3.1. T Cells
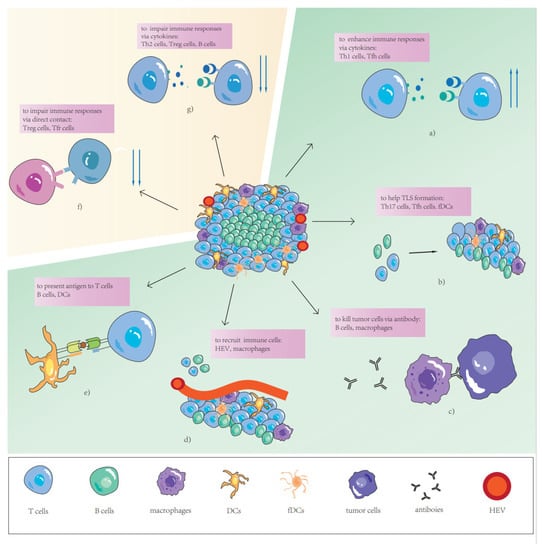
Naïve CD3+T cells recruited by TLSs become activated, proliferate, and differentiate based on the local tumor antigen presentation, cytokine milieu, and expression of costimulatory molecules, to result in several subsets of effector CD4+ T helper cells (Th), effector CD8+ T cytotoxic cells (CTL), and a small amount of memory T cells (Tm). The subtypes of Th cells can activate anti-tumor immunity directly or stimulate T cytotoxic cells to activate anti-tumor immunity, and some specific species can also inhibit immune cells from activity. Resembling SLOs, different subtypes of Th cells and their secreting cytokines, as well as chemokines, have mutual inhibition competition in TLSs. According to digital spatial-profiling data, T cells in tumors without TLSs had a dysfunctional molecular phenotype, which suggests that TLSs play a key role in the immune microenvironment by conferring distinct T cell phenotypes [
15].
CD4+Th-1 cells are characterized by T-bet and production of IL-2, interferon γ (IFNγ), and so on. IFN-γ is a pleiotropic cytokine that plays an important role in anti-tumor immunity by directly mediating tumor rejection and recruiting and activating innate and adaptive immune cells in TME. IL-2, which promotes T cell proliferation and maintains its functional activity, has been used in patients with metastatic melanoma and kidney cancer. The production of these cytokines by Th-1 cells is crucial to anti-tumor immunity mediated by CD8+ T cells. However, interestingly, a previous study showed that high infiltration in Th-1 cells and high numbers of CD20+ B-cell follicles–both of them usually aggregating with structures considered as TLSs–were associated with better relapse-free survival in gastric cancer [
51]. The densities of Th-1 cells and T follicular helper cells (Tfh) are both reported to be positively correlated with overall survival (OS) in nasopharyngeal carcinoma [
52], and the latter are vital to B cells during germinal center (GC)-reactions in SLO [
53]. This means that TLSs may exert an anti-tumor immune function through allowing T cell and B cell coordination. Although there is increasing evidence confirming the importance of humoral immunity in TLSs, a high ratio of Th-2 cells in TLSs, which are regarded as promoters of humoral immunity, was identified as a remarkably independent risk factor for recurrence in CRC, and the ratio increased in metastatic tumors in previous studies [
50]. Although direct evidence that Th-2 cells can suppress anti-tumor immunity and promote tumor progression is lacking for TLSs, findings regarding the TME suggest that Th2 cells can produce IL-4 and IL-13, with the former increasing the expression of epidermal growth factor to enhance neoplastic extravasating into the circulation, and the latter inhibiting the CD8+ cytotoxic T cell (CTL) response indirectly by increasing TGF-β production by myeloid cells in the tumor [
54,
55].
