Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Trauma injuries are an important healthcare problem and one of the main leading causes of death worldwide. Researchers analyzed current practices in teaching trauma management using simulations, with the aim of summarizing them, identifying gaps and providing a critical overview on what has already been achieved.
- education
- clinical simulation
- trauma management
1. Introduction
Trauma injuries are responsible for 9% of global mortality and are considered a risk all around the globe. These injuries result from traffic collisions, drowning, poisoning, falls or burns and violence, causing more than five million deaths worldwide annually [1]. Moreover, a large number of those injuries cause temporary or permanent disabilities, incurring important consequences on the patients’ lives. Therefore, a fast identification and management of trauma injuries is of great importance. To do that, a systematic and rapid approach should be applied [2].
The Advanced Trauma Life Support (ATLS) course was created in 1978 by the American College of Surgeons, and it is currently taught in over 60 countries [3]. This course has used a variety of simulation modalities to teach trauma management and, since then, other trauma management courses have arisen [4][5][6][7]. Additionally, regarding pre-hospital trauma management, the two courses mainly referenced being the Pre-Hospital Trauma Life Support (PHTLS) course [8][9][10] and the International Trauma Life Support (ITLS) course [11][12], which focus on education for first responders and also use simulations, as well as classroom sessions. Trauma training focuses on several aspects that can be classified into technical skills and non-technical skills. Technical skills refer to the application of a correct triage, primary and secondary surveys, including the techniques and treatments needed to achieve that. Non-technical skills focus on communication, leadership, management of situations and decision making. Even though both types of skills are intrinsically related, some training focuses only on technical skills, others in non-technical skills and others on both.
In this context, it is important to highlight the role of clinical simulations. Clinical simulations started to support clinical training by taking into account patient safety [13][14][15][16], but it also offers some other benefits, such as the opportunity to repeat a simulation as many times as needed, or to train a great variety of technical and non-technical skills [17][18][19][20]. Nevertheless, there is still limited evidence on the impact of simulation-based training on the performance in trauma management [14][16] and on the long-term knowledge retention of such training [16][21]. Clinical simulators are classified according to the concept of fidelity, with the simulated model’s relation to its closeness to reality being the main classification: low-, medium- and high-fidelity simulators. Low-fidelity simulators are anatomical representations of a part of the body to train simple tasks and to acquire basic motor skills to be able to develop those tasks. It is generally composed of low technology. Medium-fidelity simulators integrate low-complexity software programs that allow manipulating physiological variables to assess knowledge during decision making in environments such as cardiopulmonary resuscitation. Finally, high-fidelity simulators are life-size mannequins that integrate mechanical devices and computer technology to train advanced techniques and skills in handling critical situations. In principle, high-fidelity simulations are the best option; however, according to [22][23][24], there is no important difference with respect to knowledge and skill improvements of high-fidelity compared to low-fidelity simulators. In [22], the skill performance evolution comparing low-fidelity and high-fidelity simulations is studied in a systematic review. This study shows that, in the short-term, the use of high-fidelity simulators provides a moderate benefit compared to low-fidelity; however, in the long term, no benefits are obtained. Additionally, in [23], a study in simulated neonatal resuscitations is presented. It shows no differences after training with a low-fidelity or a high-fidelity simulator. Finally, a randomized control trial with more than 100 undergraduate students was conducted using low- and a high-fidelity simulators [24]. The conclusion was that the improvement obtained was similar after both training courses.
Therefore, a review has been accomplished to analyze the current practice in teaching trauma management using simulations with the aim of summarizing them, identifying gaps and providing a critical overview on what has been achieved in terms of trauma training.
2. Clinical Practice of Trauma Management Training
A search was performed on the Web of Science website. The initial search provided 1617 publications including on this review, finally, 35 articles. These articles focused on trauma training and provided studies on how different simulation training techniques could impact trauma management training. The article selection process is shown in Figure 1.
