Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Oncology
Immunotherapy is an ever-expanding field in lung cancer treatment research. The lung cancer treatment paradigm has been completely changed by immunotherapy; however, less than half of the treated patients obtain a response, and an even smaller proportion achieve a long survival.
- lung cancer
- immunotherapy
- emerging immune checkpoint inhibitors
1. Introduction
The last decade has seen the rapid development of immunotherapy and its role as a crucial strategy in cancer treatment, particularly in the field of lung cancer. The immune system closely interacts with tumors along the entire process of cancer onset and progression. Tumor cells develop numerous ways to escape immune cell recognition and removal by regulating their antigen presentation, through the secretion of immunosuppressive cytokines such as interleukin (IL)-10 and transforming growth factor (TGF)-β, or by affecting their metabolism, causing an alteration in the tumor microenvironment (TME) [1,2,3,4,5,6]. However, the most potent mechanism to limit normal anti-tumor immune responses is the activation of immune checkpoint pathways such as cytotoxic T-lymphocyte antigen 4 (CTLA-4), programmed death 1 (PD-1) and programmed death ligand-1 (PD-L1) [7,8,9]. In fact, the CTLA-4 and PD-1/PD-L1 blockade was capable of restoring the host’s T cell-mediated immune system response, suppressed by the tumour [9]. These findings paved the way to the development of immune checkpoint inhibitors (ICIs), which take advantage of the host’s immune system to enhance anti-tumor activity. Clinical efficacy and durable responses were recorded in several tumour types [10,11,12,13], especially in non-small-cell lung cancer (NSCLC) [14]. In patients with NSCLC without a driver mutation and in those with small-cell lung cancer (SCLC), immunotherapy in the form of ICIs is currently the cornerstone of treatment [15,16]. In NSCLC PD-L1, despite representing to date the most reliable predictive biomarker of response to immunotherapy, it fails to select the right subset of patients who would benefit from this treatment. Indeed, only a limited number of patients respond to ICI, and also in the event of a lasting response they eventually experience disease progression. Moreover, due to the paucity of effective second-line treatments, the mortality rate of this disease remains still high [17,18,19]. In addition, about 15–25% of patients treated with ICIs developed serious immune-related adverse events (irAEs), which can sometimes be fatal [20,21,22]. Therapy strategies which involve the combination of ICI with each other or with other drugs (i.e., chemotherapy, target therapy, agents, poly ADP ribose polymerase (PARP) inhibitors) or local treatment, have been adopted to overcome these hindrances, resulting in increased clinical responses. However, as many patients show primary or acquired resistance to ICIs [23,24,25,26], a great interest is addressed to discover novel targets. The next generation immune checkpoints, such as lymphocyte activation gene-3 (LAG-3), T cell immunoglobulin (Ig) and Immunoreceptor Tyrosine-Based Inhibitory Motif (ITIM) domain (TIGIT), T cell immunoglobulin and mucin-domain containing-3 (TIM-3), V-domain Ig suppressor of T cell activation (VISTA), B7 homolog 3 protein (B7-H3), inducible T cell costimulatory (ICOS), and B and T cell lymphocyte attenuator (BTLA), appear to be promising therapeutic strategies with the possibility of future clinical applications [27,28,29,30,31,32,33]. Furthermore, the addition of novel ICIs, which do not exhibit overlapping mechanisms of action with those already in use, could improve efficacy and decrease toxicity.
2. Current Role of Immunotherapy in Lung Cancer
In the past seven years, numerous ICIs received approval for lung cancer treatment in different settings of disease, particularly for NSCLC. Indeed, ICIs commenced as a second-line treatment strategy for metastatic NSCLC. The therapeutic indications were then extended to the first-line advanced settings and later also to the earlier stages, including both unresectable and resectable disease (Figure 1).
