2. Acute Kidney Injury and Ultra-Endurance Events
Acute kidney injury (AKI) in ultra-endurance events has been frequently reported [
1], however, the prevalence of AKI in ultra-endurance athletes has not reached a consensus ranging from 0% [
47,
59] up to 85% [
26]. Differing and inconsistent methodologies relying on changes to serum creatinine (SCr) levels, in addition to observing different modalities of ultra-events for measuring the impact on kidney function during ultra-endurance likely explains variances [
3,
56]. Recently 96.2% of AKI cases that also occurred in conjunction with exertional rhabdomyolysis (ER) were linked to ultra-running events [
2]. The majority of studies in this review (
Table 1) pertained to ultra-running events however 3 studies included ultra-cycling participants [
53,
54,
56]. The serum creatinine (SCr) levels for all the participants observed by Chlibkova et al. (2015) in both ultra-mountain bike and ultra-running races increased, however there was a significant increase in post-race SCr for 24 h ultra-running athletes compared to those competing in 24 h mountain biking events (
p < 0.01). It should be noted that very few ultra-athletes seek or need medical intervention in the presence of an AKI diagnosis [
56,
60].
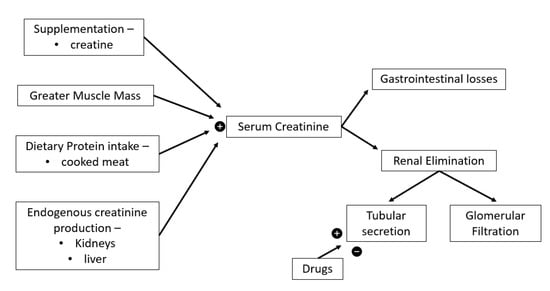
Multiple factors effect SCr levels as seen in
Figure 2. Endogenous creatine production occurs within the liver and kidneys (
Figure 2) from glycine, methionine, and arginine which is subsequently transported to skeletal, cardiac muscles and other tissues [
61] where the non-enzymatic anhydration of creatine results in creatinine [
62,
63]. High protein diets including cooked meats provide an additional creatine source (
Figure 2). Renal elimination of serum creatine occurs via glomerular filtration and low, yet unpredictable levels of tubular secretion, which is affected by multiple drugs, while small gastrointestinal losses also occur [
62,
63] (
Figure 2).
Figure 2. Serum creatinine determinants.

= increase,

= decrease.
Creatinine clearance is a useful indicator of GFR though overestimates it by around 10% compared the gold standard inulin clearance [
62]. Measuring creatinine clearance requires prolonged and impractical urine collection in addition to blood sampling [
62], in clinical practice GFR is usually estimated using equations based on SCr modified by sex, age and ethnicity to provide some degree of correction for differences in creatinine generation [
64]. SCr GFR equations were generated using the general population or hospitalised patients [
65,
66] and assume creatinine generation is steady state, not always true (
Figure 2), especially during or after extreme exercise [
62,
64], as significant increases in SCr levels are common post ultra-events (
Table 1). Severe muscle damage is common during ultra-endurance events [
4] therefore increases in SCr levels can reflect muscle damage rather than reductions in GFR [
8,
52]. Using SCr as an indicator of renal function produces inaccurate reflections of the impact of exercise on kidney function [
67] and may lead to overdiagnosis of AKI in ultra-athletes. Poussel et al. (2020) found using creatinine produced an overestimation of AKI prevalence compared to use the cystatin C. Additionally, the normal GFR for ultra-endurance athletes is unknown due to a lack of baseline data [
68] and back-calculating estimates of baseline SCr for ultra-athletes has been shown to be inaccurate [
43,
68]. Hence, avoiding SCr in settings of extreme exercise has been recommended [
8]. This highlights the importance of pre-race testing, participant screening, and the need for a more accurate and valid method for monitoring renal function for this population.
