Skin disease remains a common complaint among deployed service members. To mitigate the limited supply of dermatologists in the U.S. Military Health System, teledermatology has been harnessed as a specialist extender platform, allowing for online consultations in remote deployed settings. Operational teledermatology has played a critical role in reductions of medical evacuations with significant cost-savings. When direct in-person lesion visualization is unattainable, teledermoscopy can be harnessed as an effective diagnostic tool to distinguish suspicious skin lesions. Teledermoscopy has the versatile capacity for streamlined incorporation into the existing asynchronous telemedicine platforms utilized worldwide among deployed U.S. military healthcare providers. In terms of clinical utility, teledermoscopy offers a unique and timely opportunity to improve diagnostic accuracy, early detection rates, and prognostic courses for dermatological conditions. Such improvements will further reduce medical evacuations and time away from mission, thereby improving mission readiness and combat effectiveness. As mission goals are safeguarded, associated operational budget costs are also preserved. This innovative, cost-effective technology merits integration into the U.S. Military Health System (MHS).
- teledermoscopy
- teledermatology
- military medicine
- operational dermatology
- occupational skin disease
- operational readiness
- combat effectiveness
- medical evacuation
- mission preparedness, medical readiness
- monkeypox pandemic
- COVID-19 pandemic
1. Introduction
Telemedicine harnesses technology-based software to deliver convenient and cost-effective medical care at a distance. Telemedicine was introduced as a healthcare delivery model in the 1960s and has become a permanent delivery system [1]. For the last three decades, the United States Department of Defense (DoD) has recognized telemedicine as a component of the U.S. Military Health System (MHS) [2]. Military telemedicine aims to improve access to specialized health care services in areas where military treatment facilities are limited or unavailable [2][3]. Common modalities for military telehealth services include store-and-forward (asynchronous) systems, real-time (synchronous), and remote monitoring. Military dermatology frequently utilizes an asynchronous telemedicine model. Asynchronous delivery is a practical option for operational settings with a wide range of global time zones. Likewise, asynchronous delivery can be helpful to military dermatologists as photographs of cutaneous lesions can be further analyzed with computer software [3].
Moreover, with recent advancements in technology and the internet, a dermatoscope can be utilized for remote synchronous visualization of skin lesions. This technology is referred to as teledermoscopy. Teledermoscopy is a noninvasive diagnostic method that utilizes special instrumentation to assess cutaneous lesions when direct, clear visualization is challenging. This practical technology is an invaluable option in the prevention, diagnosis, and treatment of dermatological conditions [4][5].
Teledermoscopy is a relatively new diagnostic tool that has not been widely adopted by dermatologists. Although teledermoscopy is a low-cost technology with high diagnostic accuracy, there is scant research on its value in dermatological practice [6][7]. Such limited literature underscores the need for further studies on teledermoscopy utilization, particularly in military healthcare settings [7].
This encyclopedia article provides an updated briefing on teledermoscopy research over the last two decades and reviews evidence for the integration of teledermoscopy in military medicine. Additionally, it highlights teledermoscopy benefits such as delivery options, diagnostic efficacy, training opportunities, calculable financial benefits, clinical value in operational medicine, affordability of potential implementation, and overall relevance to mission-preparedness in a dynamic pandemic era.
2. Technological Evolution of Teledermoscopy
Several technological modalities enable teledermoscopy delivery, such as the combined utilization of a video camera (webcam or a smartphone) and a dermatoscope or magnifying glass. Other modalities include an “all-in-one” system dermatoscope with a built-in digital camera and a wireless digital microscope that can be connected to mobile phones and personal computers [6] (Figure 1). There is a vast array of evidence that demonstrates the significant benefits of teledermatology in the military. Table 1 organizes evidence associated with teledermatology usage in military health systems.
Figure 1. Teledermoscopy delivery. Overview of device options for teledermoscopy delivery.
The implementation of teledermoscopy can significantly improve early skin cancer detection than teledermatology alone [8]. Teledermoscopy can be harnessed as a practical diagnostic device to triage patients with skin conditions. With the advancement of technological delivery systems, primary care physicians and patients can conduct successful teledermoscopy sessions. Such advancements include smartphone-based microscopes, handheld digital microscopes, dermatoscopes with built-in camera systems, universal attachable dermatoscope lenses, and manual webcam attachments [8]. These devices are travel-friendly, inexpensive, and can be efficiently utilized by general practitioners to transfer photos of suspected lesions [8][9]. This practical process can aid in the elimination of unnecessary in-person consultation (and associated costs).
Additionally, a webcam in combination with a dermatoscope (or magnifying glass) can be utilized to visualize skin lesions during teledermatological consultations. Webcam devices can be readily employed to practice teledermoscopy. The incorporation of teledermoscopy has further expanded the utility of teledermatology in diagnosing these skin lesions.
