Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic, inflammatory, polygenic, multifactorial, and multifactorial illness with unknown etiology. Studies have reported extraintestinal manifestations (EIMs) or issues in several organ systems, including musculoskeletal, dermatologic, ocular, pulmonary, renal, and hepatobiliary systems.
- ocular extra-intestinal manifestation
- uveitis
- episcleritis
- conjunctivitis
- inflammatory bowel disease
- Crohn's disease
- ulcerative colitis
- IBD
1. Introduction
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is a chronic, inflammatory, polygenic, multifactorial, and multifactorial illness with unknown etiology. Studies have reported extraintestinal manifestations (EIMs) or issues in several organ systems, including musculoskeletal, dermatologic, ocular, pulmonary, renal, and hepatobiliary systems [1]. Furthermore, the existing literature is inconsistent in terms of whether these EIMs are more associated with CD or UC. Ocular EIMs (O-EIMs) are reported in 4–12% of patients with IBD, and the rate was recorded up to 29% in some cohorts [2]. EIMs are more prevalent in CD than in UC. Ocular symptoms were observed from mild conjunctivitis and episcleritis to severe inflammation, such as scleritis and uveitis. Uveitis is typically more serious and causes vision loss, whereas episcleritis is a benign condition. The most prevalent ocular IBD symptoms are episcleritis (2–5%) and uveitis (0.5–3.5%) [3][4]. Uveitis is a uveal tract inflammation involving the iris, ciliary body, and choroid and may lead to visual impairments [5][6]. According to the predominant site of inflammation, uveitis can be classified as anterior, middle, posterior, or panuveitis. Patients with IBD exhibit bilateral anterior uveitis with a gradual onset [7][8] and are unrelated to IBD activity.
