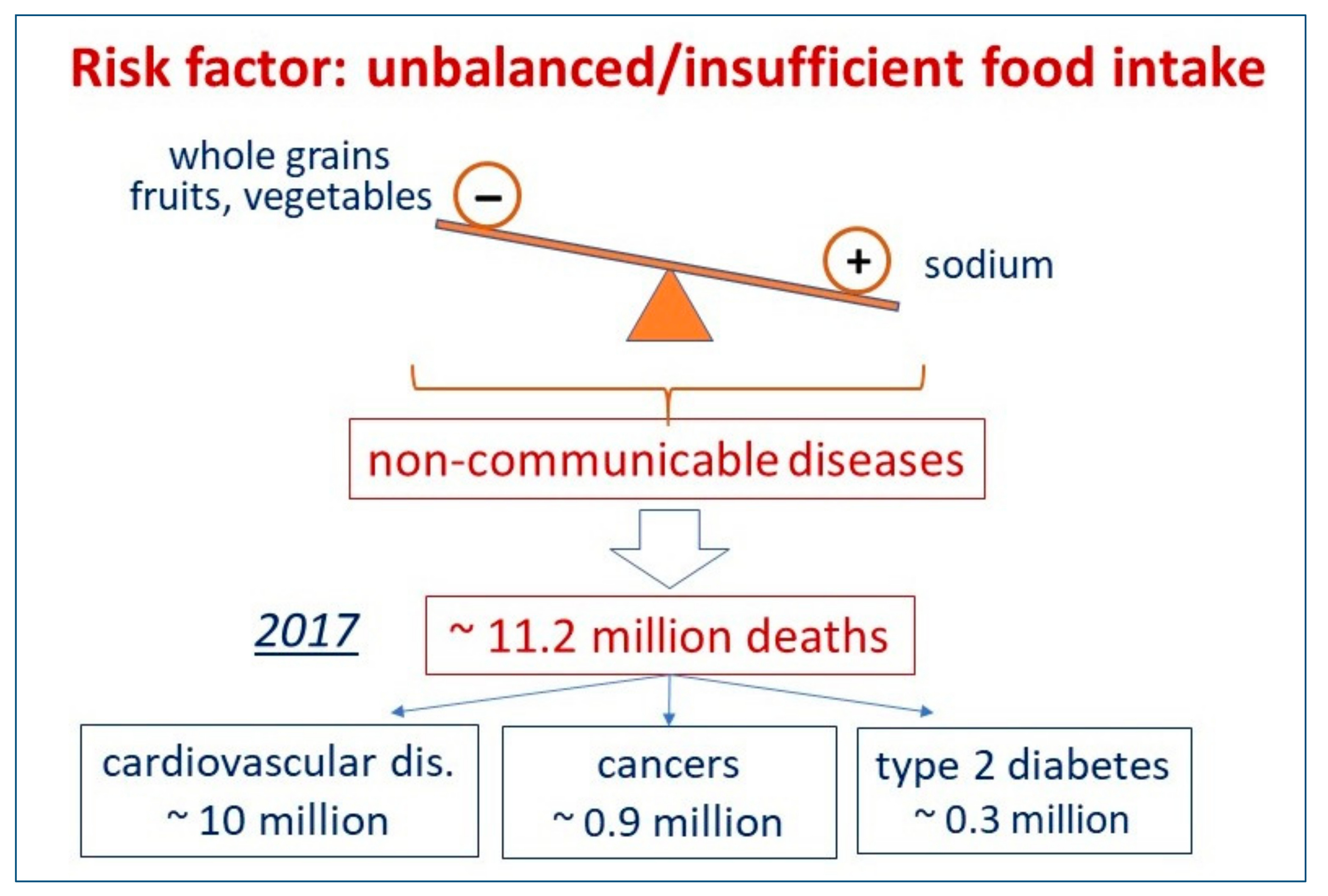
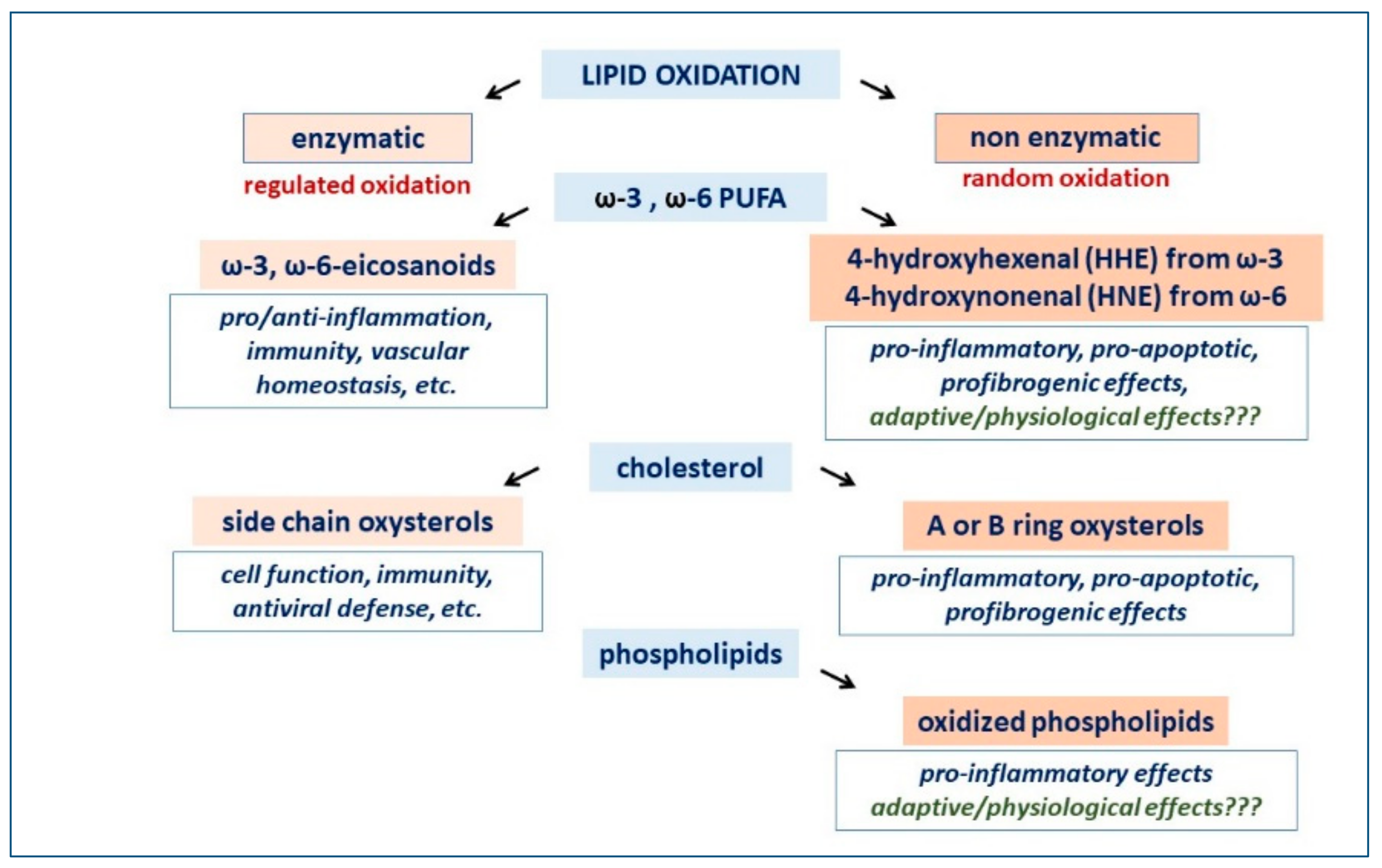
Dietary habits have major implications as causes of death globally, particularly in terms of cardiovascular disease, but to precisely define the role of the single components of diet in terms of cardiovascular risk is not an easy task. As an example, complex and multifactorial are the possible nutritional or detrimental effects of dietary fats, due to the huge variety of lipid metabolites originating from either the enzymatic or non-enzymatic oxidation of polyunsaturated fatty acids, cholesterol and phospholipids. The area of research that has allowed the benefit/risk profile of a dietary supplement to be tested with controlled studies is that of omega-3 fatty acids. Omega-3 fatty acids have showed a potential therapeutic role only in secondary cardiovascular prevention, while controlled studies in primary prevention have consistently produced neutral results.