3. Teledermoscopy Data Underscores Potential Benefits for U.S. Military Health System
3.1 Faster Access to Dermatological Care
Since its inception in the military three decades ago, teledermatology has enabled more efficient consultations and assessments. Through telemedicine platforms, service members can see a specialist within an average waiting time of 12–24 hours, in comparison to 4-8 weeks for in-person appointments [3]. Moreover, the DoD utilization of teledermatology has produced significant operational cost-savings. Military teledermatology has prevented unnecessary medical evacuations, facilitated urgent consults, and reduced physicians’ cost of travel [3].
3.2 Operational Cost-Savings
It is estimated that the healthcare costs associated with dermatology visits can be reduced by $35 million annually if approximately 5% of the office-based visits are shifted to teledermatology [10]. A 2010 study evaluated a total of 2,197 store-and-forward teledermatology consults generated by military health providers between the specified time frame: January 2005 through January 2009. This study found that teledermatology appropriately triaged dermatological cases and prevented unnecessary evacuation from the mission. The estimated total cost-saving from unnecessary evacuation during the period of the study was 30.4 million dollars [11]. Teledermatology utilization also provides incalculable savings by avoidance of dangerous travel in a war zone [11]. These results underscore the magnitude of cost-savings associated with preventing medical evacuations in combat [11]. Additional mission benefits that cannot be fully quantified include cost-savings associated with enriched quality of life-related to earlier care access and disease management [12][13][14].
3.3 Diagnostic Strength
Moreover, when compared to in-person evaluations, teledermatology offers matched diagnostic accuracy in skin disease [15]. The IMAGE IT Trial analyzed approximately five hundred skin lesions of concern independently assessed through teledermoscopy and in-person consultations [16][17][18]. Out of 491 lesions of concern, only twelve malignant lesions were misreported as benign. However, when histopathology was utilized, only one malignant lesion was missed (one basal cell carcinoma misdiagnosed as a solar keratosis lesion) [17]. The IMAGE IT Trial determined teledermoscopy evaluation accuracy approximated 100% sensitivity and 90% specificity. The most common skin conditions requiring teledermatology consultation include acne, atopic dermatitis, hair loss, and skin cancer [19]. Teledermoscopy application improves the remote assessment of pigmented lesions and synergistically determines the potential need for prompt biopsy [16][18].
4. Cost-Effective Integration for U.S. Military Health System
Day et al. conducted the first military study (Navy Medical Corps) to evaluate teledermoscopy within a military health system worldwide. The study sought to compare the diagnostic accuracy of a teledermatology consultation using synchronous teledermoscopy and a traditional in-person dermatological consultation [7]. The study was conducted on two patients at a remote military medical clinic, and each provider was blinded to the lesion diagnosis. Each patient presented with two lesions (benign and malignant) that were examined by two board-certified dermatologists [7].
The teledermoscopy session utilized a repurposed webcam ubiquitous at most military training facilities (MTFs) and a dermatoscope (x10 magnification) with transillumination properties. Figure 2 depicts the primary protocol used for the synchronous teledermoscopy application. This military research study revealed both the in-person dermatologist and the remote dermatologist were in 100% concordance regarding the accurate diagnosis of each lesion as benign or malignant when using teledermoscopy [7].

Figure 2. Synchronous teledermoscopy protocol tested at a military training facility. Basic configuration for teledermoscopy. (A) Dermatoscope; (B) Cisco Jabber Webcam; (C) Sanitize dermatoscope and skin lesions with alcohol; (D) Gentle contact between webcam and dermatoscope.
Likewise, all military dermatologists possess a dermatoscope and use dermoscopy in their daily practice [7]. The ubiquitous presence of webcam technology and personal dermatoscopes bypasses the need for high financial investments for initial military implementation [7]. The widespread existence of webcam technology at MTFs offers a unique learning opportunity for graduate medical education. Basic practice with a combined dermatoscope and webcam application has the potential to boost dermoscopy skills in military residency training programs.
Lastly, manual webcam attachment uniquely supports synchronous and asynchronous teledermoscopy delivery. An additional advantage, the manual attachment to webcams is not dependent on smartphone technologies. Furthermore, unlike smartphones, webcams can operate on minimal bandwidth (equivalent to one bar of data service). Such minimal bandwidth requirements support asynchronous delivery on the Defense Health Agency (DHA) Global Teleconsultational Portal (GTP) [7]. These simple yet effective features of webcam attachment delivery champion this modality as an affordable and pragmatic option for more widespread utilization of operational teledermoscopy in the United Military Health System [7]. Table 2 illustrates the distinct benefits and limitations of each teledermoscopic modality.
Table 2. Teledermoscopy technologies. Summary of distinct benefits and limitations.
