Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Out-of-hospital cardiac arrest (OHCA) is a prominent cause of death worldwide. As indicated by the high proportion of COVID-19 suspicion or diagnosis among patients who had OHCA, this issue could have resulted in multiple fatalities from coronavirus disease 2019 (COVID-19) occurring at home and being counted as OHCA.
- out-of-hospital cardiac arrest (OHCA)
- cardiopulmonary resuscitation (CPR)
- emergency medical services (EMS)
1. Introduction
The death toll resulting from the emerging COVID-19 pandemic is expected to be much higher due to the SARS-CoV-2 virus’s direct effect [1,2]. COVID-19 has been linked to a number of time-critical events, including “out-of-hospital cardiac arrest (OHCA)” [3]. In comparison to previous years, a recent comprehensive study found almost a two-fold jump in OHCA rates, prolonged duration for ambulance response, and a 33% drop in the probability of survival of OHCA cases related to the pandemic season [4,5].
COVID-19’s indirect effects on OHCA could have been caused by a variety of reasons. Patients seem to be less inclined to report to a nearby hospital for emergency medical care, particularly in cases of cardiac difficulties, and this has been suggested as a possible cause of higher occurrence [6,7]. This may raise the chances of OHCA [1,4,8]. Ambulance access and operations may potentially alter significantly, including the impact on “ambulance response time” due to changes in emergency medical services (EMS)” caseload and a delayed response in outpatient therapy due to restrictions for paramedics to wear COVID-19 “personal protective equipment (PPE)” [1,9,10]. Overall EMS response to OHCA differed by less than a minute between pre-COVID-19 and COVID-19 time periods [11,12]. In the 2020 group, the average EMS response time to OHCA was 56 s longer. In the 2020 group, the time from the call to emergency medical technician (EMT) departure rose by 39.8 s. Between the two periods, overall transfer times remained similar. EMTs in the 2020 group, on the other hand, stayed longer at the site, implying that the time required for resuscitation in the field was observed to be prolonged in the 2020 group. Figure 1 presents the comprehensive time difference of the prehospital phase between the 2019 and 2020 groups according to Jiun Hao’s research [13].
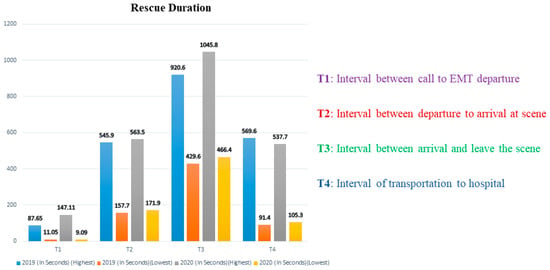
Figure 1. EMT rescue durations for OHCA before and during the COVID-19 pandemic [13].
OHCA is indeed a life-threatening medical issue. The clinical outcomes of OHCA rely heavily on a very good “chain of survival” [14,15]. This aspect of the “chain of survival” entails “bystander cardiopulmonary resuscitation” (BCPR), the utilization of “automated external defibrillators” (AEDs), and “EMS”. The unusual coronavirus pandemic, on the other hand, had an unknown influence on EMS resources. It was thought to have interrupted the “chain of survival” in the prehospital emergency setting, particularly regarding layman or bystander action [2]. From the perspective of OHCA survival, institutional limits on movement may make it less likely for OHCA to manifest in a public setting. As a result, bystander “cardiopulmonary resuscitation” (CPR) and “community defibrillation” are less likely to be performed before an ambulance arrives [16].
Because community and emergency services processes have a greater impact on survival than “advanced hospital-based interventions”, there is a lot of scientific and population health concern about how they were changed. Only those who received prompt prehospital treatments benefited from sophisticated hospital-based interventions [17,18]. Evaluating the COVID-19 pandemic’s influence on OHCA treatment plans is critical for future public healthcare programmes and policies aimed at improving OHCA outcomes after the COVID era is over and for future pandemic emergency advance preparedness.
Research examining the impact of COVID-19 on the “chain of survival,” especially that of early bystander action, has produced mixed results [19,20]. As per studies by Marijon et al., bystanders were even more cautious and unwilling to perform CPR in prospective COVID-19 instances. This was presumably because bystanders were avoiding performing CPR on probable COVID-19 suspected cases [7].
This was especially worrying because BCPR combined with early defibrillation has been shown to increase a victim’s probability of survival [21]. However, some additional studies did not find these results, thus requiring a review of the already published literature on BCPR before as well as during COVID-19. There is also a need to research relevant variables, such as OHCA at home, bystander AED usage, and observed OHCA [22,23]. Prehospital “chain of survival” and EMS treatment plans are also important variables in improving OHCA outcomes. EMS requirements, EMS resuscitation procedures and durations, or the administration of supraglottic airway devices, endotracheal intubation, epinephrine, amiodarone, and mechanical CPR are all examples of advanced life support methods [23].
