Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Oncology
Curcumin (diferuloylmethane)—the “golden spice”—has been widely studied because of its pleiotropic effects in cancer. Curcumin, a hydrophobic polyphenol, is derived from the rhizome of the herb Curcuma longa and constitutes the major curcuminoid in the spice turmeric (77% curcumin, 17% demethoxycurcumin, 3% bis-demethoxycurcumin). Curcumin is “generally recognized as safe” (GRAS) as a dietary supplement by the U.S Food and Drug Administration (FDA) and the European Food Safety Authority (EFSA) and has been catalogued with the E100 code of the European Union.
- curcumin
- metastatic colorectal cancer
- chemotherapy
1. Curcumin Attenuates Chemotherapy-Related Toxicity
For many years, curcumin (diferuloylmethane)—the “golden spice”—has been widely studied because of its pleiotropic effects in cancer. Curcumin, a hydrophobic polyphenol, is derived from the rhizome of the herb Curcuma longa and constitutes the major curcuminoid in the spice turmeric (77% curcumin, 17% demethoxycurcumin, 3% bis-demethoxycurcumin). Curcumin is “generally recognized as safe” (GRAS) as a dietary supplement by the U.S Food and Drug Administration (FDA) and the European Food Safety Authority (EFSA) and has been catalogued with the E100 code of the European Union. One of the clinical benefits of curcumin is the improvement of QoL in several health conditions [34], including cancer [35,36].
Curcumin is a pleiotropic agent that acts through multiple cellular pathways and has been shown to possess anti-cancer properties against CRC in vitro and in vivo [37,38]. Many of its anti-cancer properties have been attributed to its role as an anti-inflammatory and antioxidant, as well as to its ability to modulate the cell cycle and the pathways involved in proliferation, apoptosis, migration, invasion, angiogenesis, and metastasis [39], which are typically targeted by the drugs used to treat CRC. Mechanistically, curcumin modulates several CRC molecular targets at the same time—either by altering their gene expression, activation, or signaling pathways, or by direct interaction [37,38,39]. Importantly, in addition to its well-known anti-cancer properties, curcumin can also alleviate some of the chemotherapy-related side effects [40]. For example, curcumin attenuates the liver injury induced by oxaliplatin through activation of the nuclear factor-erythroid 2-related factor 2 (Nrf2) signaling, a key regulator pathway of cellular defense against oxidative and electrophilic stresses [41], as well as the nerve damage and the oxidative damage to mitochondria caused by oxaliplatin [42]. In fact, curcumin has been shown to not only hinder mitochondrial damage but also to protect mitochondria and induce activity of mitochondrial complex enzymes [36,42,43]. Interestingly, similar effects of curcumin on cisplatin-related toxicity have been observed in several tumor types [44,45,46,47,48]. Additionally, curcumin protects against irinotecan-induced intestinal injury by inhibiting nuclear factor kappa B (NF-κB) transcription factor activation [49], and it is also active against FOLFIRI-related cardiovascular toxicity [50] and capecitabine-induced hand-foot syndrome [51]. Recently, it has been shown that curcumin attenuates bevacizumab-associated cardiotoxicity by suppressing oxidative stress and preventing mitochondrial dysfunction in heart mitochondria [52].
In a study of curcumin’s effects in cancer patients, Belcaro and colleagues looked at the side effects of chemotherapy in several tumor types, including colon, ovarian, lung, liver, kidney, and stomach cancers. Of 80 patients treated with chemotherapy, 40 simultaneously received 500 mg of curcumin. Chemotherapy-related nausea, diarrhea, constipation, weight loss, neutropenia, and cardiotoxicity were significantly lower in the patients receiving curcumin than in the control group. Moreover, patients receiving curcumin also required fewer medications for treating these side effects [53]. In the same vein, turmeric supplementation for 21 days resulted in a clinically relevant and statistically significant improvement in global health status, symptom scores (fatigue, nausea, vomiting, pain, appetite loss, insomnia), and hematological parameters of breast cancer patients treated with paclitaxel [54]. Taken together, these findings lead us to suggest that the addition of curcumin to the standard treatment of CRC could not only attenuate chemotherapy-associated side effects but also improve the QoL of patients (Figure 1).