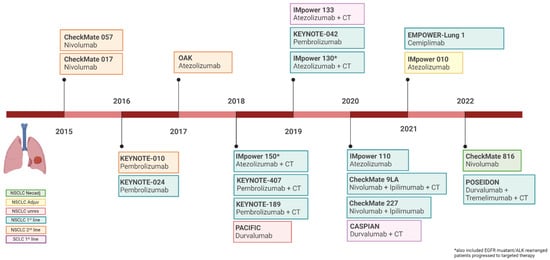
Figure 1. Timeline of Food and Drug Administration approval of immune checkpoints inhibitors in lung cancer. Image created with BioRender.com, accessed on 5 July 2022.
The most recent Food and Drug Administration (FDA) approval of ICI in NSCLC stems from the results of the CheckMate 816 trial [34]. In this study, three cycles of neoadjuvant chemotherapy plus nivolumab (anti-PD-1) in patients with resectable disease resulted in a significantly higher percentage of pathological complete response (pCR) and longer event-free survival (EFS) than chemotherapy alone [34]. The phase III trial IMpower 010 compared atezolizumab (anti-PD-L1) versus best supportive care (BSC) in patients with resectable stable IB-IIIA NSCLC undergoing complete surgical resection and subsequent adjuvant platinum-based chemotherapy [35]. The superiority of atezolizumab in disease-free survival (DFS), allowed its recent FDA approval in adjuvant setting for patients with II-III stage NSCLC, harboring PD-L1 positivity [36].
For unresectable stage III NSCLC, a placebo-controlled phase III trial revealed that treatment with durvalumab for 12 months significantly improves progression-free survival (PFS) (17.2 vs. 5,6 months) and OS (not reached [NR] vs. 28.7 months) for patient with PD-L1 expression and who had not progressed to concurrent chemoradiation. This results were confirmed at 5-year follow up [37,38].
In the advanced NSCLC setting, nivolumab was the first drug to obtain the FDA accelerated approval in 2015 as a second-line treatment after progression to platinum-based chemotherapy. Two-phase III clinical trials, CheckMate 017 and 057, showed the superiority of nivolumab compared with docetaxel in terms of objective response rate (ORR) and overall survival (OS) [39,40]. In the wake of these results, two more ICIs, pembrolizumab (anti-PD-1) and atezolizumab, displayed a comparable efficacy and have been subsequently approved for the second-line setting [41,42].
However, the big breakthrough came with the following phase III clinical trials, which widened the first-line treatment opportunities for patients with metastatic NSCLC. Indeed, ICIs proved to be superior alone or in combination with platinum-based chemotherapy over standard treatment. ICIs not only improved response rates (RR) and recorded the longest OS ever achieved, but ensured also a long-lasting survival benefit. In the KEYNOTE-024 study, pembrolizumab significantly improved PFS and OS in patients with advanced NSCLC and PD-L1 expression on at least 50% of tumor cells [43]. Likewise, atezolizumab and cemiplimab (anti-PD-1), tested in NSCLC patients with high PD-L1 expression, resulted in significantly longer OS than platinum-based chemotherapy [44,45]. Based on these results FDA approved pembrolizumab, atezolizumab, and most recently cemiplimab, for the first line treatment of adult patients with metastatic NSCLC and PD-L1 expression ≥50%, without genomic tumor aberration on epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK).
Many chemo-immunotherapy combinations have been explored, showing to be both efficacious and well-tolerated. The combination of pembrolizumab with carboplatin and pemetrexed received accelerated FDA approval in 2017 based on the phase II study KEYNOTE-021 cohort G [46]. The subsequent phase III trial KEYNOTE-189 confirmed the latter results, by testing pembrolizumab versus placebo plus four cycles of platinum-based chemotherapy and pemetrexed (continued as maintenance therapy), on patients with untreated, nonsquamous, EGFR and ALK wild-type NSCLC [47]. In the experimental arm, the median PFS and OS were 9.0 and 22.0 months versus 4.9 and 10.7 months recorded in the control arm. Pembrolizumab, added to chemotherapy, showed a good safety profile and also improved RR (48.0% vs. 19.4%) and the median duration of response (DOR) (12.4 vs. 7.1 months) [47]. Likewise, pembrolizumab added to platinum-based chemotherapy plus paclitaxel or nab-paclitaxel resulted in significantly longer OS (15.9 vs. 11.3 months) and PFS (6.4 vs. 4.8 months) than chemotherapy alone in untreated metastatic, squamous NSCLC regardless PD-L1 expression, thus receiving FDA approval [48]. Moreover, also atezolizumab obtained FDA approval with the phase III study IMpower 130 for previously untreated metastatic, non-squamous, NSCLC patients [49]. Better median PFS and OS (18.6 vs. 13.9 months) and RR (49.2% vs. 31.9%) were observe in the combination arm compared with the chemotherapy alone group [36]. An additional combination based on cemiplimab plus platinum-doublet chemotherapy has been evaluated in the phase III EMPOWER-Lung 3 study, as first-line treatment for advanced NSCLC, irrespective of PD-L1 expression or histology [50]. Cemiplimab plus chemotherapy recorded a median OS of 21.9 months compared to 13.0 months with chemotherapy alone and has been accepted for review by the FDA.
