endosseous root implants are used to support dentures or replace a damaged tooth’s root. This implant can be inserted into either the mandible or maxilla, depending on the damage location. The type of implant needed depends on the patient’s root cavity condition, damage type, and age. There are three major root implant types: screw threads, solid-body press-fit design, and porous material coated design. The physical topography of this implant may be cylindrical or conical shape (Figure 1). Screw threads or solid body press-fits can be added to a tooth’s primary shape. Most implants are cylindrical, conical, or thread shape, the most common of which is threaded or screw shape (Figure 1). Extensive research has been performed on the factors that improve screw implant success rates, such as implant diameter, implant length, geometry, and threading [3][4][5][6]. A root screw’s length ranges between 8 and 15 mm with diameters ranging between 3 and 7 mm [1]. A longer screw can dissipate stress with a large surface area, which results in good osseointegration. Wider screws can interact with larger bone areas and are better suited for removal torque tests [1][7]. The addition of threads to the root implant aids in improving initial stability, increasing initial contact, and enlarging the surface area. The most common thread designs are V-thread, square thread, and buttress thread. Square threaded designs exhibit more bone compaction and biomechanical integration than others [8][9].
1.2. Blade Implants
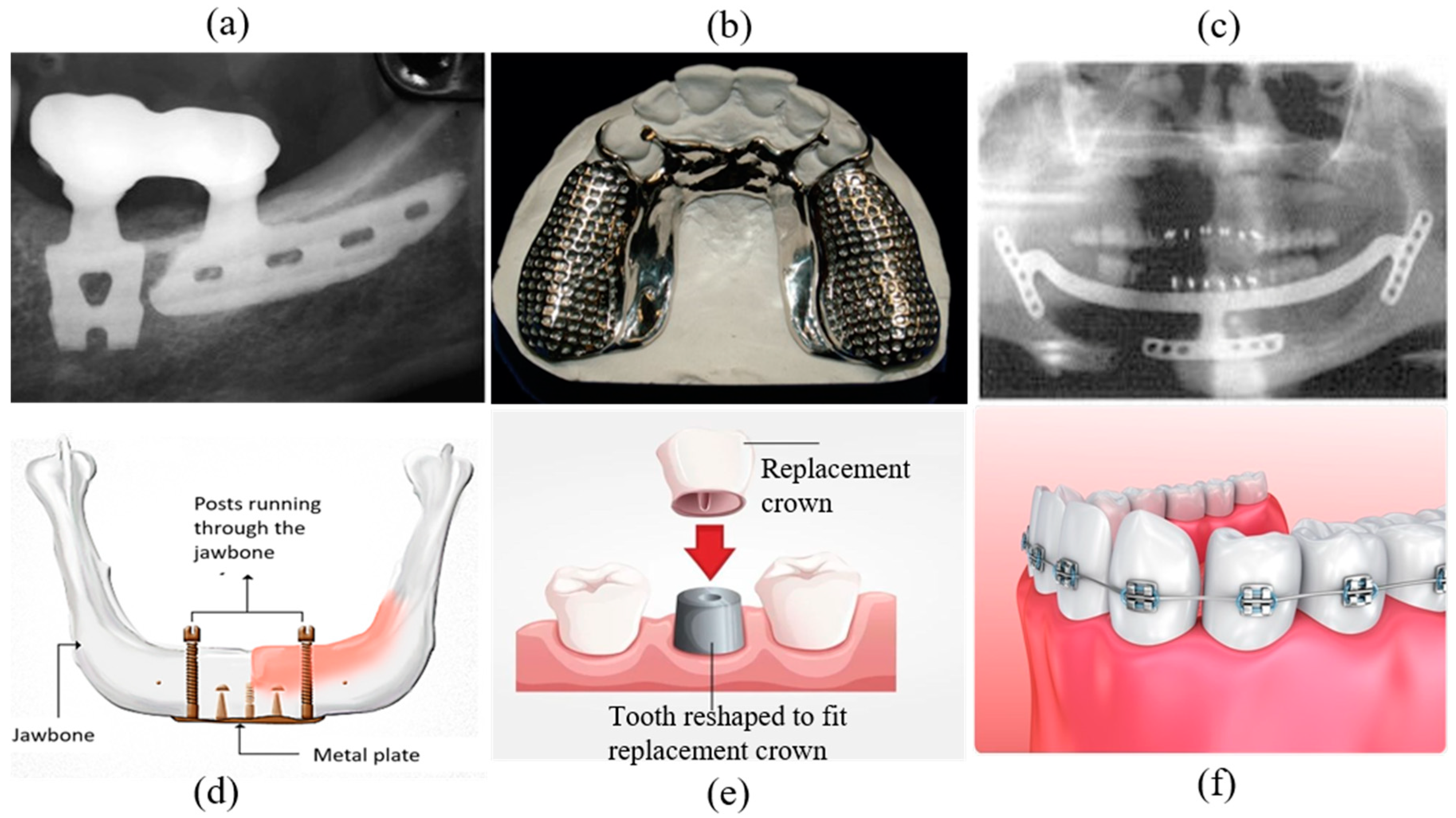
A blade implant can be a custom-made anchor for a dental prosthetic (Figure 1). Figure 2a depicts a representative image of a blade implant used in human dentistry. This type of implant supports an abutment using a metal plate placed laterally instead of in the vertical direction of a dental root. A critical factor when designing this implant is allowing the implant to bend so it can be positioned parallel to the curved mandible or maxilla and maintain alignment with the abutment. The blade implant is most useful with knife-edged ridges. The metal–bone contact area for a blade implant is higher than a root implant due to its unique design, promoting better osteointegration. The blade implantation procedure is also simpler than other types of implants [10].