- dietary fats
- fat oxidation
- nutritional research
1. Which Foods, or Food Shortages, Can Impact Mortality in Different AREAS of the World? What Kind of Non-Communicable Disease Can Be Impacted by Different Dietary Habits?
2. Is It True That the Consumption of Saturated Fat Has a Negative Impact on Cardiovascular Mortality?
3. We Are Confronted with More Doubts Than Certainties: How Reliable Is Nutritional Epidemiology Research?
4. From Uncertainties to Facts: What Are the Mechanisms Underlying the Metabolic Effects of Dietary Fats?
This entry is adapted from the peer-reviewed paper 10.3390/jcm11226652
References
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972.
- Astrup, A.; Magkos, F.; Bier, D.M.; Brenna, J.T.; De Oliveira Otto, M.C.; Hill, J.O.; King, J.C.; Mente, A.; Ordovas, J.M.; Volek, J.S.; et al. Saturated Fats and Health: A Reassessment and Proposal for Food-Based Recommendations: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 844–857.
- Mozaffarian, D.; Rosenberg, I.; Uauy, R. History of modern nutrition science-implications for current research, dietary guidelines, and food policy. BMJ 2018, 361, k2392.
- De Souza, R.; Mente, A.; Maroleanu, A.; Cozma, I.A.; Ha, V.; Kishibe, T.; Uleryk, E.; Budylowski, P.; Schünemann, H.; Beyene, J.; et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: Systematic review and meta-analysis of observational studies. BMJ 2015, 351, h3978.
- Harcombe, Z.; Baker, J.S.; Davies, B. Evidence from prospective cohort studies does not support current dietary fat guidelines: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1743–1749.
- Ramsden, C.E.; Zamora, D.; Majchrzak-Hong, S.; Faurot, K.; Broste, S.K.; Frantz, R.; Davis, J.M.; Ringel, A.; Suchindran, C.M.; Hibbeln, J.R. Re-evaluation of the traditional diet-heart hypothesis: Analysis of recovered data from Minnesota Coronary Experiment (1968-73). BMJ 2016, 353, i1246.
- Siri-Tarino, P.W.; Sun, Q.; Hu, F.B.; Krauss, R.M. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am. J. Clin. Nutr. 2010, 91, 535–546.
- Ioannidis, J.P.A. The Challenge of Reforming Nutritional Epidemiologic Research. JAMA 2018, 320, 969–970.
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Lampousi, A.-M.; Knüppel, S.; Iqbal, K.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of all-cause mortality: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2017, 105, 1462–1473.
- Poole, R.; Kennedy, O.J.; Roderick, P.; Fallowfield, J.A.; Hayes, P.C.; Parkes, J. Coffee consumption and health: Umbrella review of meta-analyses of multiple health outcomes. BMJ 2017, 359, j5024.
- Trepanowski, J.F.; Ioannidis, J.P.A. Perspective: Limiting Dependence on Nonrandomized Studies and Improving Randomized Trials in Human Nutrition Research: Why and How. Adv. Nutr. 2018, 9, 367–377.
- Ioannidis, J.P. Implausible results in human nutrition research. BMJ 2013, 347, f6698.
- Prasad, V.; Jorgenson, J.; Ioannidis, J.P.; Cifu, A. Observational studies often make clinical practice recommendations: An empirical evaluation of authors’ attitudes. J. Clin. Epidemiol. 2013, 66, 361–366.
- Endo, J.; Arita, M. Cardioprotective mechanism of omega-3 polyunsaturated fatty acids. J. Cardiol. 2016, 67, 22–27.
- Wang, H.; Li, Q.; Zhu, Y.; Zhang, X. Omega-3 Polyunsaturated Fatty Acids: Versatile Roles in Blood Pressure Regulation. Antioxid Redox Signal. 2021, 34, 800–810.
- Sottero, B.; Leonarduzzi, G.; Testa, G.; Gargiulo, S.; Poli, G.; Biasi, F. Lipid Oxidation Derived Aldehydes and Oxysterols Between Health and Disease. Eur. J. Lipid Sci. Technol. 2019, 121, 1700047.
- Gargiulo, S.; Testa, G.; Gamba, P.; Staurenghi, E.; Poli, G.; Leonarduzzi, G. Oxysterols and 4-hydroxy-2-nonenal contribute to atherosclerotic plaque destabilization. Free Radic. Biol. Med. 2017, 111, 140–150.