Nonetheless, the prevalence reported by research varies considerably, which makes it difficult to determine if O-EIMs are more prevalent in patients with CD or UC. Although a higher prevalence of O-EIMs has been demonstrated in CD patients compared with UC patients [9], the results are controversial [10][11]. CD and UC represent two separate disease entities. CD can affect any part of the GI tract, but the large and small intestines are most affected, while UC mainly affects the colon and rectum. CD is more severe than UC, yet UC is significantly more prevalent worldwide. Moreover, the risk factors of CD and UC were substantially distinct [12].
2. Association of O-EIMs with IBD
Figure 1 shows the forest plot of the prevalence of O-EIMs in patients with CD or UC. Some studies provided information on indeterminate IBD, which was excluded from the meta-analysis because it could not be categorized into CD or UC. The meta-analysis demonstrated an association between uveitis and CD, and adults with CD have a significantly elevated risk of uveitis (pooled OR 1.603, 95% CI 1.254–2.049, p < 0.001) (Figure 1A). Cochran’s chi-square test (p < 0.001) and I2 statistic (I2 = 76.116%) revealed significant heterogeneity among studies. Nonetheless, the prevalence of episcleritis and conjunctivitis had no significant difference between CD and UC (Figure 1B,C).
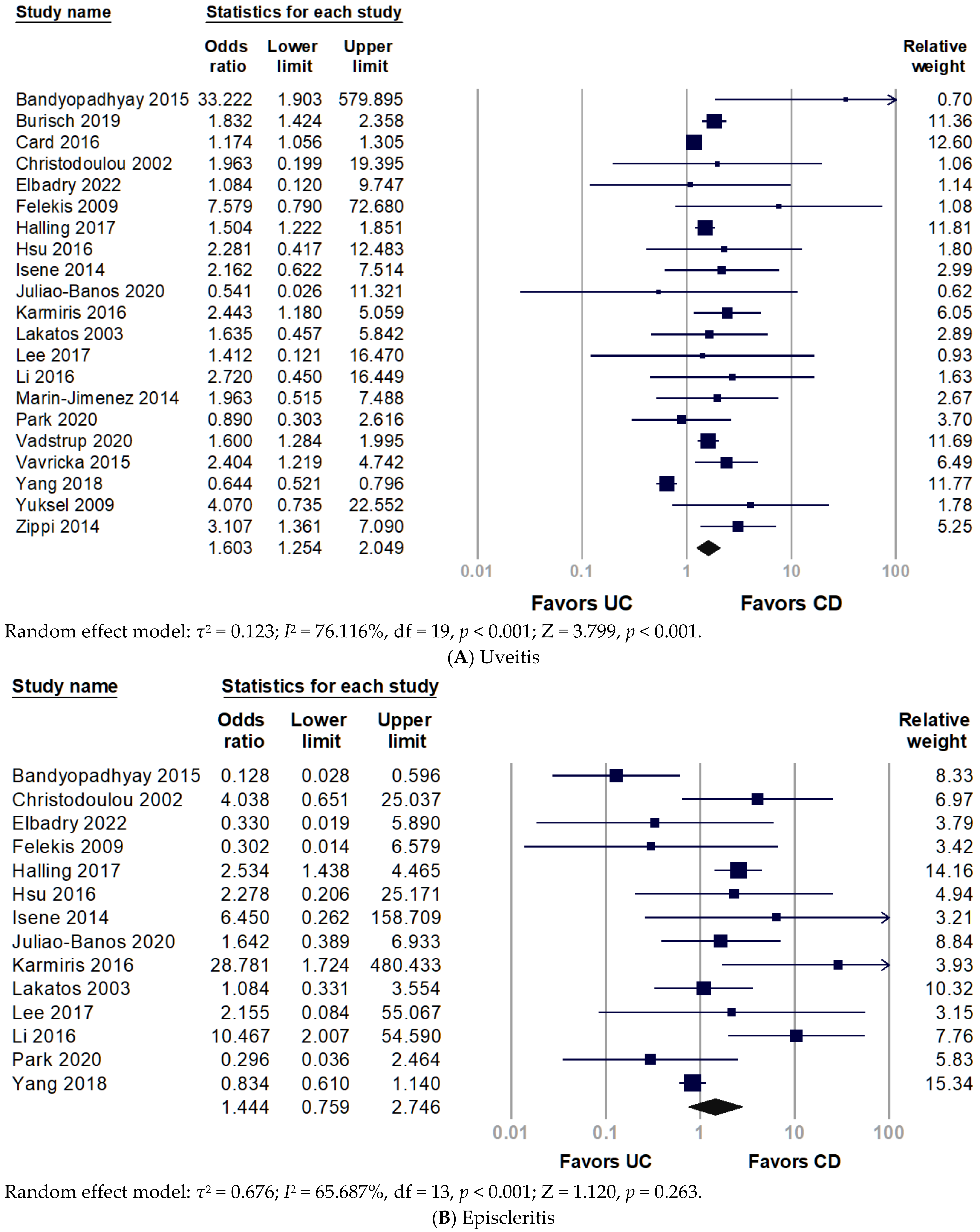
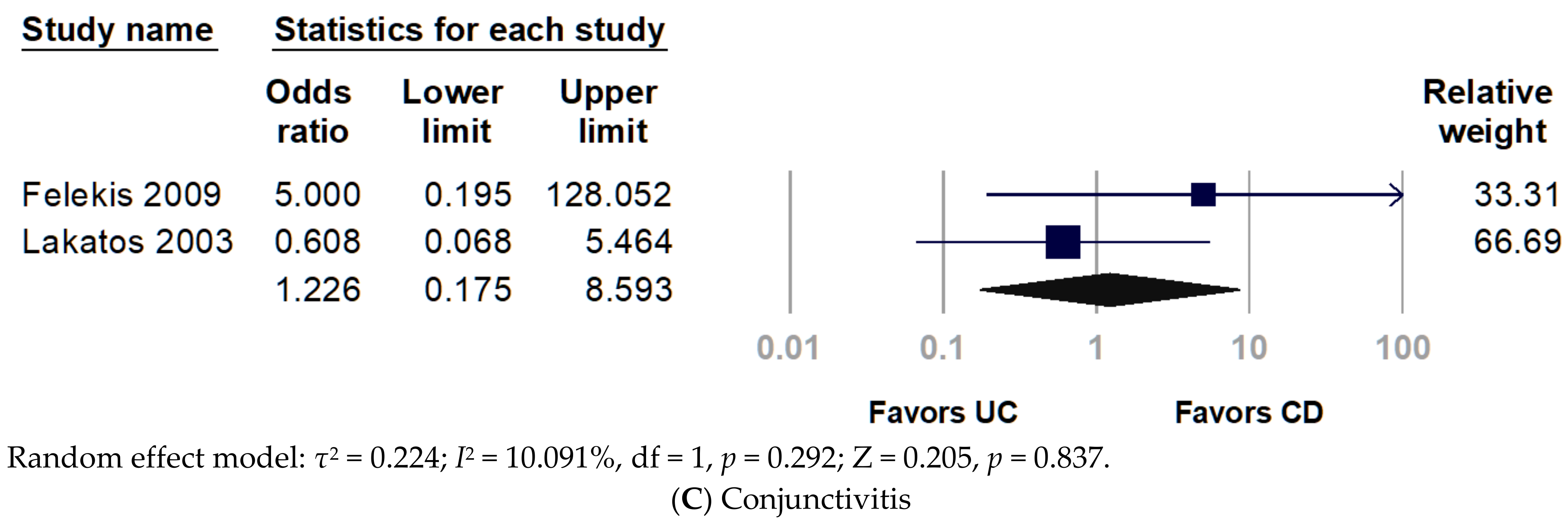
Figure 1. Forest plot for prevalence of ocular extra-intestinal manifestation among adult patients with inflammatory bowel disease: (A) uveitis; (B) episcleritis; (C) conjunctivitis. CD, Crohn’s disease; UC, ulcerative colitis.
