Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Artificial Intelligence (AI) appears to be making important advances in the prediction and diagnosis of mental disorders. Researchers have used visual, acoustic, verbal, and physiological features to train models to predict or aid in the diagnosis, with some success. However, such systems are rarely applied in clinical practice, mainly because of the many challenges that currently exist.
- artificial intelligence
- depressive disorder
- mental disorder
1. The Rationale for Using Machine Learning to Identify Mental Disorders
Since the term “mental disorder” includes different categories with high heterogeneity, the researchers mainly use the most common category of mental disorders, depressive disorders, as an example in the present research. Previous studies have found differences between depressed patients and the healthy population. These can include biochemical indicators such as blood oxygen consumption in the brain [1], neurotransmitters [2], and EEG [3], peripheral physiological signals [4] such as heart rate, skin conductance, etc., and non-verbal behaviors [5] such as facial expressions and voice features, the language used (verbal or textual), etc. The features that differ between the two groups (those with and without a depressive disorder) serve as basic AI classifiers. Therefore, by using these discriminant metrics as feature inputs for machine learning, it should be possible to train good predictive models for automated depressive disorder diagnosis.
Many studies have used nonverbal behaviors to predict depression, especially facial expressions [6][7], which are the most salient of behaviors and are considered to accurately display mood (as depressive disorders are mood disorders). The researchers chose facial cues as an example for the present research, but the application of other cues can be found in certain survey articles [1][8][9]. Facial expressions, usually categorized as expressing anger, sadness, joy, surprise, disgust, fear, etc., are regarded as discriminative cues for depressive disorder detection. Those diagnosed with a depressive disorder often demonstrate little expressiveness in their facial expressions [10]. Gavrilescu et al. proposed the determination of depression levels by analyzing facial expressions via the Facial Action Coding System. The experiment obtained 87.2% accuracy for depression identification [11]. Furthermore, the duration of spontaneous smiles [12], smile intensity [12][13], mouth animation [14], and lack of smile [15] have also been considered to offer valuable patterns for depressive disorder detection. In recent years, the use of facial expressions as cues for depression recognition has made great progress. Effective facial features can now even include pupil changes. For example, a recent study considered faster pupillary responses to represent a positive healthy control [16]. Depressed subjects demonstrate slower pupil dilation responses in certain conditions [17]. One study found that pupil bias and diameter were important for assessing the symptoms of depression [18]. Features consist of reduced eye contact [15], gaze direction [13], eyelid activity, and eye movement and blinking [19].
Single modal (such as only facial cues) depressive disorder recognition has also been found to yield positive results. Theoretically, multimodal data should be able to further enhance the effect, such as when voice and visual cues are combined as feature input, and the addition of physiological information should further enhance the accuracy of automatic diagnosis. Multimodality is a prominent direction of both algorithm development and database development.
Researchers use visual, acoustic, verbal, and physiological signals to make predictions, so what exactly are the characteristics of these diseases they are attempting to predict? What is the diagnostic process followed by clinicians? Do these issues pose challenges to AI that are different from those seen with other tasks?
The researchers use the example of depressive disorders to illustrate the challenges of using AI to diagnose mental illness. The DSM-5 [20] or ICD-11 [21] are the most authoritative diagnostic manuals available. However, even the DSM, the most widely used standard, is highly controversial. Next, the researchers will discuss the features of depressive disorders that may pose a barrier to using AI diagnosis.
2. Challenges from Diagnostic Criteria
First, many diagnostic indicators are based on subjective experiences or qualitative descriptions or are difficult to objectively quantify and standardize. Diagnostic criteria for depressive disorders are based on symptomatology, such as a depressed mood or sleep problems. Although many scholars pursue a physiological basis or biomarkers, there are no clinically useful diagnostic biomarkers that are able to absolutely confirm a diagnosis of major depressive disorder.
Second, individuals vary greatly in their presentation of symptoms (see Figure 1). According to the DSM-5, the two most important core symptoms of major depressive disorder are (1) a depressed mood most of the day and/or (2) markedly diminished interest or pleasure. At least three or four more of the other seven need to be met to be diagnosed with a depressive disorder, meaning that depressive disorders themselves do not have consistent symptoms and vary greatly among individuals. The PHQ-9 (Patient Health Questionnaire-9) is an assessment of the nine criteria in the DSM-5. Another widely used scale, the HAMD, does not focus on typological symptoms (i.e., insomnia, low mood, agitation, anxiety, and reduced weight). In addition, differences in symptoms exist across developmental stages. For example, depressive symptoms in adolescents tend to manifest as irritability and not necessarily in a constant low mood. There exist, at fewest, 1497 unique profiles for depression [22]. In some cases, patients with the same diagnosis may not share any identical symptoms [23].