A further immunotherapy strategy that showed advantage in treating lung cancer is combining PD-1/PD-L1 and CTLA-4 inhibitors. In the phase III CheckMate 227 trial, previously untreated NSCLC patients were randomized to receive in a 1:1:1 radio nivolumab plus ipilimumab, nivolumab alone, or chemotherapy [51]. In PD-L1 positive patients nivolumab plus ipilimumab showed a median OS of 17.1 months compared to 14.9 months with chemotherapy. ICIs combination recorded a higher RR (35.9% vs. 30.0%) and DOR (23.2 vs. 6.2 months) than chemotherapy alone. Despite exhibiting better outcomes than chemotherapy also in PD-L1 negative NSCLC, FDA approved the immunotherapy combination as first-line therapy only for PD-L1 positive disease [52].
Eventually, dual-checkpoint blockade combined with chemotherapy was investigated in a phase III study, CheckMate 9LA, including treatment-naïve NSCLC patients regardless of PD-L1 expression and tumor histology [53]. Patients were randomized to receive chemotherapy alone for four cycles and eventually maintenance with pemetrexed or a combination of nivolumab with ipilimumab every 6 weeks and concurrent platinum-doublet chemotherapy for only two cycles. This new chemo-immunotherapy approach met its primary endpoint, by recording a median OS of 15.6 months in the experimental arm and 10.9 months in the control group. The combination also improved PFS (6.7 vs. 5.0 months) and RR (38% vs. 25%) in the face of a higher grade toxicity (≥3 in 47% vs. 38%) and greater discontinuation rate (19% vs. 7%) compared with chemotherapy alone. The chemo-immunotherapy regimen was recently FDA approved in 2020 [54]. Very recently, FDA approved tremelimumab in combination with durvalumab and platinum-based chemotherapy for patients with metastatic NSCLC with no sensitizing EGFR, ALK genomic tumor aberrations. The phase III POSEIDON study, enrolled patients to receive the following: tremelimumab plus durvalumab and platinum-based chemotherapy for four cycles, followed by durvalumab until progression and one additional tremelimumab dose; durvalumab plus chemotherapy for four cycles, followed by durvalumab; or chemotherapy for up to six cycles ± maintenance pemetrexed [55]. Durvalumab plus tremelimumab and chemotherapy significantly improved PFS (6.2 v 4.8 months) and OS (14.0 v 11.7 months) compared to chemotherapy alone.
Unlike the success achieved in NSCLC, the application of ICIs in SCLC remains limited and not very advantageous. The only innovation relates to the implementation of first line extended-stage SCLC (ES-SCLC) therapy, which saw the addition of two anti-PD1 inhibitors to standard platinum-based chemotherapy. Atezolizumab has been approved in 2019 after phase III trial IMpower 133, which accrued patients with previously untreated ES-SCLC to receive four cycles of standard carboplatin plus etoposide and concurrent atezolizumab or placebo followed by maintenance atezolizumab or placebo [56]. The addition of Atezolizumab to chemotherapy improved median OS (12.3 vs. 10.3 months), PFS (5.2 vs. 4.3 months) and patient’s quality of life, without increase the toxicity. After about a 1 year, durvalumab received a similar approval based on the phase III CASPIAN trial. Patients were randomized to receive standard chemotherapy (platinum plus etoposide) alone or in combination with durvalumab (continued as maintenance therapy) ± tremelimumab. A median OS of 13.0 months versus 10.3 months has been recorded in the experimental arm compare to chemotherapy alone group, with 34% versus 25% of patients alive at 18 months, respectively [44]. These results made the chemo-immunotherapy combination the first intervention capable of improving survival in ES-SCLC over three decades.