3. Stratification with World Regions
To investigate the disparity between world region and race, researchers divided included studies into Asia, Central Asia, and Europe. Figure 2 presents the subgroup analyses by region of the study population. The pooled analysis of the Asian population revealed non-significantly increased odds of uveitis in patients with CD (pooled OR 1.428, 95% CI 0.612–3.334, p = 0.410). Only two studies in Central Asia were involved in the analysis, without significant results, but they presented a trend that uveitis favored in patients with CD over UC (pooled OR 2.468, 95% CI 0.640–9.525, p = 0.190). Conversely, European studies indicated a significantly increased prevalence of uveitis in patients with CD (pooled OR 1.683, 95% CI 1.377–2.056, p < 0.001). For episcleritis, the frequency of episcleritis did not differ between CD and UC (Figure 1B). Nonetheless, European populations had a significantly higher prevalence of episcleritis in patients with CD than UC (pooled OR 2.401, 95% CI 1.112–5.184, p = 0.026) (Figure 2B).
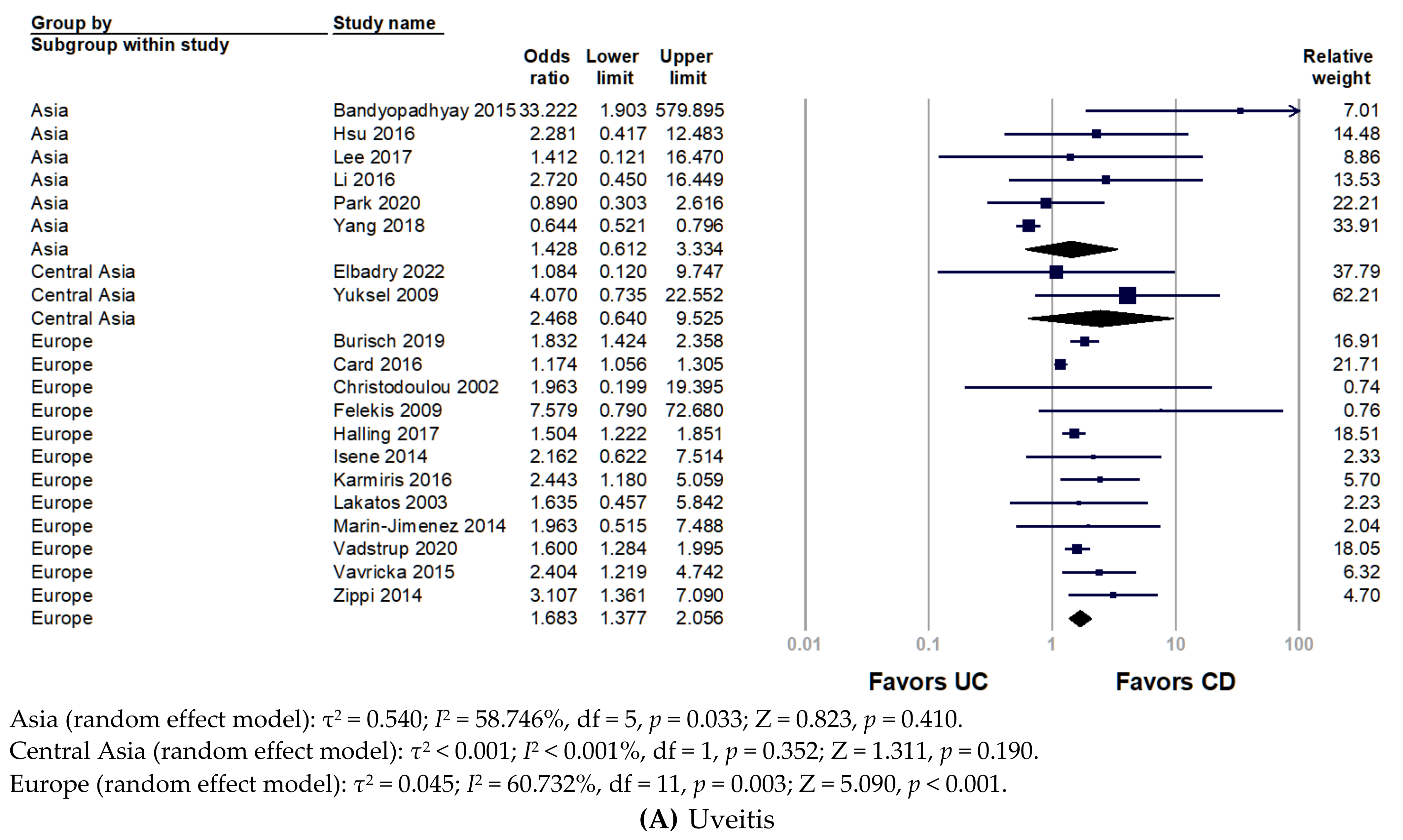
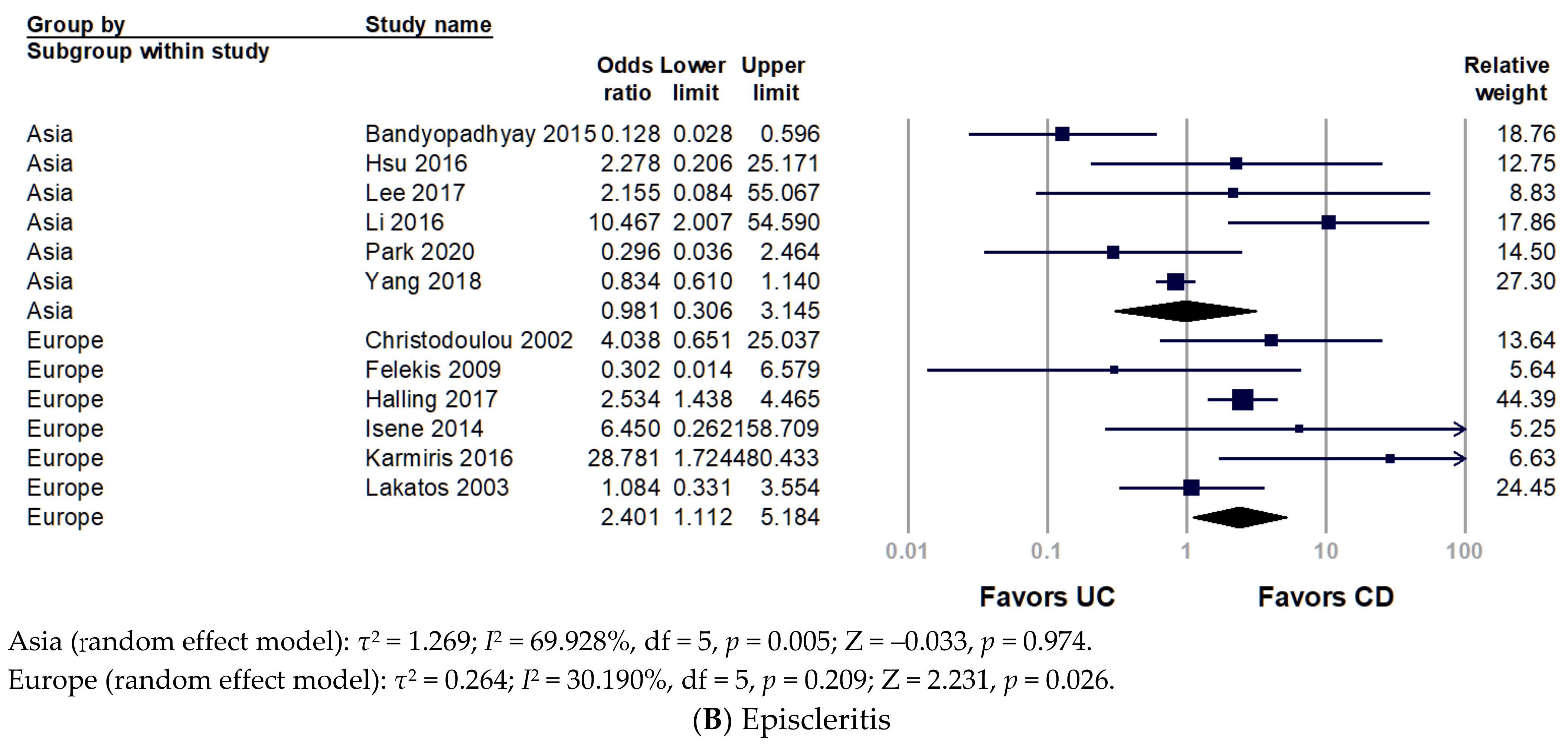
Figure 2. Forest plot for the prevalence of ocular extra-intestinal manifestation among adult patients with inflammatory bowel disease stratified by world region: (A) uveitis; (B) episcleritis. CD, Crohn’s disease; UC, ulcerative colitis.