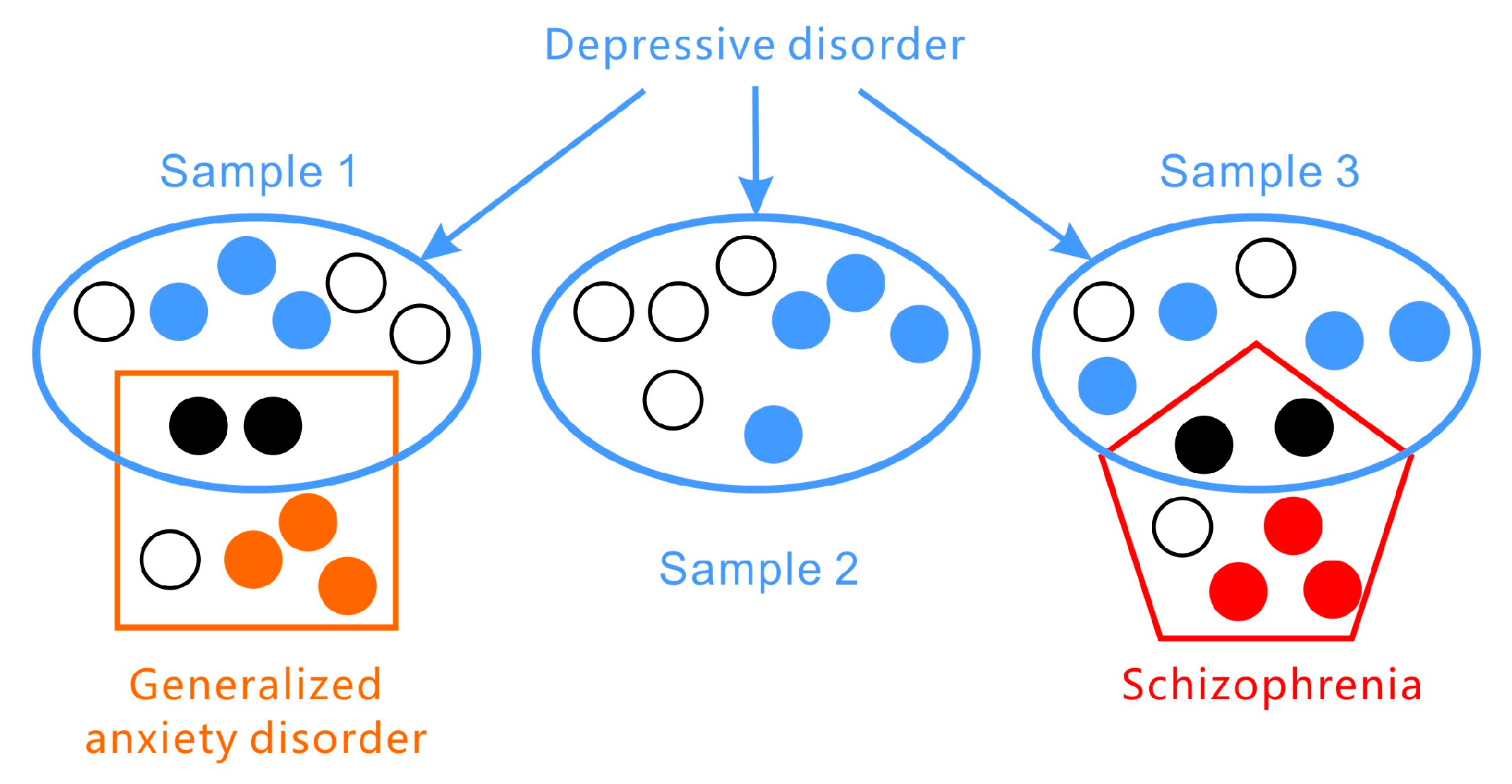
Figure 1. Depressive disorders vary greatly in their presentation of symptoms and are co-morbid with other disorders (such as generalized anxiety disorder and schizophrenia).
Third, depressive disorders comprise a collection of ailments with many subcategories and variants, such as disruptive mood dysregulation disorder, major depressive disorder, and persistent depressive disorder.
Fourth, co-morbidities are very common in mental disorders (see Figure 1). Depressive disorders may be accompanied by anxiety and personality disorders and are often confused with bipolar or other mental disorders. Such illnesses may be very similar or identical to particular depressive disorders in terms of symptoms (e.g., sleep or appetite problems) but require differential diagnoses by clinicians. This issue often results in subjective bias [24][25][26][27][28].
