You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Clinical Neurology
Stroke and cancer are disabling diseases with an enormous global burden, disproportionately affecting vulnerable populations and low- and middle-income countries. Both these diseases share common risk factors, which warrant concerted attention toward reshaping population health approaches and the conducting of fundamental studies.
- stroke
- cancer
- thrombosis
1. Introduction
Stroke is a debilitating disease with a significant morbidity burden on individuals and ever-increasing costs imposed on public health systems worldwide [1]. It stands as the second leading cause of disability-adjusted life years (DALYs) globally, with a disproportionate number of stroke-related deaths and DALYs precipitating in low- and middle-income countries (LMICs) [2]. Within Australia, a 2020 report released by Deloitte found the economic impact of stroke to be 6.2 billion Australian dollars in direct financial costs, with a further 26 billion dollars attributable to premature mortality and DALYs [3]. A similarly dire picture exists for cancer, which accounts for almost 10 million deaths worldwide each year [4]. Estimates by the International Agency for Research on Cancer (IARC) suggest that the total cost of cancer amounts to USD 1.16 trillion annually, with LMICs again disproportionately impacted, despite having lower rates of cancer, as a majority of deaths are accounted for in socioeconomically disadvantaged areas [5]. Given this substantial burden posed by stroke and cancer individually, and the various shared risk factors in the pathophysiology of cancer and stroke, such as dyslipidemia, diabetes mellitus, and hypertension, the heightened stroke risk in cancer patients, especially those undergoing radiation therapy [6], these two diseases become an even more pertinent issue to address [7].
2. The Burden of Stroke and Cancer
Table 1 provides an overall assessment of burden, prevalence, DALY, and financial burden in stroke, cancer, and cancer-associated stroke. Much needs to be accomplished to reduce the global financial burden of cancer and stroke and the life-changing impact it has on the patients themselves. Of particular concern is the inordinate burden that LMICs face, where despite having lower rates of cancer, a majority of deaths are accounted for in these socioeconomically disadvantaged areas. A similar parallel is drawn in the context of stroke, whereby an unfair 87% of DALYs are lost within LMICs [8]. More robust education, screening, availability, and accessibility of treatment must all be addressed in order to reduce these gaps.
Table 1. Stroke in Cancer stratified by the burden of disease, prevalence, DALYs, and financial burden.
| Burden of Disease | Prevalence | DALY | Financial Burden | |
|---|---|---|---|---|
| Stroke | In Australia [9]: 2.7% of the total burden of disease (2015) 38,000 incident cases (2017) 27,428 incident cases (2020) Globally [2]: 12.2 million incident cases (2019) 2nd leading cause of death, 11.6% of total deaths (2019) LMICs [8]: 70% of strokes and 87% of stroke-related deaths occur in LMICs (2017) |
In Australia: 387,000 stroke survivors (2018) [10] 445,087 stroke survivors (2020) [3] Globally [2]: 101 million stroke survivors |
In Australia: 4.6 DALYs per 1000 population (2015) [11] = 118,220 DALYs across the Australian population (2015) * 398.22 DALYs/100,000 population (2021) [12] = 102,342 DALYs across the Australian population (2021) * Globally [2]: 143 million DALYs, 5.7% of total DALYs (2019) LMICs: 87% of DALYs occur in LMICs [8] |
In Australia: AUD 633 million was spent on health system expenditure (2015–16) [13] AUD 6.2 billion in direct financial costs (2020) [3] AUD 26 billion in lost well-being and premature mortality (2020) [3] Globally: Worldwide data N/R In the EU: EUR 27 billion in health system expenditure, EUR 1.3 billion in cost for informal care, EUR 12 billion in lost productivity (2017) [14] In the US: USD 156.8 billion in total cost, $103.5 billion in indirect costs, USD 38.1 billion from productivity loss, and USD 30.4 billion from premature death (2020) [15] |
| Cancer | In Australia [16]: 151,000 new diagnoses (2021) Estimated that 43% will be diagnosed with cancer by the age of 85 Globally: 23.6 million new cancer cases (17.2 excluding nonmelanoma skin cancer) (2019) [17] |
In Australia [16]: 456,978 people living (who had been diagnosed with cancer) at the end of 2016 (diagnosed in 2012–2016) 1,176,285 people living (who had been diagnosed with cancer) at the end of 2016 (diagnosed from 1982 to 2016) Globally [17]: 85.8 million cases (2019) LMICs: 65% of all cancer deaths occurred in LMICs (2012), projected to be 75% in 2030 [18] Projection of 75% of the world’s cancers to occur in LMICs by 2040 [17] |
In Australia [16]: 18% of total burden (2018) 881,094 DALYs (2018) Globally [17]: 250 million DALYs (2019) |
In Australia: 9% of health system expenditure (2021) AUD 6.3 billion in yearly cost to the Australian healthcare system (for Australians diagnosed in 2009–13) (2013) [19] Globally: Worldwide data N/R In the EU: EUR 199 billion in total cost of cancer, EUR 103 billion on health expenditure on cancer care (including EUR 32 billion on cancer drugs), EUR 26 billion in informal care, EUR 70 billion in total productivity loss (EUR 50 billion from premature mortality, EUR 20 billion lost due to morbidity) (2018) [20] In the US: estimates of USD 161.2 billion on healthcare spending, USD 30.3 billion spent on productivity loss due to morbidity, USD 150.7 billion lost to premature mortality (2017) [21,22] |
