Electrocardiogram (ECG) still remains a very useful diagnostic method in modern cardiology. Its broad availability, noninvasiveness and good sensitivity explain why it plays a capital role in the very beginning of the process of diagnosis for every patient, with or without cardiac-related complaints. For the practitioner, good training in ECG interpretation is mandatory. Sometimes, the ECG trace reveals particular aspects that may cause confusion and complicate decision-making. Several less common situations underlying the general context and ECG features are presented. The syndromes studied have a high pathological significance and may range from acute emergencies that call for a rapid therapeutical response to chronic syndromes that require prolonged observation, monitoring and risk stratification.
1. Introduction
It was in 1903 when the bipolar three-channel electrocardiogram (ECG) was invented and recorded by William Einthoven. Since then, ECG has been a tool of remarkable clinical power, as it can quickly provide physicians with helpful and even critical information. As ECG communicates in its own unique way, it is of paramount importance for healthcare professionals to have the necessary competency to interpret it. Thanks to some investigators having an acute eye for detail, rare cardiological syndromes have been identified and characterized by their specific ECG patterns, which may testify to their clinical presentation. The instant identification of these patterns may lead to the immediate and proper management and treatment of those patients with favorable morbidity and mortality outcomes. This entry focuses on the detection of less common cardiological clinical syndromes, highlighting the general context and the ECG findings. A summary table of the syndromes’ diagnostic criteria and ECG patterns is provided below (Table 1), in order to offer a short overview of the main points and render the information more accessible to the reader.
Table 1. Electrocardiogram syndromes.
| ECG Syndrome |
ECG Diagnostic Criteria |
ECG Aspect |
| Wellen’s syndrome |
- –
-
Normal ECG in angina, T wave changes in V2-3 when pain-free.
- –
-
Absence of pathological Q waves.
- –
-
No R wave loss.
|
 |
| De Winter syndrome |
- –
-
No ST-segment elevation in precordial leads.
- –
-
Up-sloping ST-segment depression at J-point >1 mm.
- –
-
Deep symmetrical T waves in precordial leads.
- –
-
ST-segment elevation in aVR <0.5 mm.
- –
-
May be preceded or followed by ST-segment elevation.
|
 |
| Kounis syndrome |
- –
-
Evidence of myocardial ischemia on ECG in presence of systemic allergic reaction.
|
 |
| Takotsubo syndrome |
- –
-
New and reversible ECG changes (ST-segment elevation, ST-segment depression, left bundle branch block, T-wave inversion, and/or QTc prolongation) during the acute phase (3 months).
|
 |
| Yamaguchi syndrome |
- –
-
Giant negative T waves (>10 mm), left ventricular hypertrophy and possibly signs of complications, including atrial fibrillation and ACS with ST-segment elevation.
|
 |
| Wolff–Parkinson–White syndrome |
- –
-
Short PR interval <120 ms.
- –
-
Slurred upstroke at QRS beginning, called delta wave.
- –
-
Wide QRS complex >120 ms.
- –
-
T wave, ST-segment changes.
|
 |
| Lown–Ganong–Levine syndrome |
- –
-
Short PR interval <120 ms.
- –
-
Normal QRS complex <120 ms.
- –
-
Absence of delta wave.
|
 |
| Brugada syndrome |
- –
-
Type 1 consists of coved ST-segment elevations greater than 2 mm followed by an inverted T wave.
- –
-
Type 2 consists of a saddle-back ST-segment elevation greater than 2 mm followed by a normal or biphasic T wave.
- –
-
Type 3 is characterized by a coved or saddleback-shaped ST-segment elevation that is equal or less than 1 mm.
|
 |
| Frederick’s syndrome |
- –
-
Atrial fibrillation “f waves” or atrial flutter waves.
- –
-
Third degree AV block.
|
 |
PAFIYAMA
syndrome |
- –
-
Onset as paroxysmal atrial fibrillation.
- –
-
ST-segment elevation at J-point >0.1 mm in 2 leads.
- –
-
Inverted T waves in 2 leads.
- –
-
Left atrial enlargement signs.
- –
-
Left ventricular hypertrophy signs.
|
 |
| Haïssaguerre syndrome |
- –
-
J-point elevation >1 mm in >2 contiguous inferior and/or lateral leads in a patient with history of resuscitation from otherwise unexplained ventricular fibrillation or polymorphic ventricular tachycardia. Presence of J-point elevation >1 mm in >2 contiguous inferior and/or lateral leads on ECG.
|
 |
| Osborn syndrome |
- –
-
Haïssaguerre and Brugada syndrome criteria may be used.
|
 |
LEOPARD
syndrome |
- –
-
Left or biventricular hypertrophy.