Fifth, the symptoms should lead to impaired social functioning according to DSM. They are expected to cause clinically significant distress or impairment in social, occupational, or other important areas of functioning that are culturally related.
Sixth, the symptoms are not static and not always displayed. Major depressive disorder is not continuous, but rather episodic. For example, some people feel more serious in the morning on one day and remain depressed for several weeks.
Seventh, depressive disorders manifest in interactions between genetic issues and environmental, physiological, and sociocultural factors. The pathogenesis of depressive disorders has not yet been unilaterally agreed upon. Depression is not just a neurophysiological problem. It depends on the interaction between a genetic predisposition and environmental factors [29]. The combination of biological elements, family and environmental stressors, and personal vulnerabilities plays a vital role in affecting the onset of major depressive disorder [30]. This makes the subjective experience of depression and the behavioral and speech characteristics of depressed individuals very different.
3. Challenges from Standard Diagnostic Approaches
Then, how do clinicians diagnose depressive disorders, considering the variability of such characteristics?
As described above regarding the qualities and diagnostic criteria of depressive disorders, there is no unique and efficient clinical set of indicators, making the diagnosis of depressive disorders time-consuming and inherently subjective [31]. Routine assessments include self-rating scales and clinician-based interviews. Both such assessments are mainly based on the DSM and ICD. Self-rating scales are a simple and convenient way to assess depressive disorders; examples include the PHQ-9, Zung’s Self-rating Depression Scale, and the Beck Depression Self-Rating Scale. The results are most often used for screening and providing a reference for physicians’ diagnoses. Self-rating scales have been used widely in various studies, with specificity and sensitivity reaching up to 80% to 90%, though there are certain problems [32]. In addition to self-rating assessments, other rated scales such as the Hamilton Rating Scale for Depression [33] are often also used to assist clinicians’ diagnosis.
Clinical interviews are more professional and accurate but also more time-consuming and laborious. Doctors’ interview-based assessments comprise the final decision stage for diagnosis. Diagnosing depressive disorders can be complicated, depending not only on the educational background, cognitive ability, and honesty of the subject describing their symptoms but also on the experience and motivation of the clinician. Comprehensive information and thorough clinical training are needed to accurately diagnose the severity of depression [34]. Some biological markers such as low serotonin levels [35], neurotransmitter dysfunction [36], and brain structure [37] have been considered to be indicators of depression.
Depressive disorders are so complex that the diagnostic process must be considered holistically. Because depressive disorders are not just mood problems but also sociocultural in nature, they are often accompanied by a serious impairment of social functioning. This may explain why the misdiagnosis rate is high for clinicians. It requires people to rethink the current depression dataset and ask whether the samples are representative and qualified. Can the objective features recorded predict depressive disorders? Are the annotations valid?
4. Challenges from the Logical Fallacy of Mental Disorder Diagnosis
When a clinician diagnoses a person as having a depressive disorder, they rely on the symptoms reported by the client, such as a persistent low mood for two weeks and frequent suicidal thoughts. What is the cause of the persistent low mood? The usual answer is that the individual is suffering from a depressive disorder. Depressive disorders cause the corresponding symptoms, which is the premise of conditional reasoning: If p then q. Diagnosing disorders by symptoms requires the reasoning of affirming the consequent: If q then p. This is a logical fallacy (Table 1).
Table 1. The four formats of conditional reasoning.
| Logical Format | Diagnosis | Logical Value |
|---|---|---|
| DD *→DS ** Modus Pollens | If depressive disorder then depressive symptom | Valid |
| Non-DD→non-DS Denying the antecedents | If no depressive disorder then no depressive symptom | Invalid |
| DS→DD Affirming the Consequent | If depressive symptom then depressive disorder | Invalid |
| Non-DS→non-DD Modus Tollens | If no depressive symptom then no depressive disorder | Valid |
* DD = depressive disorder; ** DS = depressive symptom.
Depressive disorders are labels for sets of symptoms. This means that symptoms do not explain why a person has a depressive disorder, nor does the disorder explain why the symptoms occur. Therefore, it is implausible to identify whether a person has a depressive disorder from the symptoms they present. A person may be depressed because they have been experiencing negative stimuli for the past several weeks. If the negative stimuli disappear, so might the negative mood. On the other hand, they may be depressed because of another psychological disorder, such as a personality disorder.
The researchers are not yet sure of the relationship between depressive disorders and the set of symptoms, which causes significant problems with diagnosis. If AI tries to imitate clinicians, it will face the same challenge.