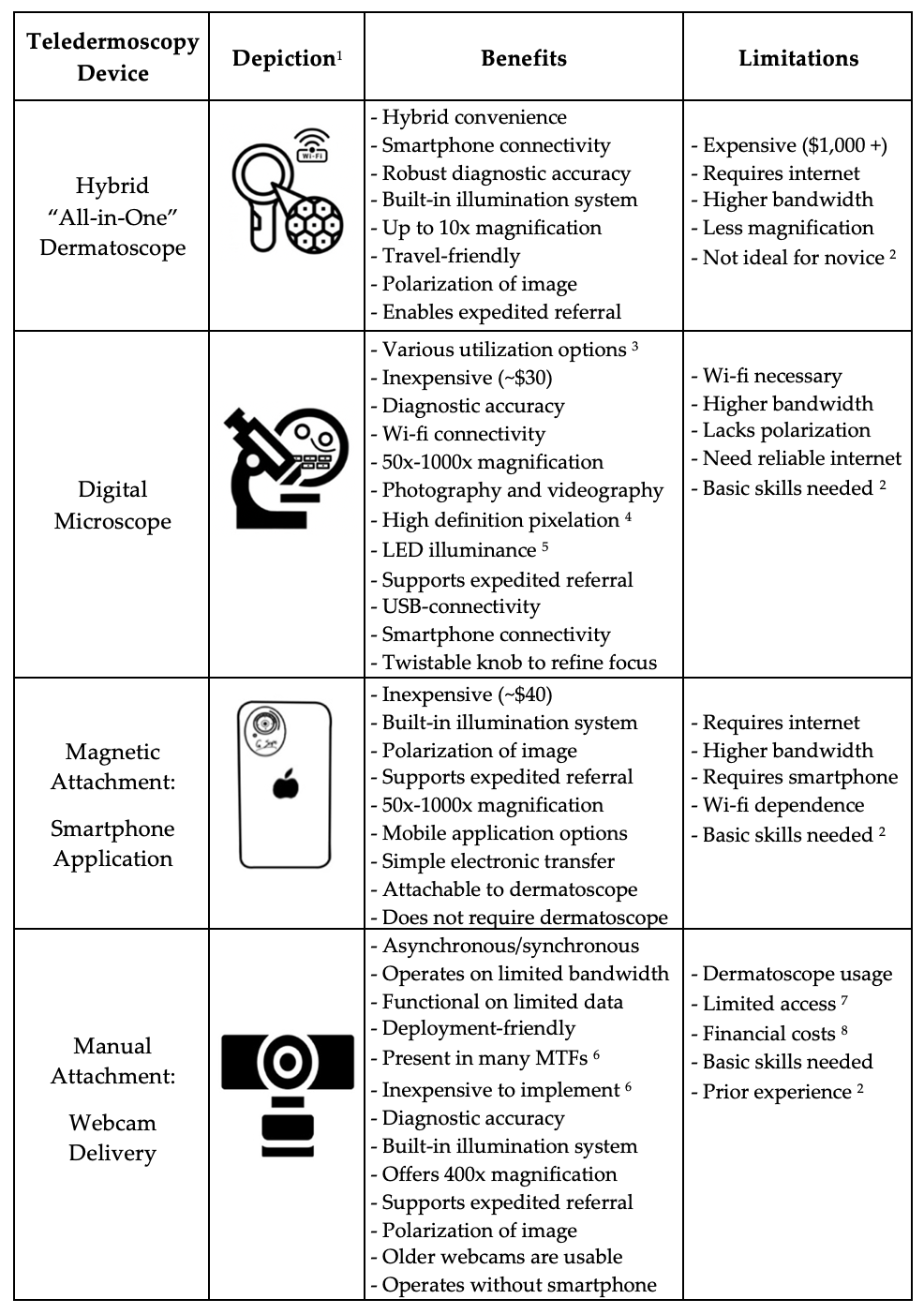
1 Device depictions are for illustrative purposes only.
2 Prior dermoscopy experience or basic training in dermoscopy is recommended for proper usage.
3 Delivery options include microscope base or free mobile application with hand.
4 High pixelation includes 2 million pixels: high definition 1080P HD picture quality.
5 Light-emitting diodes (LED) contain properties of energy efficiency.
6 Basic webcam technology exists in many military training facilities – cost-effective implementation.
7 In operational settings, dermatoscopes may not be readily available.
8 Dermatoscopes are currently not included in the reimbursable medical allowance for deployment.
Table 1. Evidence of Teledermatology Benefits.
|
Benefits |
Research Evidence |
|
Healthcare Cost Reduction
|
- Minimize unnecessary medical evacuation [18] - Reduces dermatology referrals [19] |
|
Timely Treatments
|
- Triage of more urgent, complicated medical problems [18] - Faster diagnostic procedures, medical treatment, and surgery [12]
|
|
Medical Care Mobilization |
- U.S. VHA1 implementation increased access to care2 [20] - Face-to-face dermatological care is maintained virtually [21]
|
|
Early Lesion Detection
|
- Promotes timely treatment [18] - Improved prognosis [12] - Helpful triage for general practitioners [12][18]
|
|
Reduced Evacuations |
- Reduced time away from missions - Reduced appointment time to visit - Improved recovery time - Improved prognosis - Reduced medical discharge [18]
|
1 United States Veterans Health Administration.
2 From 2002-2014, the VA provided 234,928 teledermatology consultations (6% of all consultations) to veterans without local access to dermatologists.