More accurate biomarkers of renal dysfunction are required which can identify abnormal kidney function and discriminate between intrinsic renal disease and prerenal azotaemia which is often induced by strenuous exercise [
8]. As there are 3 groups of AKI biomarkers: indicators of renal function (low molecular weight proteins such as Cystatin C) [
69], indicators of tubular damage (urinary neutrophil gelatinase-associated lipocalin (NGAL) and urinary kidney injury molecule-1 (KIM-1)) [
8] and renal inflammatory mediators (leukocytes and prostaglandins) [
70]. Cystatin C (Cyst-C) has less non-GFR determinants, being unrelated to muscle mass or diet, compared to SCr [
69,
71,
72] and has been recommended in populations with increased muscle mass or extreme diets [
73]. Over the marathon distance, the rise in Cyst-C was equal to half that of the increase in SCr, supporting that Cyst-C is less affected by sport related renal blood flow changes or muscle damage [
74]. Mccullough et al., (2011) found that there was a comparable rise and normalisation for both SCr and Cyst-C after marathon running. Additionally, this study found a 5-fold increase in NGAL and a lesser increase in KIM-1 measures supporting a real decrease in renal function due to renal tissue injury [
33]. As an 25 kDa acute phase protein, NGAL is mainly produced in the kidney tubules [
8,
47,
48], is a key indicator of early ischemic damage to the kidneys [
75,
76,
77,
78] and early detection of AKI and predicting renal disease progression [
48,
59,
75,
76]. NGAL levels have been shown to significantly increase during then returned to baseline within 24 h [
8] or continued to increase post ultra-race [
33] indicating that tubular injury was present independent of changes to SCr. The minimal increase in urinary neutrophil gelatinase-associated lipocalin (NGAL) and urinary kidney injury molecule-1 (KIM-1) levels in another study also argues against the diagnosis of AKI using criteria based on increased SCr [
47]. Therefore, future studies should compare the sensitivity of available biomarkers while also meetings the practical needs of medical professionals present at ultra-endurance events.
3. Non-Steroidal Anti-Inflammatory Drugs
Five studies reported AKI alongside positive use of NSAIDs for ultra-athletes (
Table 1). In only one study was use of NSAIDs denied by ultra-athletes [
46], whilst the remaining 16 studies did not specify whether there was use of NSAIDs by their participants. NSAIDs inhibits cyclo-oxygenase production thus preventing the synthesis of prostaglandins resulting in increased renal vasodilation and decreasing homeostasis [
25,
77] (
Figure 3). Exercise reduces renal blood flow, however renal perfusion is augmented, and homeostasis maintained via vasodilatory prostaglandins [
78]. The absence of prostaglandins and the subsequent reduced renal perfusion results in reduced GFR contributing to mild increases in renal function markers and ultimately, occasionally, kidney failure [
67,
79]. For healthy individuals, prostaglandin stimulated vasodilation is unnecessary for maintenance of renal function [
78], while those with renal disease requires prostaglandin driven vasodilation of renal vascular beds to maintain renal perfusion [
80] and avoid renal ischemic injury [
78].
Figure 3. Multiple pathologies and mechanisms promoting acute kidney injury (AKI) in ultra-endurance athletes. Non-steroidal anti-inflammortory drugs (NSAIDs), glomerular filtration rate (GFR), exertional rhabdomyolysis (ER), myoglobin (MB), serum creatine kinase (S-CK), arginine vasopressin (AVP), exercise-associated hyponatremia (EAH),

= increase,

= decrease.