2. Subperiosteal Dental Implants
Subperiosteal implants are positioned between the jawbone and gum. The implant will become fastened to the jawbone through osseointegration. These types of implants include dentures and ramus frames. Dentures can be classified as fixed dental dentures and removable dentures; then, they can be further classified as partial or full based on placement technique and patient need. Removable partial dentures (RPDs) are currently the most popular implant due to anatomical, physiological and economic conditions, even though they require maxillary or mandibular rehabilitation (Figure 2b) [11]. Dentures are typically created using the lost wax technique; however, 3D scanning and rapid prototyping are becoming popular with advancements in materials and manufacturing. Four general classification outlines, Class I, II, III, and IV, were proposed by Dr. Edward Kennedy for partially edentulous arches [12]. RPD could be used for this treatment depending on the categorized oral conditions.
- i.
-
CLASS I: Bilateral Posterior Edentulous Area;
- ii.
-
CLASS II: Unilateral Posterior Edentulous Area;
- iii.
-
CLASS III: Unilateral or Bilateral Edentulous Area(s) Bounded by Remaining Tooth/Teeth;
- iv.
-
CLASS IV: Single Edentulous Area Anterior to Remaining Teeth and Crossing the Midline.
A ramus frame is a U-shaped one-piece mandibular implant (Figure 2c) that can be supported at the wisdom teeth and under the chin. Its specific design, tripoidal shape, provides a unique support structure for the mandibular denture [13]. This type of implant may be used if the required dental implants are missing conventional support placements. This frame can also be useful for reducing discomfort caused by damaged gums, resolving chewing difficulties caused by implants, stabilizing an implant in the correct position, and mitigating speaking challenges.
3. Transosteal Implants
Endosseous and subperiosteal implants require sufficient bone support from the mandible. A transosteal implant can be used if the patient has severe resorption and jaw damage resulting from failure caused by insufficient implant support (Figure 2d). A metal plate with screws piercing through the jawbone is bolted to the lower mandible to support the metal rods of other implants running from the superior mandible to the inferior border, acting as a horizontal support beam [14]. Both intra- and extra-oral incisions are required to ensure proper stability, which is also referred to as a mandibular staple. Transosteal implants are not used frequently, since they are prohibitively expensive.
4. Other Dental Implant Types
Other types of implants, which are used for aesthetic purposes or to cover the original implant, exist. These implants are usually designed for temporary use and can be redesigned or relocated based on the patient’s needs.
4.1. Dental Crown
One of the most common implants is the dental crown (Figure 2e). A crown, or cap, is generally used to protect a weak tooth, restore a broken tooth, or cover a tooth filling and dental implant. A crown’s support system could be a natural tooth, dental implant, or bone [15]. One essential aspect of a dental crown is its placement technique on the root abutment. The implant abutments connect the prosthetics, a dental crown in this case, to the endosteal implant [16]. The dental crown protects the tooth from further damage since it acts as the tooth’s outer surface. A patient can receive a temporary crown while waiting for a permanent one. Crowns can be made from various materials, including metal, porcelain, ceramic, zirconia, or composite resin [17][18].
4.2. Dental Braces
Braces are temporary, wire-based implants that attach to teeth to fix alignment or crowding primarily for aesthetic purposes (Figure 2f). Brace positioning requires complex tooth defects and brace positioning knowledge as well as the effects of wire tension. Braces are usually made of stainless steel; however, ceramics are increasing in popularity. Stainless steel is the material best suited for braces; however, nickel ions leached from the steel alloy may cause sensitization or allergic reactions [19].
4.3. Dental Veneers
Dental veneers are wafer-thin, custom-made shells of tooth-colored porcelain or resin composites designed to cover a tooth’s front surface to improve appearance. The veneer material’s adhesion to the tooth’s surface gives patients a classically shaped look. Veneers are used for stained teeth, misshapen teeth, substantial gaps between front teeth, or worn teeth.
This entry is adapted from the peer-reviewed paper 10.3390/ma16010161
References
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50.
- Michelle Grandin, H.; Berner, S.; Dard, M. A review of Titanium Zirconium (TiZr) alloys for use in endosseous dental implants. Materials 2012, 5, 1348–1360.