- –
-
Repolarization abnormalities.
- –
-
Prolonged QT-interval.
- –
-
Atrioventricular blocks.
|
 |
2. Wellen’s Syndrome
Wellen’s syndrome was first described in 1982 by Hein J.J. Wellens (1935–2020) et al., in the Annadal Hospital, Maastricht, Netherlands, in a group of patients presenting with unstable angina. Findings later showed that 18% of the aforementioned group was proven to suffer from Wellen’s syndrome. After being solely treated medically, the majority of patients shortly developed a myocardial infarction
[1].
Usually, an atheromatic plaque ruptures, travels through the bloodstream to the heart as an embolus, and temporarily occludes the left anterior descending (LAD) artery, causing a pre-infarction state
[2]. This occlusion obstructs the myocardial perfusion, but soon after, the clot is lysed, and the occlusion is reversed before a myocardial infarction occurs
[3].
Clinical manifestations. Patients commonly present with chest pain, characteristic of unstable angina, or characteristic of stable exertional angina in rarer cases. Commonly, it is a substernal pain with tightness that radiates to the left arm, the jaw, or the back. Heavy meals, cold, or exertion can exacerbate the pain
[4]. The pain can also be associated with dyspnea, sweating, dizziness, and palpitations. The symptoms mainly occur in the early morning and last for about 15–25 min
[5]. One atypical clinical presentation of Wellen’s syndrome was reported by Ajibawo T. et al., where a patient presented with an episode of syncope, intense abdominal pain, and vomiting and denied any of the common symptoms
[6].
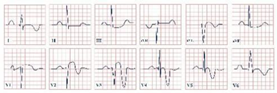
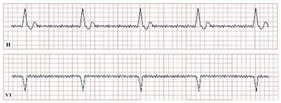
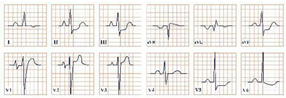
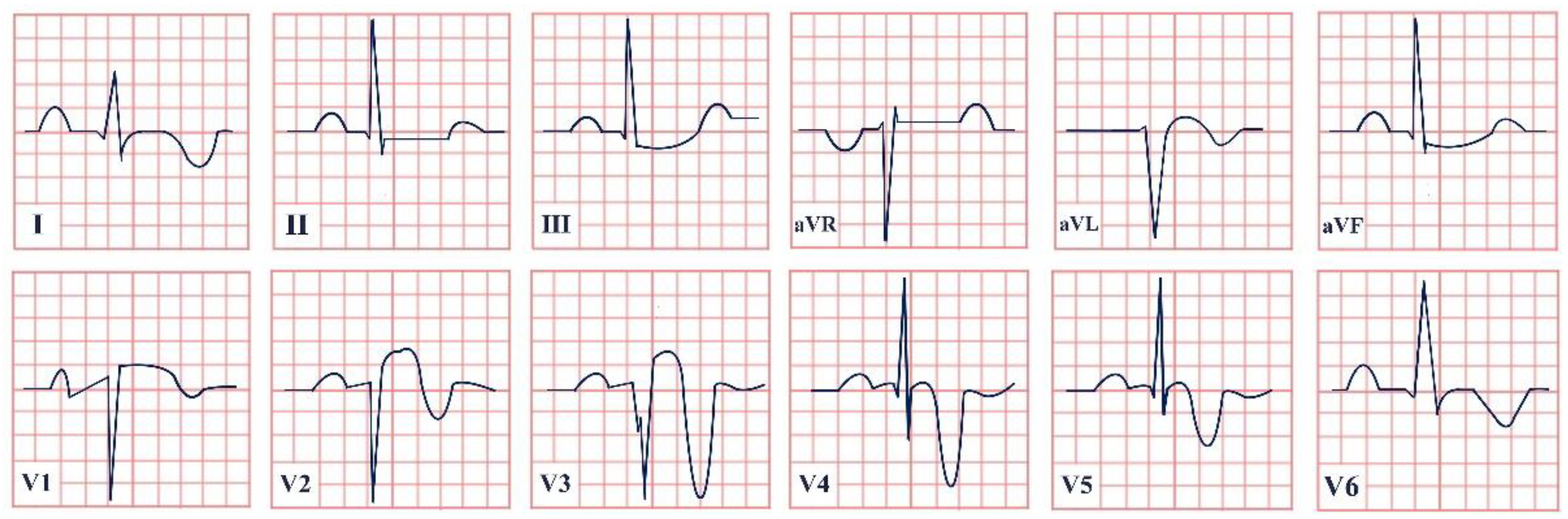
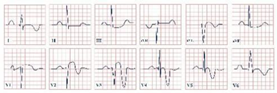
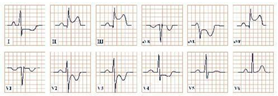
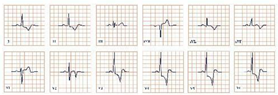
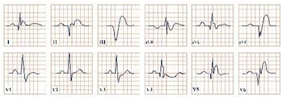
Paraclinical diagnosis. ECG will show a sinus rhythm and an otherwise normal ECG aspect but with T wave changes. The T wave in V2–V3 leads can be deeply inverted and symmetrical (Type A Wellen’s) or biphasic (Type B Wellen’s), as they often begin as biphasic and slowly evolve into deeply inverted ones (
Figure 1). ECG can appear totally normal during the period of chest pain and only show changes when the patient is pain-free, which is why obtaining a series of ECGs is crucial to establishing the diagnosis
[7].