These characteristics are crucial in the management and care of OHCA patients. It is an early step before they are admitted to the hospital for specialized care [24]. Lim et al. earlier hypothesised that “during the outbreak of COVID-19, EMS call to arrival times were likely to increase given the challenges like heightened personal protective equipment (PPE) requirements” [4]. The influence of COVID-19 on EMS quality care, on the other hand, remains unknown [25].
2. Strategies for OHCA Management during COVID-19
2.1. Need to Reduce Risk Rate for Provider
Due to frequent interaction with symptomatic people, frontline healthcare personnel are at a high risk of developing respiratory diseases [58]. Coronavirus transmission can be reduced with proper PPE, such as N95 masks or “positive air pressure respirators”, mainly throughout “aerosol generating procedures (AGPs)” [83,84]. Individual (e.g., age) and system characteristics might influence provider risk. If their workforce has not been fully vaccinated, healthcare organisations might have to consider redoubling their ability to preserve a decent supply of PPE for AGPs. This is crucial because only complete immunisation of healthcare personnel provides a very low infection rate. CPR comprises AGPs, and healthcare provider vaccination percentages stay below 100%.
Even if healthcare providers obtain resistance to SARS-CoV-2 by vaccination, it is essential for them to continue to take precautionary measures against COVID-19 and its variations. On the other hand, the danger of the patient contracting COVID-19 and developing a serious illness is exceedingly high when compared to the considerably smaller chance of the resuscitation provider contracting COVID-19 and developing a medical condition. This risk is notably low in vaccinated as well as unvaccinated healthcare providers who work with patients while wearing AGP-specific PPE. Although current vaccinations have been shown to be effective against the wild-type SARS-CoV-2 and variations of concern, breakout infections, which are usually not fatal, may still occur. It is possible that boosters addressing developing variations of concern may be needed [85].
2.2. Offer Timely Care and Limit Provider Exposure
Chest compressions must not be deferred in individuals with probable or confirmed COVID-19 who have suddenly stopped breathing [86]. Chest compressions can be conducted using a chest compressor either with or without the use of a surgical mask until rescuers with adequate PPE for AGPs are able to relieve the patient. Chest compressions must not be interrupted for the collection and administration of a mask and face covering for both the patient and the physician given the limited rate of recorded dissemination to health care providers so far. While data in this area are still developing, once compressions have begun and personnel with suitable PPE for AGPs arrive, providers may choose to wear masks [87]. The airway is usually blocked in the unconscious victim with minimal airflow throughout chest compressions unless deliberate attempts are made to keep it open.
Because not every resuscitation room supports “negative pressure ventilation”, locking the door may assist to prevent contamination of nearby indoor places. Taking actions to adequately ventilate a restricted location, including opening windows and doors, may minimise the local accumulation of aerosols for healthcare workers in “out-of-hospital cardiac arrest”. However, if contamination of other sites in immediate proximity is not a concern, this should be performed. Furthermore, certain healthcare companies may continue to face PPE shortages, poor vaccination rates among employees, and staffing constraints.
2.3. Deflection of Respiratory Particles
It is uncertain if defibrillation is an AGP in and of itself. Furthermore, early animal data suggest that chest compressions after defibrillation could produce aerosol [59]. Case-control and “retrospective cohort studies” of many other infectious pathogens dispersed via aerosolization, on the other hand, suggest that the risk of transmission throughout defibrillation is low.
Exhaled respiratory particulate can flow through some oxygen-delivery masks; thus, a surgical mask on something such as a COVID-19 patient may assist in deflecting them [88]. Mask supply, on the other hand, should not potentially prevent life-saving interventions, such as “chest compressions” as well as “defibrillation”, from taking place. An endotracheal tube, supraglottic airway, or a high-efficiency particulate air (HEPA) filter on a ventilator exhaust port can catch aerosolized contaminants when effectively ventilating with bag-mask ventilation [89]. “Endotracheal intubation” should be scheduled when enough PPE-protected workers are available to perform the procedure [90].
2.4. Cardiopulmonary Resuscitation (CPR) and OHCA Management
Cardiopulmonary resuscitation (CPR) in suspected or diagnosed COVID-19 patients requires a different strategy than standard CPR. CPR in COVID-19 patients puts healthcare practitioners at risk [91]. This is due to the procedures that produce aerosols. It necessitates a large number of rescuers working in close proximity, which increases the risk of a personal security violation due to a high-stress occurrence. The most difficult task is to provide COVID-19 victims with the finest potential chance of survival without risking the rescuer’s life. According to the “WHO”, over 22,000 health care workers (HCWs) were exposed to COVID-19 at work around the world, accounting for between 4% and 13% of all affected patients in different countries.