4. Chronological Analysis
Only two studies showed uveitis before and after IBD diagnosis. The pooled analysis indicated no significant finding (pooled OR 2.152, 95% CI 0.136–33.964, p = 0.586) since extreme heterogeneity (I2 = 99.516%) (Figure 4).
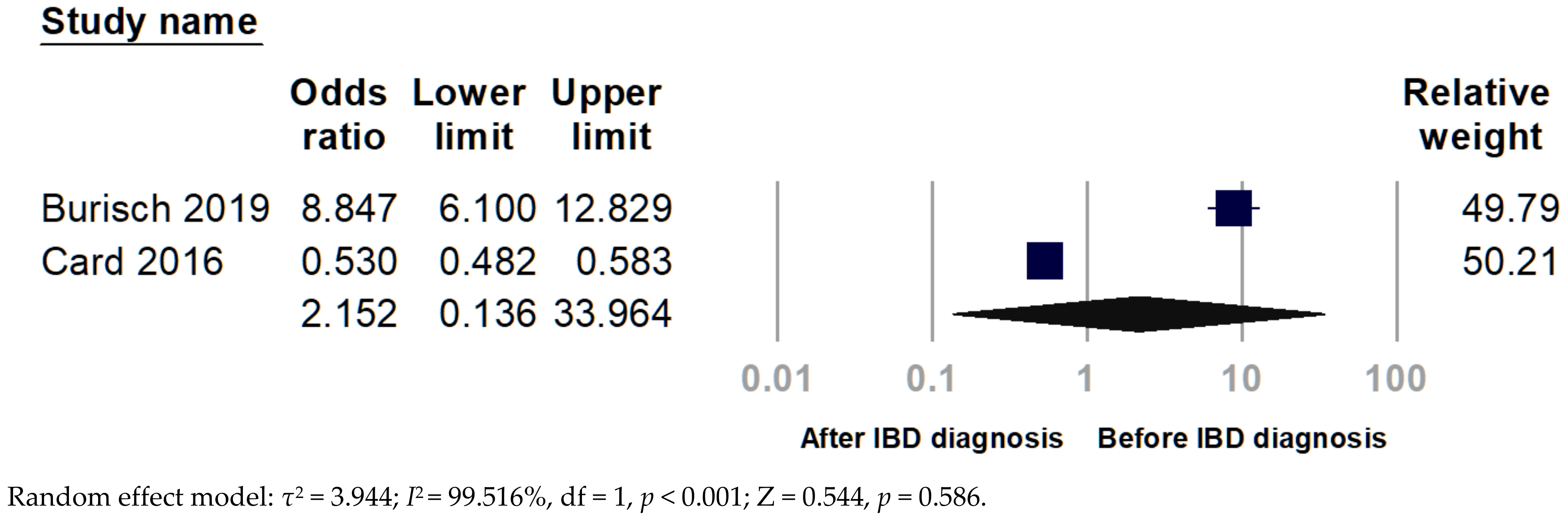
Figure 3. Forest plot for the chronological relationship between uveitis and inflammatory bowel disease (IBD).
5. Period Prevalence of O-EIMs
Figure 4 illustrates the overall prevalence of uveitis, episcleritis, and conjunctivitis. The period prevalence of uveitis in CD and UC ranged from 0–21.57% and 0–4.76%, respectively. While the period prevalence of episcleritis in CD and UC was 0–5.41% and 0–24.14%, respectively.