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics13010002
References
- Wang, L.; Hermens, D.F.; Hickie, I.B.; Lagopoulos, J. A systematic review of resting-state functional-MRI studies in major depression. J. Affect. Disord. 2012, 142, 6–12.
- Pan, J.-X.; Xia, J.-J.; Deng, F.-L.; Liang, W.-W.; Wu, J.; Yin, B.-M.; Dong, M.-X.; Chen, J.-J.; Ye, F.; Wang, H.-Y. Diagnosis of major depressive disorder based on changes in multiple plasma neurotransmitters: A targeted metabolomics study. Transl. Psychiatry 2018, 8, 1–10.
- Lee, H.S.; Baik, S.Y.; Kim, Y.-W.; Kim, J.-Y.; Lee, S.-H. Prediction of antidepressant treatment outcome using event-related potential in patients with major depressive disorder. Diagnostics 2020, 10, 276.
- Ellis, A.J.; Vanderlind, W.M.; Beevers, C.G. Enhanced anger reactivity and reduced distress tolerance in major depressive disorder. Cogn. Ther. Res. 2013, 37, 498–509.
- Fiquer, J.T.; Moreno, R.A.; Brunoni, A.R.; Barros, V.B.; Fernandes, F.; Gorenstein, C. What is the nonverbal communication of depression? Assessing expressive differences between depressive patients and healthy volunteers during clinical interviews. J. Affect. Disord. 2018, 238, 636–644.
- Pampouchidou, A.; Simos, P.G.; Marias, K.; Meriaudeau, F.; Yang, F.; Pediaditis, M.; Tsiknakis, M. Automatic assessment of depression based on visual cues: A systematic review. IEEE Trans. Affect. Comput. 2017, 10, 445–470.
- Lee, Y.-S.; Park, W.-H. Diagnosis of Depressive Disorder Model on Facial Expression Based on Fast R-CNN. Diagnostics 2022, 12, 317.
- Li, X.; Zhang, X.; Zhu, J.; Mao, W.; Sun, S.; Wang, Z.; Xia, C.; Hu, B. Depression recognition using machine learning methods with different feature generation strategies. Artif. Intell. Med. 2019, 99, 101696.
- Wu, P.; Wang, R.; Lin, H.; Zhang, F.; Tu, J.; Sun, M. Automatic depression recognition by intelligent speech signal processing: A systematic survey. CAAI Trans. Intell. Technol. 2022.
- Jones, N.P.; Siegle, G.J.; Mandell, D. Motivational and emotional influences on cognitive control in depression: A pupillometry study. Cogn. Affect. Behav. Neurosci. 2015, 15, 263–275.
- Gavrilescu, M.; Vizireanu, N. Predicting depression, anxiety, and stress levels from videos using the facial action coding system. Sensors 2019, 19, 3693.
- Scherer, S.; Stratou, G.; Morency, L.-P. Audiovisual behavior descriptors for depression assessment. In Proceedings of the 15th ACM on International Conference on Multimodal Interaction, Sydney, Australia, 9–13 December 2013; pp. 135–140.
- Morency, L.-P.; Stratou, G.; DeVault, D.; Hartholt, A.; Lhommet, M.; Lucas, G.; Morbini, F.; Georgila, K.; Scherer, S.; Gratch, J. SimSensei demonstration: A perceptive virtual human interviewer for healthcare applications. In Proceedings of the AAAI Conference on Artificial Intelligence, Austin, TX, USA, 25–30 January 2015.
- Gupta, R.; Malandrakis, N.; Xiao, B.; Guha, T.; Van Segbroeck, M.; Black, M.; Potamianos, A.; Narayanan, S. Multimodal prediction of affective dimensions and depression in human-computer interactions. In Proceedings of the 4th International Workshop on Audio/Visual Emotion Challenge, Orlando, FL, USA, 7 November 2014; pp. 33–40.
- Ringeval, F.; Schuller, B.; Valstar, M.; Cummins, N.; Cowie, R.; Tavabi, L.; Pantic, M. AVEC 2019 workshop and challenge: State-of-mind, detecting depression with AI, and cross-cultural affect recognition. In Proceedings of the 9th International on Audio/Visual Emotion Challenge and Workshop, Nice, France, 21 October 2019; pp. 3–12.
- Siegle, G.J.; Steinhauer, S.R.; Friedman, E.S.; Thompson, W.S.; Thase, M.E. Remission prognosis for cognitive therapy for recurrent depression using the pupil: Utility and neural correlates. Biol. Psychiatry 2011, 69, 726–733.
- Silk, J.S.; Dahl, R.E.; Ryan, N.D.; Forbes, E.E.; Axelson, D.A.; Birmaher, B.; Siegle, G.J. Pupillary reactivity to emotional information in child and adolescent depression: Links to clinical and ecological measures. Am. J. Psychiatry 2007, 164, 1873–1880.