- Misch, C.E. Contemporary Implant Dentistry, 2nd ed.; Mosby: St. Louis, MO, USA, 1999; ISBN 9780815170594.
- Winkler, S.; Morris, H.F.; Ochi, S. Implant survival to 36 months as related to length and diameter. Ann. Periodontol. 2000, 5, 22–31.
- Ivanoff, C.J.; Gröndahl, K.; Sennerby, L.; Bergström, C.; Lekholm, U. Influence of variations in implant diameters: A 3- to 5-year retrospective clinical report. Int. Oral Maxillofac Implant. 1999, 14, 173–180.
- Misch, C.E.; Qu, Z.; Bidez, M.W. Mechanical properties of trabecular bone in the human mandible: Implications for dental implant treatment planning and surgical placement. Int. J. Oral Maxillofac Surg. 1999, 57, s0278–s2391.
- Lee, J.H.; Frias, V.; Lee, K.W.; Wright, R.F. Effect of implant size and shape on implant success rates: A literature review. J. Prosthet. Dent. 2005, 94, 377–381.
- Misch, C.E.; Bidez, M.W.; Sharawy, M. A Bioengineereed Implant for a Predetermined Bone Cellular Response to Loading Forces. A Literature Review and Case Report. J. Periodontol. 2001, 72, 1276–1286.
- Bumgardner, J.D.; Boring, J.G.; Cooper, R.C., Jr.; Gao, C.; Givaruangsawat, S.; Gilbert, J.A.; Misch, C.M.; Steflik, D. Preliminary evaluation of a new dental implant design in canine models. Implant Dent. 2000, 9, 252–260.
- Linkow, L.I.; Winkler, S.; Shulman, M.; Carlo, L.D.; Pasqualini, M.E.; Rossi, F.; Nardone, M. A new look at the blade implant. J. Oral Implantol. 2016, 42, 373–380.
- Lima, J.M.C.; Anami, L.C.; Araujo, R.M.; Pavanelli, C.A. Removable partial dentures: Use of rapid prototyping. J. Prosthodont. 2014, 23, 588–591.
- Carr, A.; Brown, D. McCracken’s Removable Partial Prosthodontics, 13th ed.; Elsevier: Amsterdam, The Netherlands, 2016; ISBN 9780323339919.
- American Dental Association; Turner, H.F. Ramus frame implant technique. J. Am. Dent. Assoc. 1990, 121, 418–420.
- Dmd, K.U. Effects of Chemical and Prophylactic Agents Used in Dentistry on Titanium Implant Surfaces. Ph.D. Thesis, University of Szeged, Dugonics tér, Hungary, 2013.
- Misch, C.E. Single-Tooth Implant Restoration: Maxillary Anterior and Posterior Regions. Dent. Implant. Prosthet. 2015, 499–552.
- Prasad, D.K.; Prasad, D.A.; Bardia, A.; Hegde, C. Questionable abutments: General considerations, changing trends in treatment planning and available options. J. Interdiscip. Dent. 2013, 3, 12.
- Rathi, S.; Verma, A. Material Selection for Single-Tooth Crown Restorations; Elsevier: Amsterdam, The Netherlands, 2018; ISBN 9780128137598.
- Makhija, S.K.; Mph, D.D.S.; Lawson, N.C.; Gilbert, G.H.; Litaker, M.S.; Mcclelland, J.A.; Louis, D.R.; Valeria, V.; Ms-ci, D.D.S.M.S.; Pihlstrom, D.J.; et al. Dentist Material Selection for Single-Unit Crowns: Findings from The National Dental Practice-Based Research Network. J. Dent. 2017, 55, 40–47.
- Jensen, C.S.; Lisby, S.; Baadsgaard, O.; Byrialsen, K.; Menné, T. Release of nickel ions from stainless steel alloys used in dental braces and their patch test reactivity in nickel-sensitive individuals. Contact Dermat. 2003, 48, 300–304.
- Almufleh, B.; Emami, E.; Alageel, O.; de Melo, F.; Seng, F.; Caron, E.; Nader, S.A.; Al-Hashedi, A.; Albuquerque, R.; Feine, J.; et al. Patient satisfaction with laser-sintered removable partial dentures: A crossover pilot clinical trial. J. Prosthet. Dent. 2018, 119, 560–567.e1.
- Weiss, C.M.; Weiss, A. Implant dentistry nomenclature, classification, and examples. In Principles and Practice of Implant Dentistry; Mosby Incorporated: St. Louis, MO, USA, 2001; pp. 7–16.
- Smith, Y. Procedure for Dental Crowns. Available online: https://www.news-medical.net/health/Procedure-for-Dental-Crowns.aspx (accessed on 11 November 2021).
- Smith, Y. Types of Dental Braces. Available online: https://www.news-medical.net/health/Types-of-Dental-Braces.aspx (accessed on 24 July 2021).
This entry is offline, you can click here to edit this entry!