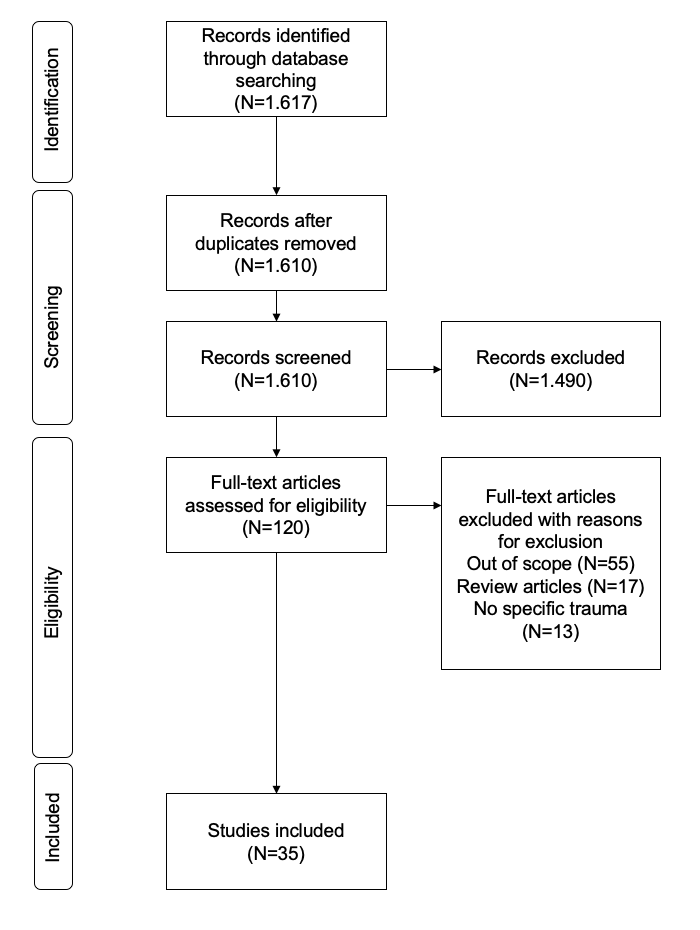
Figure 1. PRISMA flow diagram showing the study selection process.
The main topics analyzed are: the target audience of the trauma trainings, the simulation methods used, the types of skills acquired after the training, the evaluation methods used and the context in which the simulations take place. To analyze all the articles, the following information was gathered: authors, publication type, year of publication, total number of citations, population of training, simulation method used, skills trained, evaluation type used for the simulation method presented in the paper, if skills improved after the training and the context in which the simulation took place. The main takeaways are summarized below.
Taking a look at the results obtained for the target audience of the trauma trainings, it stood out that there was scarcity in trauma management training courses for medical students. Moreover, according to [16][25], the best simulation method and procedure to teach trauma management to medical students have not yet been established. This is a field that needs further development, as medical students should be trained on trauma management skills considering that they are soon-to-be residents. As residents, they are going to be the first attendants in the hospital; therefore, having specific trauma training would allow for better treatments for patients [20][26][27]. Additionally, trauma training supports clinical reasoning learning. This is key for clinical practice, and could be obtained with trauma management training [28].
According to Lewis C. and Veal B. [21], none of the 29 articles included in the review could demonstrate a significant objective impact on the mortality and morbidity of trauma patients; therefore, there is still more research needed in this field. Nonetheless, there are studies [26][29][30] that support and present statistical improvements in trauma management performance after simulation training. They confirm that, if the correct simulation modality is used, the expected outcome of the patient could be more easily predicted [2]. Therefore, it is important to know the different simulation modalities and how they should be implemented within trauma management training. In [2], it was stated that trauma training uses both low- and high-fidelity training modalities. Low-fidelity training allows to reproduce and practice technical skills such as airway management, whereas high-fidelity training offers the possibility to train both technical and non-technical skills. Additionally, standardized patients could also be used to train non-technical skills and, if properly garbed with the appropriate modules, some technical skills could also be practiced. Moreover, virtual reality is currently increasing its presence, as it allows to connect multiple users at multiple locations, increasing availability to centers with limited resources. This simulation modality offers the possibility to immerse learners within authentic clinical scenarios at a low cost.