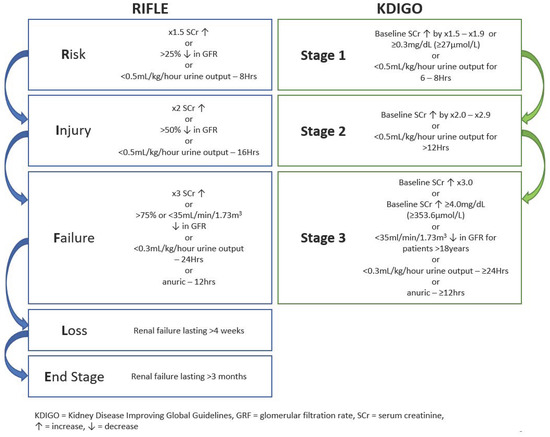
Compared to marathon (42 km) and trail runners (67 km), ultramarathon runners (112 km) had the highest per-event NSAIDs intake indicating that the duration of the event plays a role in the quantity and chronological consumption of NSAIDS in ultra-events [
17]. Although NSAIDs have been found to be a significant risk factor for AKI after endurance events, some debate exists regarding whether NSAIDs induce a reduced renal function in ultra-athletes. Wharam et al., (2006) found that NSAIDs significantly increase SCr compared to non-NSAIDs users. More recently, Lipman et al., (2014) showed a 18% increase in overall AKI incidence and severity for NSAIDs users, as 12% more ultra-athletes met the AKI at-risk criteria and 6% more met the injury criteria (
Figure 1) [
14]. Poussel and colleagues found that observing only non-NSAIDs user ultra-athletes reduced the incidence of AKI compared to other ultra-athlete studies [
59]. However, contrary evidence exists as both Dumke et al. (2007) and Page et al. (2007) found no significant difference in SCr levels between NSAID using and non-using ultra-runners, though both sample sizes were small, the NSAIDs doses subtherapeutic, and the studies were unblinded.
In the 11 case reports systematically reviewed by Hodgson et al. (2017) investigating the concern of severe AKI after various marathon and ultramarathon events, 22 of 27 cases of severe AKI in ultra-athletes required hospitalisation, 18 (67%) reported NSAIDs use. In the studies discussed in this review (
Table 1) no renal biopsies were completed, although 1 case of acute tubular necrosis (ATN) was made from urinalysis, serology, and ultrasound results [
58]. However, in studies reviewed by Hodgson et al., (2015), 4 kidney biopsies were completed, all revealing ATN for both marathon and ultramarathon distance events, suggesting an ischaemic aetiological link in developing AKI and ATN for endurance athletes using NSAIDs [
8]. NSAIDs have also been linked to the development of EAH and ER in ultra-athletes which may also contribute to subsequent AKI and hospitalisation [
34,
60]. Ultra-athletes should approach the consumption of NSAIDs with caution and pay closer attention the potential negative health outcome, especially the development of AKI and ATN rather than performance benefits.
4. Hydration
Ultra-endurance events occur across the world and expose athletes to a multitude of different and fluctuating environmental conditions including hot, humid, tropical conditions [
4,
26,
34,
35,
81]. Physical exertion in these ambient conditions often promotes kidney damage and ultra-athletes often experience inadequate hydration status [
39,
81,
82]. Altered kidney function is promoted due to combinations of dehydration, high internal and external metabolic loads, and heat strain [
24,
83]. Severe dehydration is widely recognized as a contributor to AKI after endurance exercise and other life-threatening consequences [
23,
24]. Increased loss of electrolytes and water via increased sweating can also cause hyponatremia [
34,
56]. While adequate hydration status maintenance does not prevent ER in ultra-athletes [
26], dehydration induced reduction of renal blood flow and renal ischemia resulting in an accumulation of muscle proteins within a reduced total blood volume can increase the risk AKI [
84,
85] and ER [
86,
87] for ultra-athletes (
Figure 3).
Loss of body mass does not directly translate into an absolute measure of dehydration however it is a simple method of assessing hydration status during exercise [
88]. Previous studies have found that limiting the body exercise induced weight loss to ~2–3% is necessary to avoid dehydration while maintaining or improving performance [
89,
90,
91]. The average body weight loss for ultra-marathon runners was ~5%, reaching >11% of body weight in some cases [
26,
92]. Water can be produced during exercise via a combination of the utilisation of endogenous and exogenous substrates and the release of glycogen bound water through glycogenolysis [
91] assisting in alleviating dehydration [
93]. Therefore, maintaining euhydration requires at least ~2–5% reduction in body mass during ultra-events [
91], which seems to be tolerated by ultra-athletes [
94]. Belli et al., (2018) found that athletes who presented with body mass reductions >5% (−5.2 to −10.4%) also presented with >25% (−27.1 to −44.4%) reduced GFR from 84 km to the completion of the 200 km event. Similarly, a greater reduction in body mass from 120 km was linked to greater renal dysfunction for ultra-athletes during multi-stage 250 km desert races [
25]. Hence, complying with typical hydration guidelines and avoiding a 2% mass loss [
30,
95], can result in hyperhydration of ultra-athletes [
82], increases the risk of developing symptomatic EAH [
96], and increased levels of cytokinemia and bacterial endotoxemia and subsequent increased AKI risk [
97]. Dehydration is most likely to occur during the early stages of ultra-events as the first 4 h showed the maximum slope of weight loss [
25,
26,
46]. However, an increased total percentage body mass loss resulted in a higher proportion of subjects meeting RIFLE criteria for AKI compared to those with less mass loss [
39,
57] and therefore needs further investigation.
