Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Infectious Diseases
Resistance to antimicrobials and particularly multidrug resistance is one of the greatest challenges in the health system nowadays. The continual increase in the rates of antimicrobial resistance worldwide boosted by the ongoing COVID-19 pandemic poses a major public health threat. Different approaches have been employed to minimize the effect of resistance and control this threat.
- antimicrobial resistance (AMR)
- multidrug-resistant (MDR) bacteria
- therapeutic strategies
1. Introduction
Multiple drug resistance (MDR) is identified by the World Health Organization (WHO) as one of the most serious threats to global health, food security and development [1]. It can affect anyone, at any age and in any country. It is now a major global public health challenge that arises for multiple reasons, including overpopulation, increased global migration, and selective pressure from increased use of antibiotics. The WHO has listed antibiotic resistance as one of the three most important public health threats in the 21st century (Figure 1) [2]. It estimates that infections caused by multidrug-resistant (MDR) bacteria (bacteria that are simultaneously resistant to three or more kinds of antibiotics used in a clinic) kill about 700,000 people worldwide each year, and that this number might rise to 10 million fatalities by 2050, exceeding the current yearly number of cancer-related deaths, if no action is taken [3,4,5].
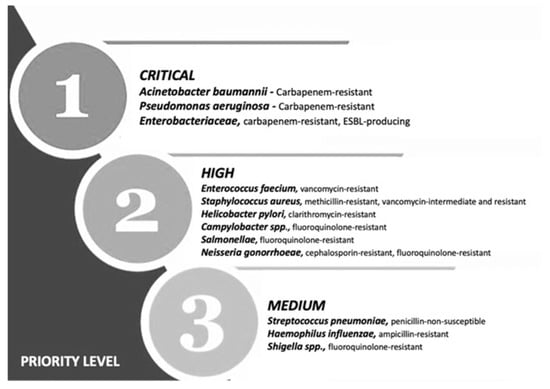
Figure 1. Priority list for development of new antibiotics according to the World Health Organization. Adapted from (Zyman A; et al., 2022) [6].
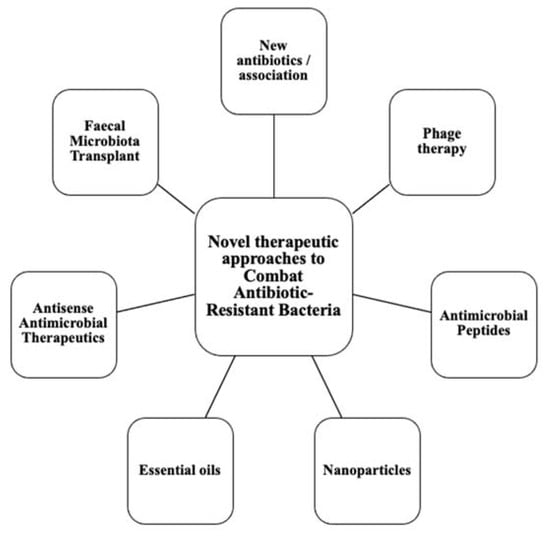
This calls for the scientific community to design new antibiotics or innovative therapeutic approaches for treating critical priority antibiotic-resistant infections [5]. Common bacterial pathogens, such as Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Escherichia coli, etc. have evolved and become resistant to multiple antibiotics, and their treatment is now becoming problematic (Figure 1). An increasing number of infections, such as pneumonia, tuberculosis, gonorrhea, or salmonellosis are becoming more difficult to treat as the antibiotics used to treat these infections lose their effectiveness. Unfortunately, the inadequate and irregular administration of antibiotics also contributes significantly to the development of antibiotic resistance, which leads to prolonged hospitalizations and increased medical expenses [7]. Additionally, several studies have reported that widespread use of antibiotics for hospitalized COVID-19 patients without established secondary infection was markedly increased, thereby leading to an increase in antimicrobial resistance through driving selection of MDR organisms [8,9,10,11]. The Centers for Disease Control and Prevention (CDC) in its special report of the year 2022 entitled “COVID-19: U.S. Impact on Antimicrobial Resistance” also concluded that the threat of antimicrobial-resistant infections is not only still present but has worsened [12]. Therefore, there is an urgent need for new classes of antimicrobials and other innovative approaches to fight against the emergence of MDR bacteria and escape the therapeutic impasse. In addition to traditional approaches, several new approaches (Figure 2), such as bacteriophages, antimicrobial peptides, essential oils and host-oriented therapies show great potential.
Figure 2. Alternatives therapeutic approaches to conventional antibiotics.
2. Phage Therapeutics
Phage therapy dates back to the beginning of the 20th century, even before Alexander Fleming’s discovery of penicillin in 1928 [68]. The first phage activity dated back to 1896, when Ernest Hankin reported that the waters from the rivers Ganges and Yamuna in India possessed antibacterial activity against Vibrio cholerae [69]. In the late 1910s, and following initial work by the English bacteriologists Ernest Hankin and Frederick Twort, a French microbiologist from the Pasteur Institute (Felix d’Herelle, 1917) identified viruses that specifically and selectively parasitized bacteria and named them “bacterium eaters” (bacteriophages) [70,71]. It was d’Herelle who first developed the notion of using phages therapeutically to treat bacterial infection with encouraging results [69]. However, since the discovery and development of antibiotics, Phage therapy was largely abandoned in the Western world due to the efficacy and promise held by antibiotics, with the exception of the Soviet Union and some Eastern European countries [69]. Recently, and in the face of the rapid emergence of resistant bacteria, phages (estimated to exceed 1031 particles) have re-emerged as alternative and complementary therapies to control bacterial infections [72]. Thus, phage therapy has shown to be an interesting alternative in the fight against multi-drug resistant bacteria [73]. Phages or bacteriophages are lytic viruses that exclusively and specifically infect bacterial species, showing bactericidal effects against both Gram-positive and Gram-negative bacteria [74,75]. In contrast, some tend to be specific to a particular species or strain of bacteria [76]. The tailed double-stranded DNA phages (order Caudovirales) are the most studied group and are thought to account for 96% of all phages and are easily isolated from various environmental sources (soil, wastewater, and aquatic environments) [73]. By adhering, via tail proteins, to specific surface receptors of bacteria, phages insert their genetic material into their bacterial hosts [69]. Several types of life cycles can be triggered by bacteriophages, of which the two most frequent are the lytic and lysogenic cycles [68]. During the lysogenic cycle, the virion DNA is incorporated in the bacterial genome. The resulting prophage replicates its genetic material within the bacterial cell without damaging it until the lytic cycle is trigger [68,77]. Undoubtedly, prophages are supposed to be shunned and lytic phages are selected. During the lytic cycle, the phage uses the cellular machinery to yield as many as 20,000 new virions per infected bacterial cell in optimal conditions [68]. These phages secrete lytic enzymes (endolysins) that hydrolyze the bacterial cell wall to ensure phage release [77,78]. Since then, it has become clear that phage therapy and the application of its endolysins offer the possibility to apply more specific antibacterial treatments and propose a potential solution to the problem of antibiotic resistance [79]. The table below (Table 1) shows some advantages of applying phage therapy to fight bacterial infections.
Table 1. Main advantages of bacteriophages for infections control.