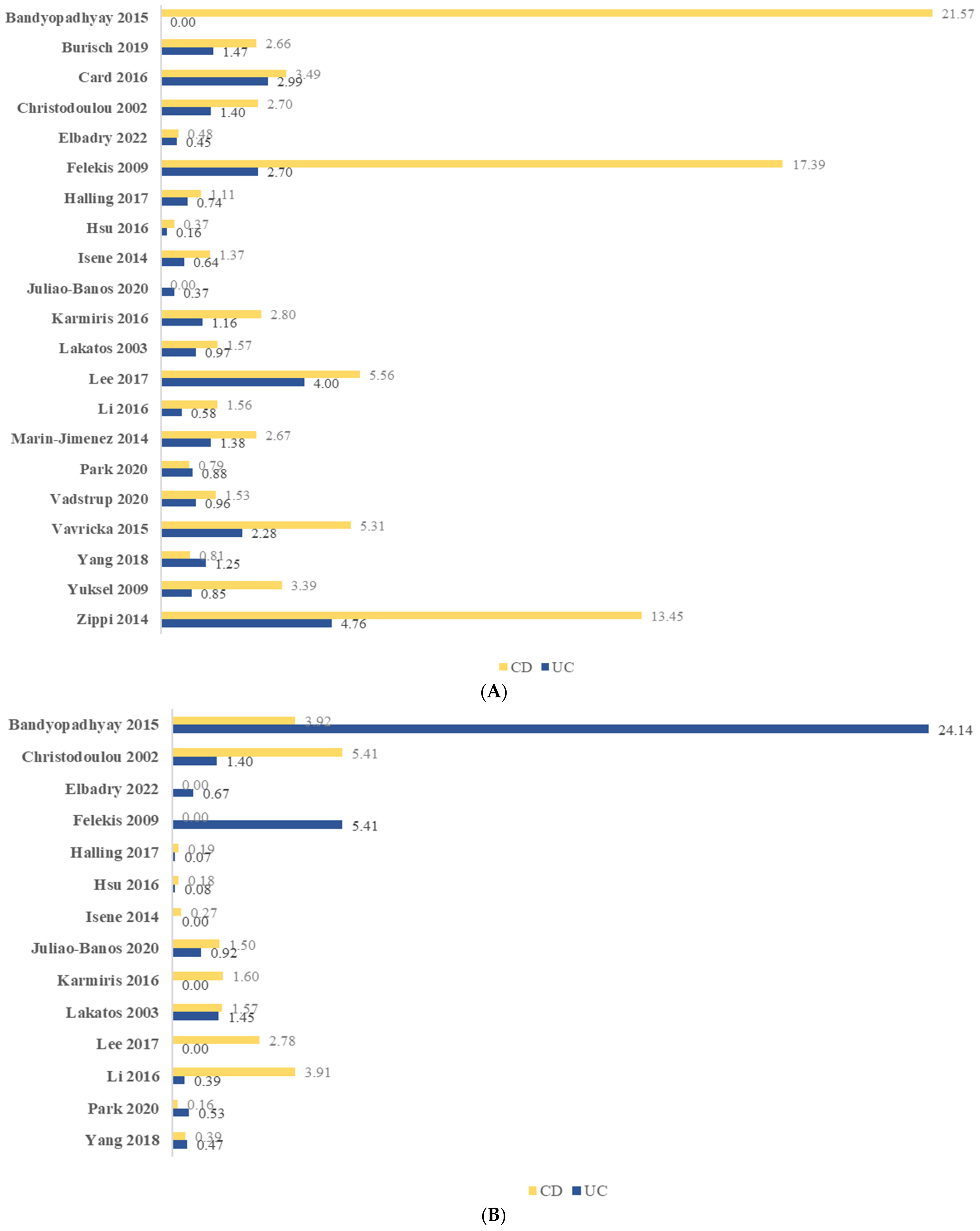
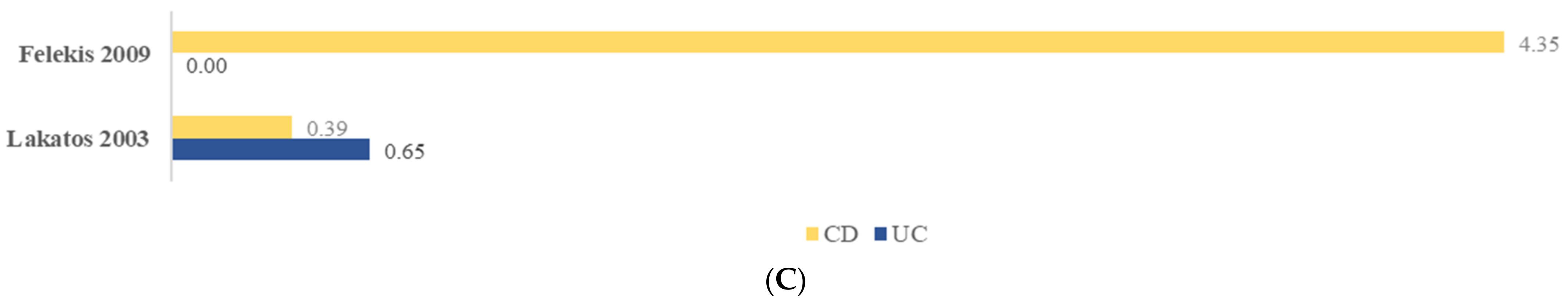
Figure 4. Period prevalence (%) of ocular manifestation among adult patients with inflammatory bowel disease: (A) uveitis; (B) episcleritis; (C) conjunctivitis. CD, Crohn’s disease; UC, ulcerative colitis.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph192315683
References
- Ott, C.; Scholmerich, J. Extraintestinal manifestations and complications in IBD. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 585–595.
- Greuter, T.; Vavricka, S.R. Extraintestinal manifestations in inflammatory bowel disease-epidemiology, genetics, and pathogenesis. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 307–317.
- Mady, R.; Grover, W.; Butrus, S. Ocular complications of inflammatory bowel disease. Sci. World J. 2015, 2015, 438402.
- Vavricka, S.R.; Rogler, G.; Gantenbein, C.; Spoerri, M.; Prinz Vavricka, M.; Navarini, A.A.; French, L.E.; Safroneeva, E.; Fournier, N.; Straumann, A.; et al. Chronological Order of Appearance of Extraintestinal Manifestations Relative to the Time of IBD Diagnosis in the Swiss Inflammatory Bowel Disease Cohort. Inflamm. Bowel Dis. 2015, 21, 1794–1800.
- Durrani, O.M.; Tehrani, N.N.; Marr, J.E.; Moradi, P.; Stavrou, P.; Murray, P.I. Degree, duration, and causes of visual loss in uveitis. Br. J. Ophthalmol. 2004, 88, 1159–1162.