- Price, R.B.; Rosen, D.; Siegle, G.J.; Ladouceur, C.D.; Tang, K.; Allen, K.B.; Ryan, N.D.; Dahl, R.E.; Forbes, E.E.; Silk, J.S. From anxious youth to depressed adolescents: Prospective prediction of 2-year depression symptoms via attentional bias measures. J. Abnorm. Psychol. 2016, 125, 267.
- Alghowinem, S.; Goecke, R.; Wagner, M.; Parker, G.; Breakspear, M. Eye movement analysis for depression detection. In Proceedings of the 2013 IEEE International Conference on Image Processing, Melbourne, Australia, 15–18 September 2013; pp. 4220–4224.
- Association, A.P. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013. J. Physiother. Res. Salvador 2019, 9, 155–158.
- World Health Organization. ICD-11 for Mortality and Morbidity Statistics. Version: 2019 April. Geneva. Available online: https://icd.who.int/browse11/l-m/en (accessed on 24 October 2022).
- Lochbaum, M.; Zanatta, T.; Kirschling, D.; May, E. The Profile of Moods States and athletic performance: A meta-analysis of published studies. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 50–70.
- Østergaard, S.D.; Jensen, S.; Bech, P. The heterogeneity of the depressive syndrome: When numbers get serious. Acta Psychiatr. Scand. 2011, 124, 495–496.
- Stein, D.J.; Phillips, K.A.; Bolton, D.; Fulford, K.; Sadler, J.Z.; Kendler, K.S. What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychol. Med. 2010, 40, 1759–1765.
- Oquendo, M.A.; Baca-García, E.; Mann, J.J.; Giner, J. Issues for DSM-V: Suicidal Behavior as a Separate Diagnosis on a Separate Axis; American Psychiatric Association: Washington, DC, USA, 2008; Volume 165, pp. 1383–1384.
- Lux, V.; Kendler, K. Deconstructing major depression: A validation study of the DSM-IV symptomatic criteria. Psychol. Med. 2010, 40, 1679–1690.
- Kamphuis, J.H.; Noordhof, A. On categorical diagnoses in DSM-V: Cutting dimensions at useful points? Psychol. Assess. 2009, 21, 294.
- Brown, T.A.; Di Nardo, P.A.; Lehman, C.L.; Campbell, L.A. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. J. Abnorm. Psychol. 2001, 110, 49.
- Nestler, E.J.; Barrot, M.; DiLeone, R.J.; Eisch, A.J.; Gold, S.J.; Monteggia, L.M. Neurobiology of depression. Neuron 2002, 34, 13–25.
- Kessler, R.C.; Bromet, E.J. The epidemiology of depression across cultures. Annu. Rev. Public Health 2013, 34, 119.
- Maj, M.; Stein, D.J.; Parker, G.; Zimmerman, M.; Fava, G.A.; De Hert, M.; Demyttenaere, K.; McIntyre, R.S.; Widiger, T.; Wittchen, H.U. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry 2020, 19, 269–293.
- Williams, L.S.; Brizendine, E.J.; Plue, L.; Bakas, T.; Tu, W.; Hendrie, H.; Kroenke, K. Performance of the PHQ-9 as a screening tool for depression after stroke. Stroke 2005, 36, 635–638.
- Hamilton, M. The Hamilton Rating Scale for Depression. In Assessment of Depression; Springer: Berlin/Heidelberg, Germany, 1986; pp. 143–152.
- Mundt, J.C.; Snyder, P.J.; Cannizzaro, M.S.; Chappie, K.; Geralts, D.S. Voice acoustic measures of depression severity and treatment response collected via interactive voice response (IVR) technology. J. Neurolinguist. 2007, 20, 50–64.
- Sharp, T.; Cowen, P.J. 5-HT and depression: Is the glass half-full? Curr. Opin. Pharmacol. 2011, 11, 45–51.
- Luscher, B.; Shen, Q.; Sahir, N. The GABAergic deficit hypothesis of major depressive disorder. Mol. Psychiatry 2011, 16, 383–406.
- Peterson, B.S.; Kaur, T.; Baez, M.A.; Whiteman, R.C.; Sawardekar, S.; Sanchez-Peña, J.; Hao, X.; Klahr, K.W.; Talati, A.; Wickramaratne, P. Morphological Biomarkers in the Amygdala and Hippocampus of Children and Adults at High Familial Risk for Depression. Diagnostics 2022, 12, 1218.
This entry is offline, you can click here to edit this entry!