Approximately 548 “HCWs” in India were contaminated by COVID-19, accounting for 1% of all infected cases. Because this can have a substantial effect on the already overburdened healthcare system, the protection of HCWs performing CPR should be prioritised. During the COVID-19 epidemic, many international institutions, including the “American Heart Association (AHA)”, the “International Liaison on Resuscitation (ILCoR)”, and the “UK Resuscitation Council”, issued interim updates and amended resuscitation recommendations. Though most of the suggestions are in agreement, there are variances in specific areas of attention among societies. Furthermore, in resource-constrained settings, it may not be possible to implement all the guidelines. For the purpose of resuscitation of COVID-19 patients, ILCoR performed a thorough study and published its results on science, treatment strategies, and task force findings. As a result, the “European Resuscitation Council (ERC)” has produced COVID-19 guidelines that include some adjustments to current standards that should be addressed during COVID-19 patient resuscitation.
(i) Layperson High-Quality CPR
If cardiac arrest is predicted, telecommunicators must prioritise CPR training for bystanders to provide “hands-only CPR” for an adult patient, including rescue breathing (if ready and interested) for infants and young children. Telecommunicator-CPR can significantly enhance lay rescuer CPR service and maximize a system’s survival.
There is no information on the effects of the strategies used by telecommunicators to include COVID-19 inquiries in suspected OHCA cases [92]. By introducing questions or systematic inquries regarding COVID-19, one may delay or impede lay rescuer service for all OHCA victims. This may generate worry and panic in the rescuer. In contrast, each second that CPR is prolonged, there is a substantial reduction in the chances of survival. As a result, telecommunication programmes should take COVID-19 incidence among OHCA into account [93]. If evidence suggests a prevalence rate, telecommunicators as well as rescuers should focus on chest compressions prior to asking about COVID-19.
2.5. Use of PPE
In an undefined OHCA, it can be difficult to tell whether an individual has COVID-19 or not. The likelihood of contacting a COVID-19-infected person who has had an OHCA will clearly vary depending on the incidence of patients in the community. Furthermore, there is only shaky proof that the most efficient life-saving operation (defibrillation) is an “aerosol generating medical procedure (AGMP)” [94]. As a consequence, reported PPE guidelines vary significantly. For example, before attending the site, all prehospital care workers must put on airborne as well as droplet PPE, or defibrillation can be performed while donning droplet precautionary PPE while, on the other hand, airborne PPE can be used when performing chest compressions as well as ventilation procedures [95]. Finally, regardless of COVID-19 condition, paramedics should put on PPE following local and regional regulations prior to contact with patients in all OHCA cases.
2.6. Advanced Airway Management
All airway procedures are AGMPs with a high risk. As a result, paramedics should use caution when administering airway treatment throughout the COVID-19 pandemic [96]. As per the ability and competence of paramedics, the strategy for airway management must proceed by identifying the most suitable strategy with the lowest total risk of aerosolization. A HEPA filter should be linked to the airway device. The danger of aerosol exposure will be reduced if early advanced airway management is prioritised.
2.7. Mechanical Chest Compressions
“Mechanical chest compression devices” may be a better option than manual chest compressions for individuals who need “prolonged resuscitation” and “chest compressions” during ambulance transport [97]. This reduces the number of people who have to perform chest compressions. As a result, contact with aerosolized particles is reduced. When compared to high-quality human chest compressions, “mechanical chest compression devices” have similar percentages of survivability to hospital discharge. “Mechanical chest compression devices” are not commonly available, and competent use necessitates hands-on training and ongoing expertise [98]. This skill is essential for limiting hands-off time when presenting the device to an OHCA individual. The goal is to keep the chest compression percentage as low as possible. As a result, these devices need only be administered by paramedics who are experts and have practice with them [99].
2.8. Layperson Early Defibrillation
For OHCA patients, defibrillation by laypeople in public places is a successful approach for maximising the survival benefits of early defibrillation. The danger of COVID-19 transmission to lay rescuers is unknown in relation to the use of an “automated external defibrillator” and shock. However, there is some indirect information that can be used to estimate transmission risk. Defibrillation is uncommon among cardiac arrest treatments in that it requires very little patient contact. Rescuers can provide therapy without contacting the patient aside from applying sticky electrodes [92].