| Stroke in Cancer | Country-specific data N/R A US population-based study of 7,529,481 patients found the risk of fatal stroke to be 21.64 per 100,000-person-years. Standardized mortality ratio is 2.17 (95% CI, 2.15–2.19) (2019) [23] |
In Australia: Total number of cases of stroke in cancer (2019) = 0.06 × 456,978 = ~27,419 * Globally: The rate of non-fatal strokes in cancer patients is 5%, rate of fatal strokes in cancer patients is 1%. The combined rate of fatal plus non-fatal stroke is 6% for cancer cohort [23]. Total number of cases of stroke in cancer (2019) = 0.06 × 85.8 million = ~5.148 million * |
In Australia: Total number of DALYs due to stroke in cancer (2011) = 0.06 × 833,250 = ~49,995 * Globally: Global DALYs due to stroke in cancer (2019) = 0.06 × 250 million = ~15 million * |
In Australia: 0.06 × USD 6.3 billion of direct costs = ~USD 378 million of Australian health system expenditure on stroke in cancer (2013) * |
2.1. Burden of Stroke
Stroke afflicts millions of individuals worldwide, with estimates from the 2019 GBD study estimating 12.2 million incidents and 101 million prevalent cases [2]. Ischaemic stroke accounted for 62.4% of incidences, 27.9% by intracerebral hemorrhages, and 9.7% by subarachnoid hemorrhages. Furthermore, 6.55 million deaths occurred due to stroke. Though rates of stroke incidence, prevalence, mortality, and DALY rates declined in the last few decades, the absolute number of individuals developing stroke, dying, or becoming disabled from stroke doubled. This is cause for further concern given that most of the stroke burden occurs in LMICs, which shoulder 80% of incident strokes, 87% of deaths, and 89% of all stroke-related DALYs [24]. Currently, inadequate gaps in the care of stroke in LMICs include longer waiting times in the emergency department, a paucity of equipped stroke-dedicated units, funding deficiencies/financial difficulties in purchasing potentially lifesaving trans plasminogen activator (tPA), and under-established secondary prevention public health promotion strategies [25].
Within the context of Australia, in 2018, the Australian Institute of Health and Welfare (AIHW) estimated 387,000 prevalent stroke cases, declining from 1.7% in 2003 to 1.3% in 2018 [10]. Stroke incidence in 2017 came to approximately 38,000, falling 24% from 2001 to 2017. Stroke as the underlying cause of death accounted for 8400 lives lost in 2018-5.3% of all deaths that year. Death rates from stroke also fell by 75% from 1980 to 2018. These all point toward improved prevention, treatment, and post-stroke care within the Australian health system.
Disparities exist within Australia as well, with Aboriginal and Torres Strait Islander peoples experiencing higher rates of stroke in comparison to non-Indigenous Australians, being 1.6 times more likely to be hospitalized for a stroke and disproportionately accounting for 2.3 times the overall burden of disease [26]. Geographical disparities in stroke diagnosis and care are another important factor mediating access and outcomes after stroke [27,28,29,30]. Stroke hospitalization rates are reportedly higher in remote and very remote areas in comparison to major cities, indicating various gaps of insufficient care due to increased travel times, lack of education, and greater limitations in supplies and available treatment [10]. Finally, the burden of stroke is more pronounced across lower socioeconomic areas relative to those from the highest areas.
2.2. Burden of Cancer
Cancer remains a leading cause of death worldwide, with the International Agency for Research on Cancer (IARC) estimating 19.3 million new cancer cases worldwide in 2020, alongside 10 million deaths from cancer [11]. The combination of an aging global population with an increasing lifespan, and ever-worsening environmental risk factors thus mean that the burden of cancer will only increase in future years. In Australia, estimates from the AIHW show that in 2021, there were 151,000 new cancer diagnoses, and 49,000 deaths [16]. Furthermore, 9% of the entire health system expenditure is attributed to cancer, with estimates from the 2015–2016 period culminating in an overall AUD 10.1 billion expense, with AUD 9.1 billion spent on diagnosis and treatment, and AUD 409 million on the nationwide bowel, breast, and cervical screening programs [16]. Though cancer mortality and diagnosis rates are trending downward due to vast improvements in screening programs and cancer care, discrepancies exist across the Australian population regarding both cancer diagnosis and mortality. Upon comparing Indigenous and non-Indigenous populations, the former group is 14% more likely to be diagnosed with cancer in their lifetime, and 20% less likely to survive 5 years after diagnosis. This gap continues in terms of the hospital care received, whereby Indigenous people accounted for a higher proportion of public hospital admitted care, at 73% vs. 52%, whilst 33% of non-Indigenous people receive care in private hospitals compared to 6% of Indigenous people [31]. This calls into question the disparity in care received, ability to access cancer specialists, and novel clinical trials—all of which might improve prognosis.