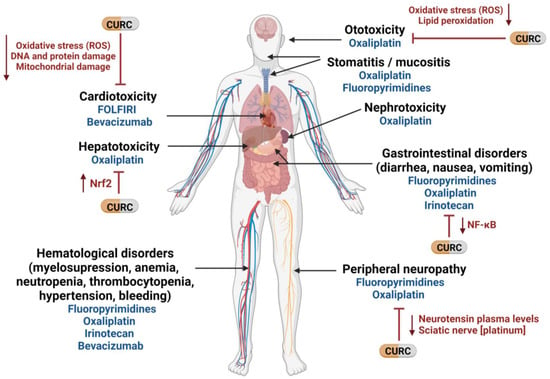
Figure 1. Potential use of curcumin to mitigate therapy-related side effects in mCRC. CURC: curcumin; NF-κB: nuclear factor kappa B; Nrf2: nuclear factor -erythroid 2- related factor 2; ROS: reactive oxygen species. Created with BioRender.com (accessed on 16 September 2022).
2. Curcumin Reverts Chemotherapy Resistance in mCRC
In addition to chemotherapy-related toxicity, chemoresistance remains one of the main problems hindering treatment success. Tumor cells can be intrinsically resistant or acquire resistance during a treatment. Resistance to chemotherapy is a complex and multifactorial process involving several mechanisms, including drug influx/efflux modifications, alterations in DNA damage repair (DDR), decreased cell death activation, autocrine survival signaling, and high detoxification activity [55,56]. One of these mechanisms with consequences in mCRC is the hyperactivation of the NF-κB signaling pathway [57], which promotes the expression of several target genes involved in inflammation, cell proliferation, apoptosis, angiogenesis, invasion, metastasis, and chemoresistance [58,59]. In fact, most of the anti-inflammatory and anti-cancer properties of curcumin are believed to be due to its ability to inhibit NF-κB activation through interaction with the IκB kinase complex (IKK) by inhibiting the phosphorylation and degradation of IκBα, a NF-κB inhibitor, and thereby blocking the nuclear translocation of this transcription factor [37,60,61]. Along with other studies [62,63,64], our group has demonstrated that curcumin can overcome oxaliplatin resistance by inhibiting the activity of the CXC-chemokines/NF-κB axis and, consequently, the expression of genes involved in anti-apoptosis and proliferation [57]. Additionally, in CRC preclinical models, curcumin was shown to enhance the effect of 5-fluorouracil [65,66] and capecitabine [67] by inhibiting AKT and NF-κB activity, and consequently, NF-κB-regulated gene products. In the same vein, Pattel and colleagues reported that curcumin sensitizes CRC cells to FOLFOX by inhibiting EGFR family receptors and insulin-like growth factor-1 receptor (IGF-1R) [68,69,70], the overexpression of which has been related to chemoresistance in CRC [71,72].
Chemotherapy resistance is also related to the specific mechanism of action of the drug. An example of such a specific mechanism is gene amplification in TS in 5-fluorouracil treated patients [73] and upregulation of genes involved in DDR pathways, such as ERCC1 in oxaliplatin treated patients [74]. Interestingly, Rajitha and colleagues demonstrated that the inhibition of NF-κB translocation by curcumin or its analogs induces cell cycle arrest and downregulates TS in CRC cells [61]. Furthermore, curcumin was found to inhibit ERCC1 through its ability to modulate miR-409-3p, thereby overcoming oxaliplatin resistance in CRC cells [75].
Curcumin can also promote the activation of apoptotic pathways by increasing the generation of reactive oxygen species (ROS) [76]. In a recent work, Li and colleagues demonstrated that curcumin can reverse Nicotinamide N-methyltransferase-induced cell proliferation and 5-fluorouracil resistance through ROS generation and cell cycle arrest [77].