2.9. Recommended Guidelines and Suggestions for OHCA during COVID-19
Figure 5 shows the algorithm for OHCA during the COVID-19 pandemic. Comprehensive OHCA management and treatment guidelines would assist paramedics in determining crucial interventions for patients with significantly high chances of survival. These would also restrict interventions for people whose chances of survival are slim. These suggestions may also aid in reducing the strain on hospital limited critical care facilities. Regarding the COVID-19 pandemic, studies propose a balanced strategy for all adult OHCAs with an emphasis on paramedic protection and survival in patients. The following guidelines apply to OHCA with a suspected cardiac cause [99]:
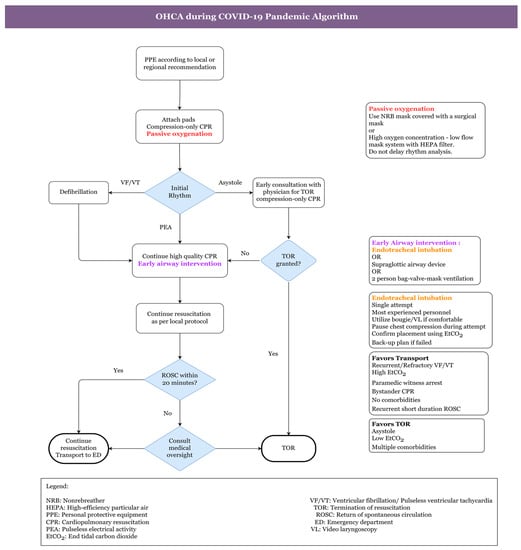
Figure 5. Algorithm for OHCA during COVID-19 Pandemic [99].
-
To begin, the healthcare practitioner should use a surgical mask or fabric to cover his or her own and the patient’s nose and mouth.
-
The absence of “carotid artery pulsations (CAP)”, responsiveness, and normal breathing could all be signs of cardiac arrest.
-
To hear or feel for breathing, healthcare staff should not put their ear or cheek close to the patient’s lips.
-
An ambulance with an “automated external defibrillator (AED)” should be summoned at the same time. Moreover, the healthcare provider should be alerted about the patient’s COVID-19 status and associated hazards. It should also be stated whether the patient is from a hotspot or a cluster location.
-
Then, at a pace of 100–120 per minute, one must start chest compressions in the centre of the chest. No one should use a pocket mask or mouth-to-mouth resuscitation.
-
If an AED is available, the patient should then be defibrillated (according to the rhythm) as quickly as possible to avoid brain damage. Certain measures must be observed during the patient’s travel and arrival.
-
The situation of COVID-19 should be communicated to all new healthcare practitioners who will be in close contact with patients.
-
Before administering CPR on a suspected COVID-19 patient, most recommendations for out-of-hospital cardiac arrest urge that healthcare providers wear full PPE.
-
However, in developing nations, complete PPE might not even be available outside the hospital. In such instances, donning a three-ply mask with a full seal, face shield, facemask, gloves, and a plastic apron are all recommended precautions to take before doing CPR.
-
After donning a face mask, the local caregiver (who could have previously been exposed) should be persuaded to begin CPR.
-
If a telecommunications system is available, caregiver CPR can indeed be performed with the assistance of an HCW who directs and simulates CPR procedures. One must keep in mind that a patient’s face is wrapped with a cloth or mask before beginning CPR. Likewise, after resuscitation, good hand hygiene should be practised by washing hands with soap or a disinfecting alcohol-based gel.
-
Healthcare professionals should also wear PPE kits while transporting patients, whether inside or outside the hospital.
-
A closed circuit must be used to ventilate the patient. High-efficiency particulate air (HEPA) heat moisture exchanger (HME) filters should be included in all ventilator equipment, such as bag valve masks. In ambulances, a PPE kit or at the very least an N95 mask must be supplied. Ideally, ambulances with a separate driver area and a heating, ventilation, and air conditioning (HVAC) system need to be employed. In the ambulance, COVID-19-suspected/confirmed sufferers should not be accompanied by family or friends.
-
They should not ride in the same vehicle as a COVID-19 patient according to the AHA.
-
Furthermore, if return of spontaneous circulation (ROSC) is not obtained in the field, avoid moving the patient to the hospital to prevent additional prehospital and hospital personnel contact with the patient. According to the authors, one family member wearing a face mask can ride in the very same ambulance with the sufferer if he or she has been in direct contact with the patient.
-
If an aerosol-generating technique is required, open the carrying vehicle’s back doors, but do so away from pedestrians.
-
The HVAC system, if accessible, should be turned on. In circumstances where COVID-19 patient ventilation is necessary with a driver in the very same cabin, the outside air vents in the driver section must be opened, and reverse exhaust ventilation should be powered on to generate a “negative pressure gradient” in the patient area.
This entry is adapted from the peer-reviewed paper 10.3390/healthcare11020189
This entry is offline, you can click here to edit this entry!