3.2. B Cells
B cells are mostly located in the germinal centers of TLSs in human cancers. They are characterized by different markers depending on their maturation degree such as CD19, CD20, and CD21. B cells and plasma cells (mature B cells) make up the germinal centers in TLSs and are considered one of alternative markers of TLSs. In the beginning of the era of immune therapy, B cells were reported to potentially favor tumor occurrence, progression, and spread [
72]. In a variety of mouse models, complement and antibodies produced by plasma cells were found to contribute to chronic inflammation [
73], and immune complexes might activate macrophages to produce vascular endothelial growth factors that could increase angiogenesis [
74]. In addition, B cells were considered to be able to produce suppressive cytokines such as IL-10, inhibiting T cell responses [
75]. With the development of tumor immunity, increasing research has suggested that an abundance of B cells, especially in TLSs, has been positively correlated with prognosis and the efficacy of immune therapy in human cancers in recent years [
76,
77,
78,
79,
80]. Although the true mechanisms by which B cells in TLSs enhance or directly develop anti-tumor immune responses still need to be explored, we can learn from how B cells influence immunity in SLOs. Just like in SLOs, B cells can recognize neoantigens via B cell receptors and then allow antigen binding with major histocompatibility complex-1 (MHC-1) or major histocompatibility complex-2 (MHC-2), then the presentation to T cells directly or to dendritic cells (DC) to activate T cells in TLSs [
81,
82,
83]. This method of antigen presentation is very effective in eliciting a T cell response with a low tumor mutation load and amplifying an immune response with high tumor mutation load [
72] because B cells may make contact with tumor cells at a very close distance, and immune complexes formed by combination of antibodies and neoantigens can be internalized by DCs. This means that the quantity of antigens necessary to induce a T cell response is much lower than direct antigen presentation by DCs. In addition, they are able to produce antibodies that can recognize shared tumor antigens, not patients’ specific tumor antigens that are almost recognized by T cells [
84]. Tumor cells are damaged by these antibodies through antibody-dependent cell-mediated cytotoxicity (ADCC) and/or antibody-dependent cell-mediated phagocytosis (ADCP). These reactions are mediated by fragment crystallizable (Fc) portions of tumor-specific antibody binding to Fc receptors of effector cells or complements. Similarly, there are differences between B cells with different functional markers in prognosis, such as OS being longer for TLSs with low fractions of CD21+ B cells, and shorter for those with a low activation-induced deaminase (AID)+ fraction of B cells [
85]. B cells will gradually decrease the expression of CD21 and increase the expression of AID in their mature process and migrate to the GCs. AID supports immune system diversification and acts in antigen-stimulated B cells by allowing antigen-driven immune globulin diversification. When AID is activated with appropriate cytokine signals in the B cells, interaction can occur with DCs and Tfr cells in GCs [
86]. Many studies have indicated that B cells play a direct or indirect important immune role in TLSs. However, a previous study on hepatocellular carcinoma showed that B cell-rich TLSs constitute a specific niche by which to protect tumor progenitors and produce lymphotoxin β to support the growth of tumor cells [
87].
3.3. Dendritic Cells
Dendritic cells (DCs) are a diverse group of professional antigen-presenting cells, with key roles in the initiation and regulation of innate and adaptive immune responses [
88]. DCs are crucial to TLS formation [
89] and maintenance, which has been validated in mouse models [
90]. LAMP+ DCs (mature DCs) are considered to be believable markers of TLSs in non-small-cell lung cancer (NSCLC), because they are almost exclusively found in these structures in this cancer type [
18]. However, some research on other cancers has shown that LAMP+DC was detected in non-TLS tumor lesions [
80,
91,
92]. Another previous study suggested that the LAMP+DC density was correlated with favorable clinical outcomes (overall, disease-specific, and disease-free survival) and the TIL density (in particular, Th-1 cells) was significantly decreased in tumors poorly infiltrated by LAMP+DCs [
45]. LAMP+DCs are also strongly correlated with Th-1 cells and immune cytotoxicity signals, and are positively associated with OS, because they can support TLSs to participate in promoting protective immunity in NSCLC. Another major subtype of follicular dendritic cells is discussed later.
3.4. High Endothelial Venules
Tumor-associated HEVs characterized by MECA-79 and peripheral node addressin (PNAd) are frequently found in TLSs and have been proposed to play important roles in lymphocyte entry into tumors, which is a process essential for successful antitumor immunity [
93]. In a murine model of colon carcinoma, HEVs were observed to control the formation of TLSs via production of IL-36γ [
94]. Numerous studies have shown that the density of HEVs is strongly correlated to the density of TLSs and is a positive predictor in many cancer types [
27,
94,
95,
96].
3.5. TLS-Associated Immune Cells
Immune fibroblasts are considered necessary for the early phase of TLS formation via building a network whose expansion is mediated by IL-22 and lymphotoxin α1β2 (LTα1β2) to support TLSs [
97,
98]. Some studies have shown that TLSs are not promoted by chronic inflammatory conditions in all organs because immune-associated fibroblasts are necessary and indispensable [
99,
100]. In a mouse model of TLSs, the subcutaneous injection of immune fibroblasts successfully induced TLSs that attracted the infiltration of host immune-cell subsets [
17]. Follicular dendritic cells (FDCs) are a specialized type of DC and are detected in the germinal center via labeling CD21, serving as immune-associated fibroblasts [
101]. FDCs form a dense three-dimensional follicular network, which lays a foundation for the generation of TLSs. In addition to antigen presentation and providing structural support, FDCs are able to modulate B cell diversity and enhance B memory cell differentiation in GCs [
102,
103]. The abundance of FDCs has been positively associated with the density of TLSs, suggesting better prognosis [
11].
Macrophages are characterized by the expression of CD68 and multiple functions. A previous study suggested that macrophages could secrete IL-36γ to control TLS formation [
94] and were responsible for recruiting CD4+ T cells and B cells to promote the formation of TLSs as antigen presentation cells [
104]. Additionally, macrophages are one of the main types of effector cells of ADCC and ADCP, which are primary anti-tumor mechanisms of humoral immunity in solid tumors. However, following ADCP, macrophages may up-regulate PD-L1 and indoleamine 2,3-dioxygenase to support local immunosuppression [
105]. In addition, a previous study on soft tissue sarcomas showed that macrophage colony-stimulating factor-1 receptor (CSF1R) responses were more frequent in TLSs compared with tumor tissue without TLSs. CSF1R is a marker of immunosuppressive macrophages, which are believed to maintain an anti-inflammatory niche for malignant cell growth [
106].