On the other hand, the drug-resistant phenotype is associated with the acquisition of mesenchymal features, and epithelial-to-mesenchymal transition (EMT) plays a key role in chemoresistance in CRC, mainly through the activation of the NF-κB and transforming growth factor β (TGF-β) pathways [78,79,80]. In fact, EMT was observed in chemotherapy-resistant CRC cell lines [57,81,82], while curcumin was able to revert this chemoresistance by downregulating EMT markers [83] through TGF-β/Smad2/3 signaling attenuation [84], by upregulating EMT suppressive miRNAs [85] or by downregulating the TET1-NKD2-WNT signaling pathway [86]. In addition, several studies have demonstrated that curcumin can sensitize colon cancer stem cells (CSC), a small subpopulation of cells within tumors capable of self-renewal, differentiation, and tumorigenicity [87], to 5-fluorouracil, FOLFOX and irinotecan, thereby preventing the emergence of chemoresistant CRC cells [70,88,89,90,91]. In this regard, a recent study has demonstrated that treatment of CRC organoids with a combination of amorphous curcumin (a compound with improved solubility and bioavailability) and oxaliplatin, 5-fluoroouracil, or irinotecan showed a synergistic activity through the inhibition of proliferation-related signals and CSC marker expression, in addition to arresting the ERK signaling pathway [92]. Along the same lines, Zheng and colleagues showed that low doses of curcumin promoted the sensitivity of CRC cells to 5-fluorouracil by downregulating phospho-ERK signaling [93].
Finally, several studies have shown that curcumin can increase the intracellular accumulation of oxaliplatin and 5-fluorouracil in CRC cells by downregulating the P-gp [75,94] and ATP-binding cassette transporter G2 (ABCG2) [70] drug-efflux transporters both at the mRNA and protein levels. Preclinical data have suggested that the expression of ATP-binding cassette (ABC) transporters, such as ABCC2 [95], ABCB4 [96], as well as the multidrug resistance protein 1 (MDR1, also known as P-glycoprotein or P-gp), which is encoded by ABCB1 [97,98], can confer resistance to chemotherapy. However, evidence that these transporters contribute to drug resistance in human tumors is sorely lacking [99] and the development of MDR1 as a therapeutic target has been unsuccessful [100]. It is important to highlight that although several studies have related the ABC transporters’ overexpression to platinum resistance [55,101,102], the association between oxaliplatin resistance and the MDR1 expression has shown unconvincing results. For instance, Ekblad and colleagues described an overexpression of this membrane transporter as a consequence of oxaliplatin resistance acquisition in vitro, although functional tests did not show any increase in ABCB1 transport activity in the oxaliplatin-resistant models compared with its parental cell lines [103]. Other studies have reported no association between these drug efflux pumps and the sensitivity to oxaliplatin in CRC clinical samples [104]. In the same vein, the ability of MDR1 to confer resistance to 5-fluorouracil and irinotecan has been demonstrated in different CRC cell lines transfected with this carrier. However, its clinical relevance in CRC refractoriness to antitumor chemotherapy remains to be established [105,106]. Taken together, these results highlight the necessity of further investigation into the role of MDR1 and curcumin in oxaliplatin and 5-fluorouracil resistance in CRC patients.
Most clinical data on curcumin come from early phase clinical trials, with results showing that oral curcumin can achieve efficacious levels in the colon with negligible distribution outside the gut [107,108]. Moreover, curcumin was shown to be safe in advanced CRC patients when administered for up to four months [109]. In addition, a study by James and colleagues found that curcumin at doses up to 2 gms daily was highly tolerable when added to a FOLFOX regimen in mCRC patients with liver metastases [110]. More recently, the same group performed a phase IIa randomized trial of first-line treatment for mCRC patients comparing FOLFOX +/−bevacizumab with the same regimen plus curcumin 2 gms/day (CUFOX) in mCRC patients. In the intention-to-treat population, patients in the CUFOX arm achieved longer overall survival (HR 0.34; p = 0.02) but there was no difference in progression-free survival (HR 0.57) [111].
In conclusion, a further improvement in outcomes for mCRC highly depends on identifying and targeting mechanisms of drug resistance. Taken together, these findings offer compelling evidence that combining curcumin with conventional chemotherapy may be effective in overcoming drug resistance in mCRC
This entry is adapted from the peer-reviewed paper 10.3390/ijms232214058
This entry is offline, you can click here to edit this entry!