5. Strategies for Successful Military Implementation
Teledermoscopy offers clinical utility in military medicine, with promising potential to support the medical readiness of the force. Despite feasible telehealth platforms for military implementation, operational settings present unique obstacles in telehealth delivery, including limited bandwidth, ongoing staff permanent change of station (PCS) assignments, staff inexperience with dermoscopy, and limitations in authorized reimbursable medical allowance to military providers. Dermatoscopes are not currently authorized as reimbursable equipment in the designated medical allowance for deployed medical providers.
5.1 Technological Options for Limited Bandwidth Connectivity
Existing technologies can mitigate obstacles in limited bandwidth connectivity. In terms of technological implementation, teledermoscopy fits appropriately into the Defense Health Agency (DHA) Global Teleconsultational Portal (GTP) [22][23][24]. Enacted in 2021, GTP is an asynchronous virtual medical center (VMC) currently utilized in the United States Military Health System (MSH). GTP was derived from the merger of the Pacific Asynchronous TeleHealth and the Health Experts Online Portal (PATH/HELP) systems which previously enabled provider-to-provider teleconsultation and patient support to the MHS. Since 2004, GTP has operated as a worldwide accessible, HIPAA-compliant, secure, web-based system for military health care personnel and providers. GTP has been widely used to access medical specialists, such as board-certified military dermatologists [24].
Interestingly, GTP can operate on a web browser with limited internet bandwidth, affording the unique opportunity to be utilized at military treatment levels [24]. Limited bandwidth due to poor data service can limit the transmissibility of medical data. As such, these technological adaptations allow for continued streaming at limited bandwidths via the Defense Health Agency Global Teleconsultational Portal, which operates on low bandwidth connectivity – equivalent to “one bar of service” in cellular usage [24].
5.2 Training Methods for Improving Teledermoscopic Diagnosis
A comparative study assessed teledermoscopy versus clinical examination in the accurate identification of skin cancers. Results revealed high diagnostic accuracy of skin cancers via teledermoscopy. Additionally, this investigation demonstrated consistent diagnostic accuracy among general practitioners and surgeons [25]. Various factors attributed to proper diagnostic consensus including a six-hour training course, photography quality, systematic methodology, ABCDE clinical algorithm implementation, and data acquisition software [25].
The research study implemented a training course focused on two major domains: clinical diagnosis of skin cancer (per the ABCDE clinical algorithm) and proper acquisition of teledermoscopic images. The ABCDE algorithm taught providers important clinical factors in the assessment of suspicious lesions. A skin lesion was deemed suspicious if a minimum two of the following three criteria were graded positive: A – asymmetry; C – color; E – evolution. Training for proper acquisition of teledermoscopic images included hands-on training to utilize a teledermoscopic system: digital dermatoscope and specialized teledermoscopy data acquisition software. Providers were also taught to collect relevant clinical data points (patient identification, Fitzpatrick skin phototype, skin cancer risk factors, anatomical region of concern, relevant ABCDE criteria) to produce a teledermoscopic report. Figure 3 illustrates quality dermoscopic images obtained in the study [25]. These successful findings in diagnostic accuracy are suggestive to the spectrum of options to deliver focused teledermoscopy training for general providers. Selective teledermoscopy education could yield great benefits for military healthcare providers, especially those in critical settings where dermatologists are in limited supply.

Figure 3. Dermoscopic images: (A) Dysplastic Naevus; (B) Melanoma in Situ; (C) Basal Cell Carcinoma (low grade-nodular type).
5.3 Teledermoscopy Education for New Providers
The transient nature of military staff assignments leads to more frequent staff turnover. This recurrent turnover may lead to new medical support staff with little to no experience in teledermoscopy. Such inexperience may impede successful teledermoscopy delivery. Nonetheless, these barriers can be overcome by concise training to ensure basic competency. For example, a pragmatic option for teledermoscopy training could involve a demonstration video that teaches proper utilization for best diagnostic outcomes. Figure 4 features key points for ideal acquisition of dermoscopic images.