Figure 1. Electrocardiogram aspect in Wellen’s syndrome.
The cardiac enzymes can be normal or slightly increased. Coronarography is positive for LAD artery occlusion in almost all cases, with few exceptions, showing a critical total or near-total obstruction. Cardiac stress testing is strictly contraindicated, as it can trigger an acute myocardial infarction
[8].
Diagnostic criteria. Wellen’s diagnostic criteria are as follows:
-
Previous history of angina.
-
Normal or slightly increased cardiac enzymes.
-
Normal ECG during angina and T wave abnormalities when pain-free in V2–V3 (deeply inverted in Type A or biphasic in Type B).
-
No pathological Q waves.
-
Differential diagnosis. The following ECG changes can mimic the specific Wellen’s syndrome aspects.
- –
-
T wave inversion or biphasic T wave due to ischemia.
- –
-
T wave inversion, in most leads, due to Takotsubo cardiomyopathy.
- –
-
ST-segment depression and T wave flattening, best seen in V2–V4, due to hypokalemia.
- –
-
T wave inversion in V1–V6 due to acute pulmonary embolism.
- –
-
T wave inversion due to cardiac memory, such as in LBBB, pacemakers, or transient tachycardia.
- –
-
T wave inversion in V1–V3 physiologically in prepubertal patients.
- –
-
T wave inversion in most leads due to pericarditis, myocarditis, or advanced AV block
[10].
Treatment/Prognosis. Prognosis can be poor if Wellen’s syndrome goes unrecognized and is treated with pharmacotherapy alone. Due to its similarities with acute coronary syndrome (ACS) without persistent ST-segment elevation, it can be frequently misdiagnosed and, thus, lead to fatal complications
[3]. Prognosis is good in patients who undergo coronary revascularization with either percutaneous coronary intervention (PCI) to open the vessel and improve blood flow or coronary artery bypass grafting (CABG), using a vessel graft to bypass the occlusion. Patient follow-ups, identification, and elimination of atherogenic risk factors are highly suggested as there is a risk of recurrence
[11].
3. Conclusions
The electrocardiogram is a widely available, affordable, and non-invasive modality with a high diagnostic sensitivity. As modern cardiology evolves, so do the types of ECG and the settings where it is available, with portable 24 h Holter monitors, treadmill testing, and emergency electrocardiograms in the field. With cardiovascular disease being the leading cause of death worldwide, it is vital that healthcare professionals from all specialties have a thorough training on electrocardiogram interpretation, being able to identify not only common ECG findings but also rarer and more complicated ones. In this entry, researchers provide information regarding the discovery of various ECG syndromes, their clinical manifestations and paraclinical investigations to be used, as well as the prognosis and treatment.
The diagnosis of the above-mentioned syndromes can be challenging for the physician, resulting in misdiagnosis and delay in treatment. The knowledge and understanding of these syndromes are critical for detecting early, treating appropriately, and preventing fatal arrhythmias and sudden cardiac death. Through this entry, researchers hope to spread awareness of all these syndromes and their particularities in order to promote prompt recognition, referral, and improved survival rates.
This entry is adapted from the peer-reviewed paper 10.3390/jpm12111754