This entry presents an overview of the smart electro-clothing systems (SeCSs) targeted at health monitoring, sports benefits, fitness tracking, and social activities. Technical features of the available SeCSs, covering both textile and electronic components, are thoroughly discussed and their applications in the industry and research purposes are highlighted. In addition, it also presents the developments in the associated areas of wearable sensor systems and textile-based dry sensors. As became evident during the literature research, such a review on SeCSs covering all relevant issues has not been presented before. This entry will be particularly helpful for new generation researchers who are and will be investigating the design, development, function, and comforts of the sensor integrated clothing materials.
- smart garments
- e-textiles
- biosignals
- sensors
- dry electrode
- signal-to-noise ratio (SNR)
- Internet of Things (IoT)
- knitted fabrics
1. Introduction
The electrical, chemical, and mechanical activities that take place in the human body during any biological event, such as beating of the heart and contraction of muscles, produce different biomedical signals [[1]]. On the basis of the physiological origins of these biosignals, they can be grouped as bioelectrical, biomagnetic, biochemical, biomechanical, bioacoustics, bio-optical, and biothermal signals. They can be further classified based on their nature of existence, that is, permanent or induced biosignals [[2]]. Permanent signals exist at all times within the body and are generated without any artificial trigger, impact, or excitation from outside of the body, for example, electrocardiogram (ECG) signal. Induced biosignals are artificially triggered, excited, or induced and they exist roughly for the duration of the excitation, for example, electroretinogram (ERG). Sensors that can sense biosignals or biopotentials can be categorised as physical, electrical, or chemical depending on their specific applications [[1]]. Different kinds of specialised electrodes are used for capturing biosignals. These electrodes could be either non-invasive (placed on skin surface) or invasive (e.g., microelectrodes or wire electrodes). Adding electrodes and sensors onto textiles and garments is a non-evasive way of capturing and measuring biosignals.
2. Influence and application
Thanks to the advancement of technology in producing microelectromechanical systems (MEMSs), wearable electronics have become very common consumables on the market nowadays. Wrist-worn wearable devices (smart watches and fitness trackers) experienced a growth of 18% and 7% in the United Kindom during the period of 2016–2017 and 2017–2018, respectively [[3]]. With the advent of conductive threads, textile structures either woven or knitted from conductive yarns, and conductive print-inks including those from graphene, it is now possible to produce or integrate light-weight sensors onto textiles to monitor health, fitness, and performance in a non-clinical environment, in daily-life, and in sport-training conditions [[4][5][6][7]]. An overview of the recent developments in wearable sensors for remote health monitoring is presented by Majumder et al. [[8]], while the smart sensors and fusion systems for sports and biomedical applications are reviewed by Mendes Jr. et al. [[9]]. In some cases, smart sensors are worn directly on the body using belts, straps, and adhesives; and in some cases, they are integrated or pocketed within textiles. The concept of Wearable 2.0 [[10]] envisages a full integration of wearable electronics within clothing, as presented in the Figure 1. Traditionally, such systems are known as smart garments, e-textiles, and e-garments. In the literature, they have also been mentioned as the IoT (Internet of Things) smart garments system [[11]]. For the ease of understanding across all disciplines, we have referred to them as smart electro-clothing systems (SeCSs) in this review.
A good number of SeCSs have emerged onto the market. This paper reviews the state-of-the-art development in design, construction, functionality, and application of such systems. As far as is known, such a review on SeCSs covering these relevant issues has not been presented before. However, it is important for researchers and product developers to have a complete review of those before initiating new research and attempting new product development in this and associated fields.
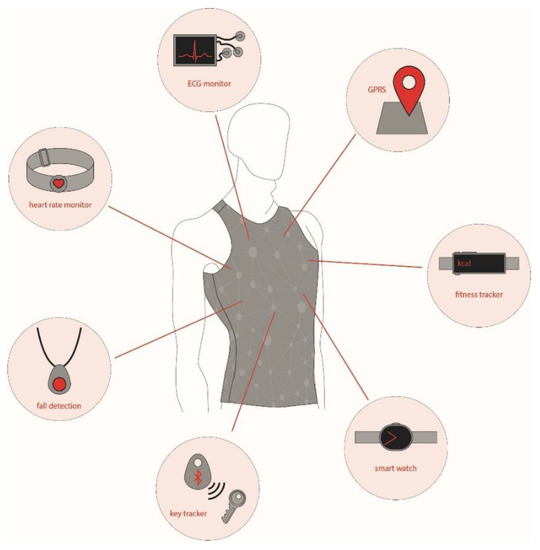
Figure 1. Concept of Wearable 2.0. ECG, electrocardiogram.
This entry is adapted from the peer-reviewed paper 10.3390/s20030587
References
- Enderle, J.; Blanchard, S.; Bronzinzo, J. Introduction to Biomedical Engineering; Elsevier Academic Press: Cambridge, MA, USA, 2005.
- Kanisusas, E. Fundamental of biosignals. In Biomedical Signals and Sensors, Linking Physiological Phenomena and Biosignals; Springer: Berlin, Germany, 2012; pp. 1–20
- Reynolds, A. Wearable Technology-UK-November 2018; Mintel: London, UK, 2018; Available online: http://academic.mintel.com.ezproxy.mmu.ac.uk/display/859763/ (accessed on 11 January 2019).
- Chen Zou; Yajie Qin; Chenglu Sun; Wei Li; Wei Chen; Motion artifact removal based on periodical property for ECG monitoring with wearable systems. Pervasive and Mobile Computing 2017, 40, 267-278, 10.1016/j.pmcj.2017.06.026.
- Takanori Ishikawa; Yasuhide Hyodo; Ken Miyashita; Kazunari Yoshifuji; Yota Komoriya; Yutaka Imai; Wearable Motion Tolerant PPG Sensor for Instant Heart Rate in Daily Activity. Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies 2017, , 126-133, 10.5220/0006109901260133.
- Juwon Lee; Jae-Hyun Nam; Design of Filter to Reject Motion Artifacts of PPG Signal by Using Two Photosensors. Journal of information and communication convergence engineering 2012, 10, 91-95, 10.6109/jicce.2012.10.1.091.
- Brendan Michael; Matthew Howard; Activity recognition with wearable sensors on loose clothing. PLOS ONE 2017, 12, e0184642, 10.1371/journal.pone.0184642.
- Sumit Majumder; Tapas K. Mondal; M. Jamal Deen; Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130, 10.3390/s17010130.
- José Mendes Jr.; Mário Elias Marinho Vieira; Marcelo Bissi Pires; Sergio Stevan Jr.; José Jair Alves Mendes; Sergio Luiz Stevan Jr.; Sensor Fusion and Smart Sensor in Sports and Biomedical Applications. Sensors 2016, 16, 1569, 10.3390/s16101569.
- Min Chen; Yujun Ma; Jeungeun Song; Chin-Feng Lai; Bin Hu; Smart Clothing: Connecting Human with Clouds and Big Data for Sustainable Health Monitoring. Mobile Networks and Applications 2016, 21, 825-845, 10.1007/s11036-016-0745-1.
- Tiago M. Fernandez-Carames; Paula Fraga-Lamas; Towards The Internet-of-Smart-Clothing: A Review on IoT Wearables and Garments for Creating Intelligent Connected E-Textiles. Electronics 2018, 7, 405, 10.3390/electronics7120405.