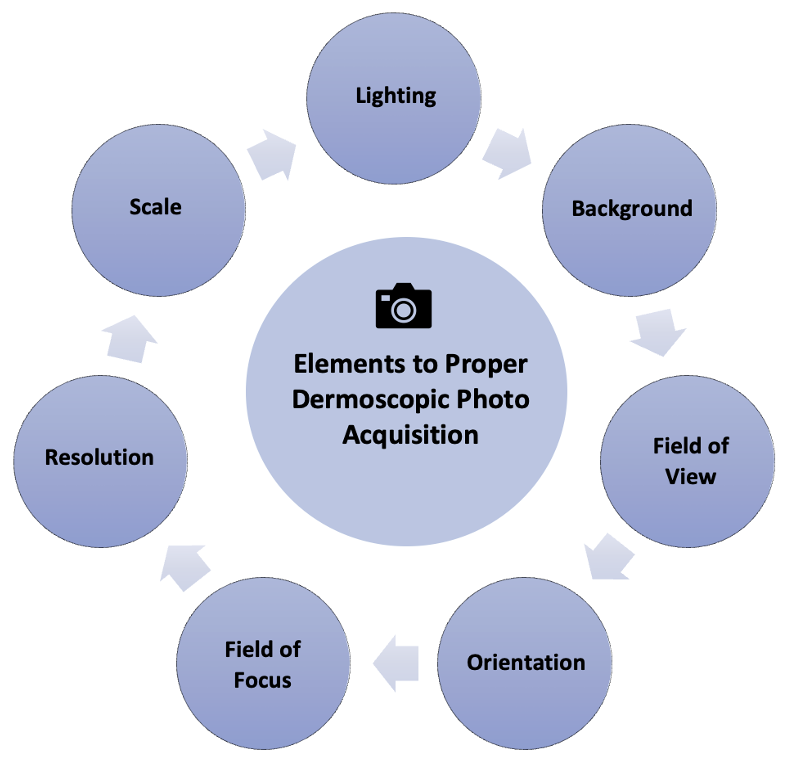
Figure 4. Key elements for the successful acquisition of clinical images for asynchronous teledermatology consultations. Important delivery considerations include appropriate lighting, background, field of view, orientation, focus, field, resolution, and photo scale.
Figure 5 outlines best practices to capture teledermoscopic images for asynchronous delivery, commonly used in operational dermatology. Figure 6 provides a checklist of recommendations to ensure high-quality teledermoscopic images via an asynchronous store-and-forward telemedicine consultation. Important delivery considerations include appropriate lighting, background, the field of view, orientation, focus, field, resolution, and photo scale. The implementation of dermoscopy algorithms can increase the sensitivity, specificity, and early detection of critical lesions, including skin cancers, compared to examination by the naked eye [26]. Likewise, dermoscopy can lead to the detection of thinner and smaller cancers. Such a diagnostic sensitivity is critical to mission effectiveness and decreased evacuations. With basic instruction, operational teledermoscopy could be successfully incorporated into the existing “store-and-forward” asynchronous military telemedicine platform.
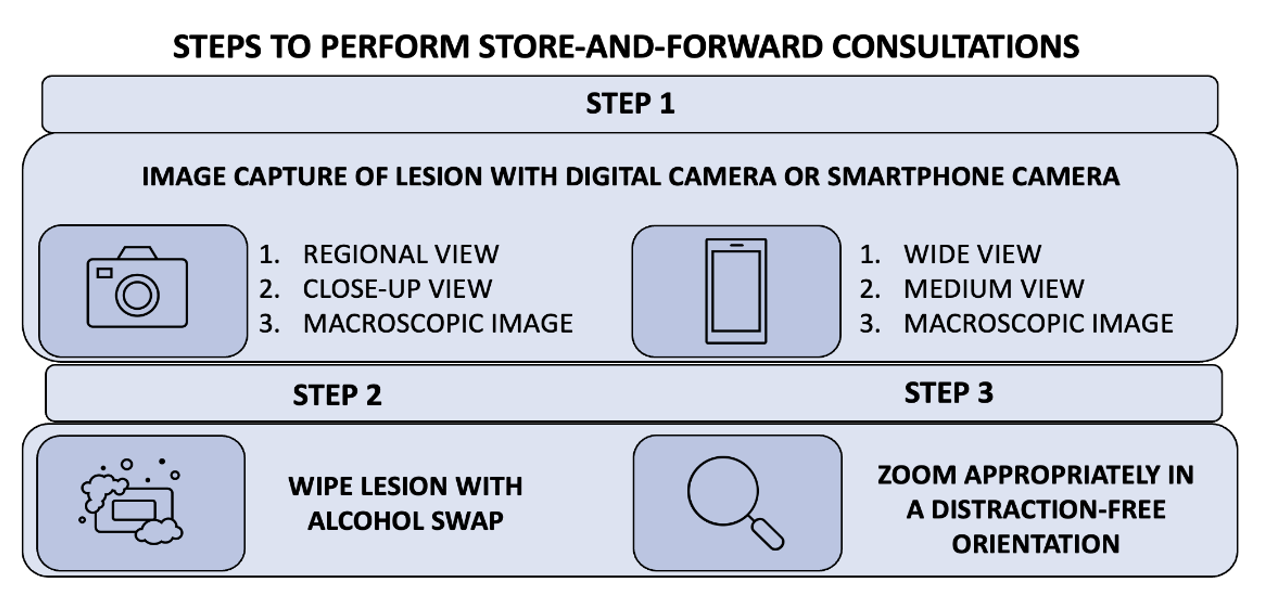
Figure 5. Teledermoscopy using an asynchronous delivery system. The summary of three key steps describes how to perform teledermoscopy via an asynchronous store-and-forward telemedicine consultation successfully. Asynchronous teledermatology is widely utilized in operational dermatology.