With respect to the simulation methods used, traditional simulation methods try to imitate real patient simulations. That is the reason why high-fidelity mannequins or actors have been widely used [31][32]. Nevertheless, technology allows for the development of other simulation methods that could offer solutions to the limitations that actors and mannequins have. Simulations with actors have limitations, as some techniques cannot be applied. High-fidelity mannequins are expensive models that require specific technical requirements and resources. Virtual reality offers a solution to these limitations, as it allows trainees to immerse themselves in the situation, enabling them to accomplish different trauma scenarios without compromising the patient and allowing institutions to train a large number of trainees [28][33][34][35]. However, each simulation method has its advantages and disadvantages and, therefore, a further reflection is needed with respect to the selection of simulation method, as stated in [2][16]. It is also important to consider, for the selection of the simulation method, which skills to train.
Taking into account the results obtained for the skills trained, there was still a majority of simulation-based training courses that focused on technical skills. The goal of these training courses is to teach complex and specific skills [36]. Moreover, the number of training courses that consider non-technical skills is increasing [37][38][39]. That is the reason why the number of simulation-based training courses that consider both types of skills is also higher. It is important to highlight that the articles included focused on individual training. Therefore, it makes sense that more articles focused on training technical skills. The training courses that focus on non-technical skills prefer training in groups or teams, as this allows to practice those skills. Consequently, and as previously highlighted, depending on the skills to train, one simulation method can be better than another.
According to [15], medical training courses that use simulations should be adapted to the level and the type of education. Therefore, this article considered undergraduate teaching, postgraduate teaching, continuing medical education, disaster management and military trauma management. Furthermore, according to [2], the training courses should focus on the types of skills to train. Therefore, this article proposed to classify training courses into either task-oriented or non-technical-skill-oriented training, independently on the individual level and type of education of the trainee. The main idea behind these studies is identifying the focus of the training and then trying to find a simulation method that fits better with that focus, independent of the name provided to the focus of the training. It is clear that the trend is to incorporate non-technical skills within training courses in order to create a comprehensive trauma program; therefore, this trend is generally perceived in trauma training. Consequently, high-fidelity mannequins seem to be the best option; however, incorporating virtual reality together with low-fidelity mannequins could be another alternative with some advantages, such as the cost of the chosen simulation method used. For trauma training, as technical and non-technical skills need to be trained, simulation methods that combine low-, medium- and high-fidelity training should be considered.
Regarding the evaluation methods currently used in simulation-based training courses, only two of them considered the option of having an automated evaluation method [40][41]; however, either this was only partially considered, or the details on how automation was achieved were not explained. Therefore, the majority of the training courses analyzed did not offer an automated evaluation method, showing an important gap. It is true that there is an important discussion about how the evaluation of simulation-based training must be conducted [18][20][28][31][41][42][43][44][45], but it is surprising that the majority of the articles did not even consider the option to include an automated option. Additionally, this was unforeseen, as the advantage of having high-fidelity mannequins or other simulation methods is that they allow for the possibility to gather objective information directly from them. That information would be extremely valuable, as it is entirely objective, which fits with the purpose of using the simulations to provide a more objective evaluation method [46][47]. Additionally, the objective information gathered with the simulation methods has a positive impact on trainees, as it provides high-quality feedback, which allows them to see the impact of their actions during the simulation. This supports skill learning and performance [48][49][50]. As the majority of the trainings did not use an automated evaluation method, an analysis on which methods were used was performed. Many of the training courses used written evaluation forms or checklists. They were specifically developed for the trauma training provided, as stated in [18][31][51][52][53]. This allowed for the evaluation process to be more objective, though not entirely, as the trainees’ answers to the questionnaires or checklists comprised their opinions on how the simulations occurred. That opinion is valid and necessary after a simulation-based training; however, evaluating the performance of the training only with this information should not be the case. Just four of the training courses used purely subjective evaluation methods that consisted of either personal interviews, written comments or evaluations conducted through direct observations. Finally, most of the articles analyzed focused on training either technical or non-technical skills for traumas that took place in a hospital environment; however, the presence of pre-hospital training is increasing [17]. This situation highlights the importance of training all professionals involved in trauma scenarios in any of the environments in which the patient could be located, considering that the resources.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph192013546
References
- World Health Organization. Injuries. 2021. Available online: https://platform.who.int/mortality/themes/theme-details/mdb/injuries (accessed on 2 June 2021).