Geographical differences, especially in indigenous populations, also mediate outcomes after cancer [32]. Survival after cancer diagnoses declines with increasing remoteness (55% in very remote areas, 63% in major cities), in part, reflecting the poorer survival rates for Indigenous Australian populations also who reside in remote areas [16]. Incidence of diagnosis for the common cancers of lung cancer and head and neck cancer also increases with remoteness, with breast cancer being the main exception, with cases highest in major cities at 127 cases per 100,000 females vs. 89 cases per 100,000 females in very remote areas [16].
Social determinants of health also impact the entire continuum of cancer care [16]. The relationship between cancer incidence and the socioeconomic area was also detailed, with age-standardized incidence rates tending to increase with one’s disadvantage, consistent for colorectal, lung, head and neck, kidney, pancreatic, liver, cervical, and uterine cancers. However, for breast and prostate cancers, incidence rates decrease with increasing disadvantage. However, regardless of cancer, the 5-year observed cancer survival rate is consistently highest in areas of least disadvantage. From 2012 to 2016, individuals had a 56% 5-year survival rate when combining all cancers, compared to 68% in areas with the least disadvantage. This corresponds with cancer mortality rates, whereby there are 185 in 100,000 deaths in the most socioeconomically disadvantaged areas, vs. 130 per 100,000 in the least disadvantaged [16].
This mismatch is further exacerbated and exposed on a worldwide scale. Across the globe, the interplay between socioeconomic status and cancer risk is also of particular concern (Table 1). The 2019 JAMA Global Burden of Disease (GBD) study revealed that whilst 50% of cancer cases occur in high socio-demographic index (SDI) countries, these countries account for only 30% of cancer deaths, 25% of cancer DALYs, and 23% of cancer years of life lost (YLLs) [17]. This points to the current disparity in the burden experienced between developed and developing countries, whereby countries with limited resources are inadequately equipped in comparison to the rest of the globe with regards to screening programs, immunization, and cancer care, all of which would decrease this burden. The case of cervical cancer most adroitly explores this inequality, whereby country SDI plays a major role, as preventable cancer with a well-established, cost-effective vaccination and screening programs available, incidence rates are falling at slower rates in low SDI countries due to insufficient financial resources to instigate comprehensive screening [33].
The COVID-19 pandemic also caused major disruption to the standard processes of cancer screening, treatment, and care [34,35,36]. The reduction in resources and access to healthcare only served to exacerbate already existing disparities between urban and remote populations, and those who are socioeconomically disadvantaged [36].
3. Risk Factors for Stroke in Cancer
Though individual entities, the interactions between cardiovascular disease (CVD) and cancer are complex and suggest a shared pathophysiology, in particular, chronic inflammation [7]. A retrospective analysis of 1274 stroke patients, in which 12% had an additional cancer diagnosis, the researchers identified cerebrovascular risk factors for cancer patients as hypertension, atrial fibrillation, coronary vessel disease, smoking, hypercholesterolemia, and diabetes mellitus, which is in line with those of non-cancer populations.
Conditions such as obesity, hyperglycemia, hypertension, and hypertriglyceridemia, which are linked with CVD, are of particular significance due to their inflammatory effects [37]. As inflammation underpins each stage of atherosclerosis, atherosclerotic emboli are thus implicated in stroke risk within cancer patients, with conditions such as hypertension, smoking, dyslipidemia, and insulin resistance contributing toward the progression of atherosclerosis. Within cancer, the role of inflammation is also clear, with multiple cancer phenotypes triggered by an infection or chronic inflammatory diseases, such as human papillomavirus and cervical cancer, H. pylori and gastric cancer, and Epstein–Barr virus and lymphoma [9].
Cancer patients also face unique risk factors that contribute toward cerebrovascular events; namely the direct tumor effects, cancer-induced coagulation disorders, and the impact of radiotherapy and chemotherapy must be considered. The multi-faceted avenues by which stroke can occur in cancer patients are illustrated in Figure 1.
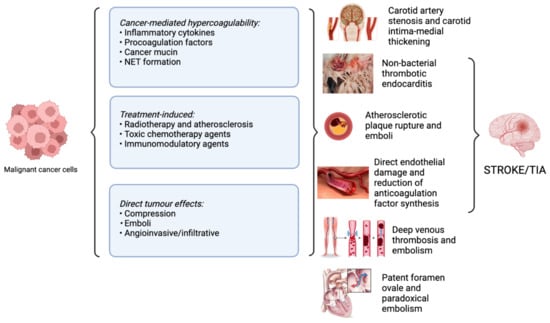
Figure 1. Overview of pathophysiological mechanisms of stroke in cancer patients. Abbreviations: NET: neutrophil extracellular trap; TIA: transient ischemic attack.
This entry is adapted from the peer-reviewed paper 10.3390/ijms232415769
This entry is offline, you can click here to edit this entry!