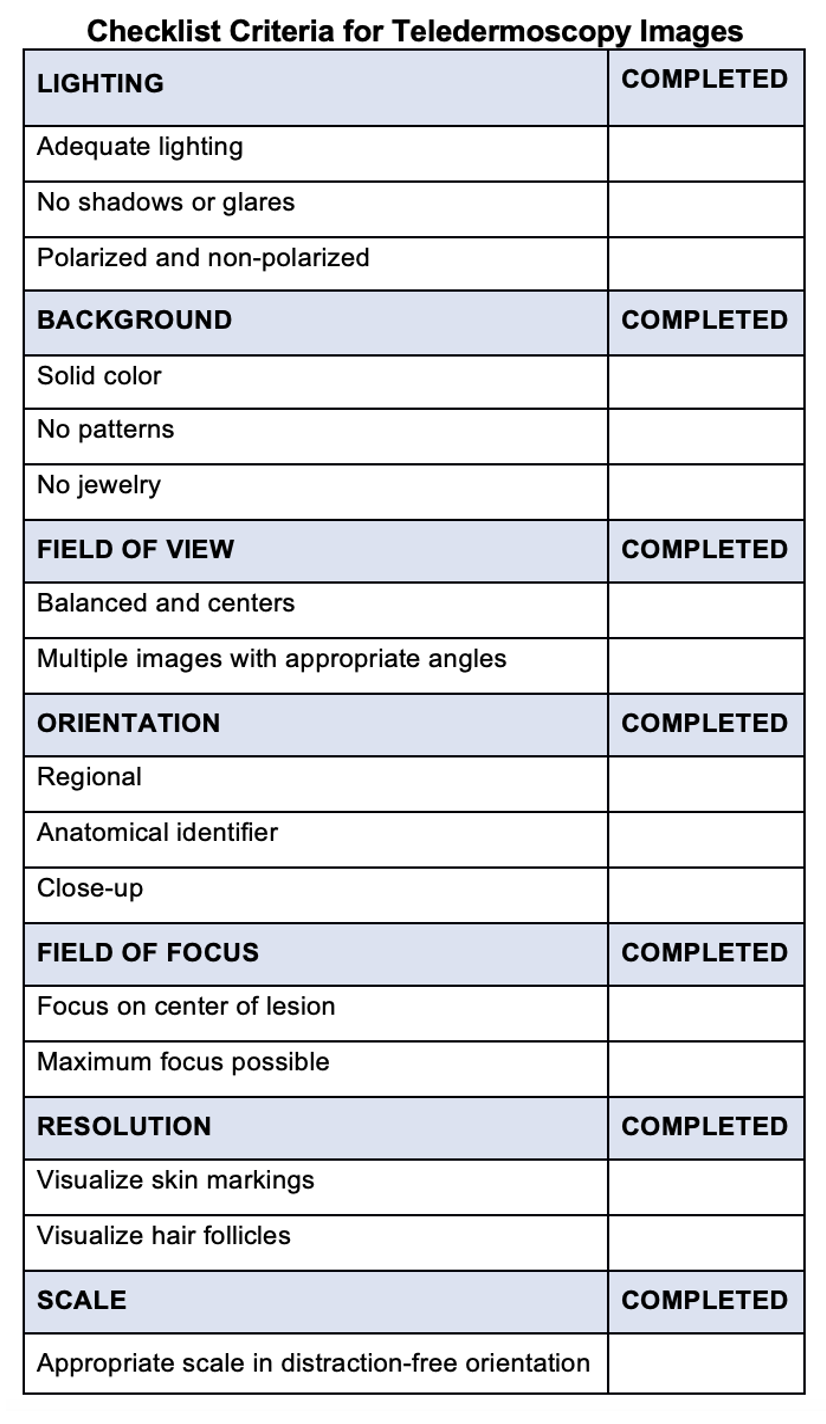
Figure 6. Checklist criteria for teledermoscopy images. The checklist provides recommendations to ensure high-quality teledermoscopic images via an asynchronous store-and-forward telemedicine consultation. Important delivery considerations include appropriate lighting, background, field of view, orientation, field of focus, resolution, and orientation.
5.4 Dermatoscope Inclusion on Authorized Medical Allowance List
A valuable for successful military integration of teledermoscopy includes the necessary inclusion of a dermatoscope in the designated Authorized Medical Allowance List (AMAL) for deployed personnel. A traditional dermatoscope can be harnessed into a valuable tool for teledermoscopy. Usage of a traditional dermatoscope can be readily implemented into the existing “store and forward” asynchronous military telemedicine healthcare delivery system for deployed personnel.
Military personnel often engage in operational requirements that increase their ultraviolet light exposure [27]. Likewise, sunscreen protection and sun-protective clothing are underutilized among military personnel, particularly in a deployed setting [28]. Furthermore, military (current and prior service) demographics include two groups who are predisposed to high rates of skin cancer: Caucasians (Fitzpatrick phototype II) and men over the age of 50 [29]. With the compounded risks of skin cancer among military personnel, it is prudent to include dermatoscopes as part of the designated medical allowance for deployed military providers. Dermatoscopes empower providers to detect lesions earlier in the disease course, significantly improving lesion prognosis and associated disease mortality reduction. With webcam technology readily available at most military training facilities (MTFs), teledermoscopy merits inclusion in the utilization of military telemedicine [7].