5. Exertional Rhabdomyolysis
Exertional rhabdomyolysis (ER) is a pathophysiological condition described by damage to or necrosis of the striated muscle tissues during strenuous exercise leading muscle cell disintegration enabling the release of myoglobin (Mb) into the bloodstream and extracellular space [
98]. Additionally, sarcoplasmic proteins such as S-CK, serum lactate dehydrogenase (S-LDH), aspartate transaminase (AST) and electrolytes are released [
99]. In extreme cases of muscle necrosis, ER symptoms can present as weakness, oedema, myalgia, and reddish-brown or tea coloured urine, without haematuria [
34]. Six papers were found discussing exertional rhabdomyolysis in ultra-endurance events resulting in 43 cases (
Table 1). Of these, 30 cases of AKI occurred either alongside or potentially due to exertional rhabdomyolysis (ER).
Serum Mb can potentially result in kidney failure via 3 mechanisms: tubular obstruction, toxic reaction, and decreased oxygen supply due to vasoconstriction of renal tissues [
60,
87] (
Figure 3). Mb is quickly eliminated from the bloodstream, so S-CK is the preferred marker for ER identification [
23] which shows a peak 24–36 h post-exercise with recovery to baseline values at 48–72 h post-exercise [
100,
101,
102]. In ER, Mb and S-CK, can rise ≥4–5 times and sometimes much greater, above normal values, while S-LDH and AST generally only double [
103]. A recent systematic review recommended that S-CK > 1000 UI/L as an essential criterion for the diagnosis of ER diagnosis [
104].
With an incidence of ~29.9 per 100,000 patient years, ER is relatively uncommon [
105] however the concurrent complication of AKI which is significantly more common is a concern for ultra-athletes [
86]. Hodgson et al. (2017) reported 27 cases of AKI across varying endurance disciplines (six in ultra-endurance athletes), with concurrent rhabdomyolysis in 23 cases (85%). Not surprisingly ER can lead to several other serious conditions, hyperkalaemia, hypernatremia, acidosis kidney tubule damage and the development of acute and chronic renal injuries [
4]. ER due to heat stress and AKI has been reported, indicating that dehydration, hyperthermia, and eccentric muscle loads can promote and contribute to the development of ER + AKI [
23,
39]. As ultra-endurance events are often held in areas with hot and humid conditions for example the tropics, these conditions can increase the risk of ER [
26,
34,
87]. It has been shown that increasingly prolonged exercise under these thermally challenging conditions can induce increased severity of both ER and AKI [
4].
 = increase,
= increase,  = decrease.
= decrease.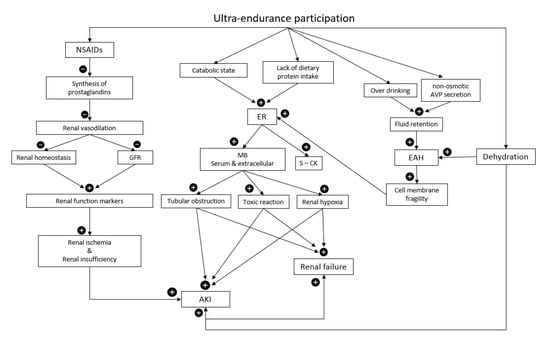
 = increase,
= increase,  = decrease.
= decrease.