Applications in Medicine
Before the dawn of antibiotics, phage therapy had been used to treat a broad range of bacterial infection diseases, including cholera [89,90,91], pediatric dysentery [92], bubonic plague [93], typhoid fever, skin and surgical site infections, peritonitis, septicemia, and external otitis [92,93]. However, in 1934, the failed attempts to reproduce positive findings had inspired the opposition from the Council on Pharmacy and Chemistry of the American Medical Association [91]. This opposition has not prevented parts of Eastern Europe (such as Georgia, Poland and Russia) from continuing to use phages in routine medical practice and today provide us with a rich source of empirical data [94]. For example, The Eliava Institute of Bacteriophage, Microbiology, and Virology in Georgia is one of the longest-running institutions where phage therapy has been provided to frequent bacterial diseases related to urology, pediatrics, internal medicine, and gynecology [71]. Recently, phage therapy has been re-employed in the United States and Europe, for the treatment of infections related to burn injuries or soft tissue and skin trauma, osteomyelitis, sepsis, bacteremia, and otitis media as well as urinary tract, pulmonary, and prosthetic device-associated infections, especially when mono- or multi-infected patients with multi-resistant bacteria are without effective treatment options or are terminally ill [71,95]. In Table 2 below, we quote the references of the main applications of phage therapy (as an adjuvant or alternative therapy to antibiotics) conducted on human patients infected with various types of MDR bacteria [2]. Results from these studies indicate that this therapy has immense potential with applications in human medicine.
Table 2. List of references of the main applications of phage therapy against multidrug-resistant bacteria classified according to the WHO priorities.

3.2. Limitations
Although phage therapy has come a long way, and is considered a promising alternative to antimicrobial agents, they have a dark, poorly explored side (Table 3). These limitations complicate the design of clinical protocols, undermine confidence in phage application, and need to be cleared before establishing successful phage therapy on a global scale.
Table 3. Limits of application of phage therapy in modern human medicine.

Conclusions
A new era is beginning today with the long-awaited growing research of novel anti-infectious approaches against MDR bacteria. These therapeutic approaches are definably a potent non-antibiotic option to curtail the huge increase in antibiotic resistant bacteria that we are facing nowadays. It cannot be denied that mechanisms of action of these therapies are complicated to elaborate and that clinical trials are not complete enough to provide valid and concise information. However, all efforts made in making these treatments as a clinical routine must be done with caution taking in consideration the efficacy and safety of each therapy. In the end, we are convinced that the knowledge and mastery of resistance patterns and mechanisms of action will allow clinicians to increasingly drive antimicrobial treatment towards an individualized and precise medical approach.
This entry is adapted from the peer-reviewed paper 10.3390/antibiotics11121826
This entry is offline, you can click here to edit this entry!