6. Conclusion
In military operational settings, dermatologists provide most dermatologic care yet remain in limited supply. Due to the high demand and limited availability of dermatologists, teledermatology is an exceptional specialist extender that allows medical providers worldwide access to dermatology consultations. Teledermatology plays a critical role in reduced medical evacuations and associated cost-savings. As a valuable diagnostic feature of teledermatology, teledermoscopy integration into the military healthcare system is merited. With versatile diagnostic capacity, teledermoscopy can provide synchronous real-time remote visualization of skin lesions, facilitating faster diagnosis, timely treatments, and reduced medical evacuations. Likewise, teledermoscopy can be readily integrated into a “store-and-forward” asynchronous teledermatology platform, as commonly utilized in the United States Military Health System (MHS).
As society continues to evolve in a pandemic era with bioterrorism threats, the United States Military Health System must also adapt to meet the critical need for swift diagnosis and prompt treatment. Currently, no teledermoscopy practice guidelines exist, presenting a unique leadership opportunity to establish clinical standards. Such initiatives could set a meaningful precedent for the nation to follow suit and improve prognosis of potentially fatal dermatological conditions. Improved clinical outcomes ultimately reduce medical evacuations, thereby improving medical readiness and combat effectiveness. As mission goals are safeguarded, associated operational budget costs are also preserved.
References
- Board on Health Care Services. The Evolution of Telehealth: Where Have We Been and Where Are We Going? National Academies Press: Cambridge, MA, USA, 2012.
- Poropatich, R.; Lappan, C.; Gilbert, G. Telehealth in the Department of Defense. In Understanding Telehealth; Rheuban, K.S., Krupinski, E.A., Eds.; McGraw-Hill Education: New York, NY, USA, 2022.
- Teledermatology in the US Military: A Historic Foundation for Current and Future Applications. Available online: https://www.mdedge.com/dermatology/article/164865/practicemanagement/teledermatology-us-military-historic-foundation (accessed on 17 August 2022).
- Sonthalia, S.; Yumeen, S.; Kaliyadan, F. Dermoscopy Overview and Extradiagnostic Applications; StatPearls Publishing: Tampa, FL, USA, 2022.
- Argenziano, G.; Soyer, H.P. Dermoscopy of Pigmented Skin Lesions—A Valuable Tool for Early Diagnosis of Melanoma. Lancet Oncol. 2001, 2, 443–449. https://doi.org/10.1016/s1470-2045(00)00422-8.
- Uppal, S.K.; Beer, J.; Hadeler, E.; Gitlow, H.; Nouri, K. The Clinical Utility of Teledermoscopy in the Era of Telemedicine. Ther. 2021, 34, e14766. https://doi.org/10.1111/dth.14766.
- Day, W.G.; Shrivastava, V.; Roman, J.W. Synchronous Teledermoscopy in Military Treatment Facilities. Med. 2020, 185, e1334–e1337. https://doi.org/10.1093/milmed/usz479.
- Veronese, F.; Branciforti, F.; Zavattaro, E.; Tarantino, V.; Romano, V.; Meiburger, K.M.; Salvi, M.; Seoni, S.; Savoia, P. The Role in Teledermoscopy of an Inexpensive and Easy-to-Use Smartphone Device for the Classification of Three Types of Skin Lesions Using Convolutional Neural Networks. Diagnostics 2021, 11, 451. https://doi.org/10.3390/diagnostics11030451.
- Coates, S.J.; Kvedar, J.; Granstein, R.D. Teledermatology: From Historical Perspective to Emerging Techniques of the Modern Era: Part II: Emerging Technologies in Teledermatology, Limitations and Future Directions. Am. Acad. Dermatol. 2015, 72, 577–586; quiz 587–588. https://doi.org/10.1016/j.jaad.2014.08.014.
- Wang, R.H.; Barbieri, J.S.; Nguyen, H.P.; Stavert, R.; Forman, H.P.; Bolognia, J.L.; Kovarik, C.L. Clinical Effectiveness and Cost-Effectiveness of Teledermatology: Where Are We Now and What Are the Barriers to Adoption? Am. Acad. Dermatol. 2020, 83, 299–307. https://doi.org/10.1016/j.jaad.2020.01.065.
- Teledermatology from a Combat Zone | Dermatology | JAMA Dermatology | JAMA Network. Available online: https://jamanetwork.com/journals/jamadermatology/fullarticle/209971 (accessed on 17 August 2022).
- Snoswell, C.L.; Caffery, L.J.; Whitty, J.A.; Soyer, H.P.; Gordon, L.G. Cost-Effectiveness of Skin Cancer Referral and Consultation Using Teledermoscopy in Australia. JAMA Dermatol. 2018, 154, 694–700. https://doi.org/10.1001/jamadermatol.2018.0855.