- Quick, J.A. Simulation Training in Trauma. Mo. Med. 2018, 115, 447–450.
- Carmont, M.R. The Advanced Trauma Life Support course: A history of its development and review of related literature. Postgrad. Med. J. 2005, 81, 87–91.
- Gambhir, R.; Agrawal, A. Training in Trauma Management. Med. J. Armed Forces India 2010, 66, 354–356.
- Lin, H.-L.; Chen, C.-W.; Lee, W.-C.; Kuo, L.-C.; Cheng, Y.-C.; Lin, Y.-K.; Lin, J.-N.; Chan, H.-M. Effects of the Emergency Trauma Training Course on the Confidence of Final-Year Medical Students Dealing with Trauma Patients. Kaohsiung J. Med. Sci. 2009, 25, 10–15.
- Shukla, A.; Kline, D.; Cherian, A.; Lescanec, A.; Rochman, A.; Plautz, C.; Kirk, M.; Littlewood, K.E.; Custalow, C.; Srinivasan, R.; et al. A Simulation Course on Lifesaving Techniques for Third-Year Medical Students. Simul. Healthc. J. Soc. Simul. Healthc. 2007, 2, 11–15.
- Ashcroft, J.; Wilkinson, A.; Khan, M. A Systematic Review of Trauma Crew Resource Management Training: What Can the United States and the United Kingdom Learn From Each Other? J. Surg. Educ. 2021, 78, 245–264.
- Mobrad, A.; Al Najjar, A.; Abu Zeid, R.; Atta Aldayes, A. Evaluating the effect of the prehospital trauma life support (PHTLS) course on emergency medical services students’ knowledge. Biomed. Res. 2020, 31, 31–36.
- Häske, D.; Beckers, S.K.; Hofmann, M.; Lefering, R.; Gliwitzky, B.; Wölfl, C.C.; Grützner, P.; Stöckle, U.; Dieroff, M.; Münzberg, M. Quality of Documentation as a Surrogate Marker for Awareness and Training Effectiveness of PHTLS-Courses. Part of the Prospective Longitudinal Mixed-Methods EPPTC-Trial. PLoS ONE 2017, 12, e0170004.
- Ali, J.; Adam, R.; Josa, D.; Pierre, I.; Bedsaysie, H.; West, U.; Winn, J.; Ali, E.; Haynes, B. Effect of basic prehospital trauma life support program on cognitive and trauma management skills. World J. Surg. 1998, 22, 1192–1196.
- Requena, A.; Jimnez, L.; Gmez, R.; del Arco, C. International Trauma Life Support (ITLS) training through the Spanish Society of Emergency Medicine (SEMES): 10 years’ experience with the SEMES-ITLS program. Emergencias 2015, 27, 62–65.
- International Trauma Life Support (ITLS); Campbell, J. International Trauma Life Support for Emergency Care Providers; Pearson Education: Harlow, UK, 2013.
- Hammond, J. Simulation in critical care and trauma education and training. Curr. Opin. Crit. Care 2004, 10, 325–329.
- Aggarwal, R.; Mytton, O.; Derbrew, M.; Hananel, D.; Heydenburg, M.; Issenberg, B.; Macaulay, C.; Mancini, M.E.; Morimoto, T.; Soper, N.; et al. Training and simulation for patient safety. Qual. Saf. Health Care 2010, 19 (Suppl. 2), i34–i43.
- Datta, R.; Upadhyay, K.; Jaideep, C. Simulation and its role in medical education. Med. J. Armed Forces India 2012, 68, 167–172.
- Borggreve, A.S.; Meijer, J.M.R.; Schreuder, H.W.R.; ten Cate, O. Simulation-based trauma education for medical students: A review of literature. Med. Teach. 2017, 39, 631–638.