PD-L1 Expression Levels and Outcome Related
PD-L1 is currently one of the few recognized and approved biomarkers predictive of response to immunotherapy. Despite the confirmed benefit of assigning ICIs according to PD-L1 expression, the latter biomarker alone is still inadequate to select the right candidates for immunotherapy [57]. In NSCLC, patients with higher levels of PDL1 expression tend to respond more favorably to the ICIs [58,59]. Different diagnostic immunohistochemistry test, with variations in cut-off values have been used to establish PD-L1 expression [60,61,62,63].
The frequency of PD-L1 expression in lung cancer has been reported by several authors [64,65,66]. In the largest real-world study conducted on 2368 advanced NSCLC patients, 22% had PD-L1 TPS ≥ 50%, 52% PD-L1 TPS ≥ 1%, and 48% PD-L1 TPS < 1%. Prevalence of PD-L1 TPS ≥ 50% and TPS ≥ 1% were similar across geographic regions ranging from 21–24% and 47–55%, respectively [64]. Another study assessed PD-L1 expression in 264 cases of NSCLC showing: high PD-L1 expression (≥50%) in 29.5% of cases, low (1–49%) in 43.9% and absent (<1%) in the 26.5% [66]. Skov et al., in their prospective study, included 819 patients with NSCLC reported a PD-L1 ≥ 1% positive cells in the 63% of NSCLC patients and PD-L1 ≥ 50% in 30% [66].
Unlike NSCLC, in other types of lung cancer such as SCLC PD-L1 expression levels are understudied, with contradictory reports of expression status [67].
Most recently Xu et al. conducted a meta-analysis to evaluate the efficacy of ICI monotherapy or combined with chemotherapy and estimate the predictive value of PD-L1 expression in predicting the response from these treatment [67]. Results showed better OS, PFS and ORR with anti-PD-1/PD-L1 monotherapy compared with chemotherapy in the intention-to-treat population (ITT) and emphasized the value of positive PD-L1 expression in predicting improvement of clinical outcome from anti-PD-1/PD-L1 treatment. Indeed, better efficacy outcomes correlated with higher PD-L1 levels (mainly PD-L1 ≥ 50%), whereas no statistical survival benefit was observed for the PD-L1 < 1% population who received anti-PD-1/PD-L1 monotherapy compared to chemotherapy alone. Subgroup analyzes showed significant improvement in ORR from ICI in patients with PD-L1 ≥ 50%, no difference in patients with PD-L1 < 1%, and better ORR with chemotherapy versus ICI monotherapy in patients with PD-L1 expression ranging from 1 to 49%.
Similar results derived from Liu et al.’s metanalysis [67]. In this study, in patients with PD-L1 ≥ 1%, ten immunotherapy combinations were associated with significantly prolonged OS and PFS (the latter especially with anti-PD-1 plus chemotherapy) compared with chemotherapy. In patients with PD-L1 1–49%, seven immunotherapy combinations also significantly improved OS and PFS compared with chemotherapy. In patients with PD-L1 ≥ 50%, nine immunotherapy combinations (except for durvalumab-tremelimumab), showed significantly higher OS and PFS benefit than standard chemotherapy [67].
Finally, another metanalysis investigated the efficacy and safety of dual ICIs ± other therapies. An improved OS with the combination therapy in the ITT population was shown. However, according to the analysis, no statistically significant difference between the two groups was found for patients with PD-L1 < 1%, thus narrowing the benefit from this combination for PD-L1 ≥ 1% expression [68].
This entry is adapted from the peer-reviewed paper 10.3390/cancers14246145
This entry is offline, you can click here to edit this entry!