- Wootton, R.; Bloomer, S.E.; Corbett, R.; Eedy, D.J.; Hicks, N.; Lotery, H.E.; Mathews, C.; Paisley, J.; Steele, K.; Loane, M.A. Multicentre Randomised Control Trial Comparing Real Time Teledermatology with Conventional Outpatient Dermatological Care: Societal Cost-Benefit Analysis. BMJ 2000, 320, 1252–1256. https://doi.org/10.1136/bmj.320.7244.1252.
- Naka, F.; Lu, J.; Porto, A.; Villagra, J.; Wu, Z.H.; Anderson, D. Impact of Dermatology EConsults on Access to Care and Skin Cancer Screening in Underserved Populations: A Model for Teledermatology Services in Community Health Centers. Am. Acad. Dermatol. 2018, 78, 293–302. https://doi.org/10.1016/j.jaad.2017.09.017.
- Beer, J.; Hadeler, E.; Calume, A.; Gitlow, H.; Nouri, K. Teledermatology: Current Indications and Considerations for Future Use. Dermatol. Res. 2021, 313, 11–15. https://doi.org/10.1007/s00403-020-02145-3.
- Lee, K.J.; Finnane, A.; Soyer, H.P. Recent Trends in Teledermatology and Teledermoscopy. Pract. Concept. 2018, 8, 214–223. https://doi.org/10.5826/dpc.0803a13.
- Tan, E.; Yung, A.; Jameson, M.; Oakley, A.; Rademaker, M. Successful Triage of Patients Referred to a Skin Lesion Clinic Using Teledermoscopy (IMAGE IT Trial). J. Dermatol. 2010, 162, 803–811. https://doi.org/10.1111/j.1365-2133.2010.09673.x.
- Altayeb, A.; Dawood, S.; Atwan, A.; Mills, C. Teledermoscopy: A Helpful Detection Tool for Amelanotic and Hypomelanotic Melanoma. J. Dermatol. 2021, 185, 1244–1245. https://doi.org/10.1111/bjd.20609.
- Pendlebury, G.A.; Oro, P.; Haynes, W.; Merideth, D.; Bartling, S.; Bongiorno, M.A. The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review. Dermatopathology 2022, 9, 212–243. https://doi.org/10.3390/dermatopathology9030027.
- Landow, S.M.; Oh, D.H.; Weinstock, M.A. Teledermatology Within the Veterans Health Administration, 2002–2014. e-Health 2015, 21, 769–773. https://doi.org/10.1089/tmj.2014.0225.
- Raugi, G.J.; Nelson, W.; Miethke, M.; Boyd, M.; Markham, C.; Dougall, B.; Bratten, D.; Comer, T. Teledermatology Implementation in a VHA Secondary Treatment Facility Improves Access to Face-to-Face Care. e-Health 2016, 22, 12–17. https://doi.org/10.1089/tmj.2015.0036.
- GTP (v5.0)—Login. Available online: https://help.nmcp.med.navy.mil/path/user/ViewLogin.action (accessed on 17 August 2022).
- Defense Health Agency. PATH & HELP to Transition to GTP; Department of Defense: Washington, DC, USA, 2020. Available online: https://path.tamc.amedd.army.mil/path/pdf/GTP_Transition2.pdf (accessed on 4 August 2022).
- Reynolds, N. “Defense Health Agency (DHA) Update on Virtual Health (VH) for Defense Health Board” Presentation, Virtual. 30 March 2022. Available online: https://www.health.mil/Reference-Center/Meeting-References/2022/03/30/Defense-Health-Agency-Update-on-Virtual-Health (accessed on 4 August 2022).
- Bandic, J.; Kovacevic, S.; Karabeg, R.; Lazarov, A.; Opric, D. Teledermoscopy for Skin Cancer Prevention: A Comparative Study of Clinical and Teledermoscopic Diagnosis. Acta Inform Med 2020, 28, 37–41, doi:10.5455/aim.2020.28.37-41.
- Holmes, G.A.; Vassantachart, J.M.; Limone, B.A.; Zumwalt, M.; Hirokane, J.; Jacob, S.E. Using Dermoscopy to Identify Melanoma and Improve Diagnostic Discrimination. Pract. 2018, 35, S39–S45.
- Gall, R.; Bongiorno, M.; Handfield, K. Skin Cancer in the US Military. Cutis 2021, 107, 29–33. https://doi.org/10.12788/cutis.0153.
- Powers, J.G.; Patel, N.A.; Powers, E.M.; Mayer, J.E.; Stricklin, G.P.; Geller, A.C. Skin Cancer Risk Factors and Preventative Behaviors among United States Military Veterans Deployed to Iraq and Afghanistan. Investig. Dermatol. 2015, 135, 2871–2873. https://doi.org/10.1038/jid.2015.238.
- Riemenschneider, K.; Liu, J.; Powers, J.G. Skin Cancer in the Military: A Systematic Review of Melanoma and Nonmelanoma Skin Cancer Incidence, Prevention, and Screening among Active Duty and Veteran Personnel. Am. Acad. Dermatol. 2018, 78, 1185–1192. https://doi.org/10.1016/j.jaad.2017.11.062.