- Munoz-Fernandez, S.; Martin-Mola, E. Uveitis. Best Pract. Res. Clin. Rheumatol. 2006, 20, 487–505.
- Harbord, M.; Annese, V.; Vavricka, S.R.; Allez, M.; Barreiro-de Acosta, M.; Boberg, K.M.; Burisch, J.; De Vos, M.; De Vries, A.M.; Dick, A.D.; et al. The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease. J. Crohns. Colitis. 2016, 10, 239–254.
- Colia, R.; Corrado, A.; Cantatore, F.P. Rheumatologic and extraintestinal manifestations of inflammatory bowel diseases. Ann. Med. 2016, 48, 577–585.
- Katsanos, A.; Asproudis, I.; Katsanos, K.H.; Dastiridou, A.I.; Aspiotis, M.; Tsianos, E.V. Orbital and optic nerve complications of inflammatory bowel disease. J. Crohns. Colitis. 2013, 7, 683–693.
- Bandyopadhyay, D.; Bandyopadhyay, S.; Ghosh, P.; De, A.; Bhattacharya, A.; Dhali, G.K.; Das, K. Extraintestinal manifestations in inflammatory bowel disease: Prevalence and predictors in Indian patients. Indian J. Gastroenterol. 2015, 34, 387–394.
- Lanna, C.C.; Ferrari Mde, L.; Rocha, S.L.; Nascimento, E.; De Carvalho, M.A.; Da Cunha, A.S. A cross-sectional study of 130 Brazilian patients with Crohn’s disease and ulcerative colitis: Analysis of articular and ophthalmologic manifestations. Clin. Rheumatol. 2008, 27, 503–509.
- Ananthakrishnan, A.N. Environmental risk factors for inflammatory bowel disease. Gastroenterol. Hepatol. 2013, 9, 367–374.
This entry is offline, you can click here to edit this entry!