- Abelsson, A.; Rystedt, I.; Suserud, B.-O.; Lindwall, L. Mapping the use of simulation in prehospital care—A literature review. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 22.
- Murray, D.J.; Freeman, B.D.; Boulet, J.R.; Woodhouse, J.; Fehr, J.J.; Klingensmith, M.E. Decision Making in Trauma Settings. Simul. Healthc. J. Soc. Simul. Healthc. 2015, 10, 139–145.
- Van Dillen, C.M.; Tice, M.R.; Patel, A.D.; Meurer, D.A.; Tyndall, J.A.; Elie, M.C.; Shuster, J.J. Trauma Simulation Training Increases Confidence Levels in Prehospital Personnel Performing Life-Saving Interventions in Trauma Patients. Emerg. Med. Int. 2016, 2016, 5437490.
- Cuisinier, A.; Schilte, C.; Declety, P.; Picard, J.; Berger, K.; Bouzat, P.; Falcon, D.; Bosson, J.L.; Payen, J.-F.; Albaladejo, P. A major trauma course based on posters, audio-guides and simulation improves the management skills of medical students: Evaluation via medical simulator. Anaesth. Crit. Care Pain Med. 2015, 34, 339–344.
- Lewis, C.; Veal, B. Patient Simulation as an Active Learning Tool in Medical Education. J. Med. Imaging Radiat. Sci. 2010, 41, 196–200.
- Cheng, A.; Lockey, A.; Bhanji, F.; Lin, Y.; Hunt, E.A.; Lang, E. The use of high-fidelity manikins for advanced life support training—A systematic review and meta-analysis. Resuscitation 2015, 93, 142–149.
- Finan, E.; Bismilla, Z.; Whyte, H.E.; Leblanc, V.; McNamara, P. High-fidelity simulator technology may not be superior to traditional low-fidelity equipment for neonatal resuscitation training. J. Perinatol. 2012, 32, 287–292.
- Nimbalkar, A.; Patel, D.; Kungwani, A.; Phatak, A.; Vasa, R.; Nimbalkar, S. Randomized control trial of high fidelity vs low fidelity simulation for training undergraduate students in neonatal resuscitation. BMC Res. Notes 2015, 8, 636.
- Jouda, M.; Finn, Y. Training in polytrauma management in medical curricula: A scoping review. Med. Teach. 2020, 42, 1385–1393.
- Cecilio-Fernandes, D.; Brando, C.; de Oliveira, D.; Fernandes, G.; Tio, R. Additional simulation training: Does it affect students’ knowledge acquisition and retention? BMJ Simul. Technol. Enhanc. Learn. 2018, 5, 140–143.
- Ruesseler, M.; Weinlich, M.; Müller, M.P.; Byhahn, C.; Marzi, I.; Walcher, F. Simulation training improves ability to manage medical emergencies. Emerg. Med. J. 2010, 27, 734–738.
- Fleiszer, D.; Hoover, M.L.; Posel, N.; Razek, T.; Bergman, S. Development and Validation of a Tool to Evaluate the Evolution of Clinical Reasoning in Trauma Using Virtual Patients. J. Surg. Educ. 2018, 75, 779–786.
- Alsaad, A.A.; Davuluri, S.; Bhide, V.Y.; Lannen, A.M.; Maniaci, M.J. Assessing the performance and satisfaction of medical residents utilizing standardized patient versus mannequin-simulated training. Adv. Med. Educ. Pract. 2017, 8, 481–486.
- Barleycorn, D.; Lee, G.A. How effective is trauma simulation as an educational process for healthcare providers within the trauma networks? A systematic review. Int. Emerg. Nurs. 2018, 40, 37–45.
- Knudson, M.M.; Khaw, L.; Bullard, M.K.; Dicker, R.; Cohen, M.J.; Staudenmayer, K.; Sadjadi, J.; Howard, S.; Gaba, D.; Krummel, T. Trauma Training in Simulation: Translating Skills From SIM Time to Real Time. J. Trauma Inj. Infect. Crit. Care 2008, 64, 255–264.
- Abelsson, A.; Rystedt, I.; Suserud, B.-O.; Lindwall, L. Learning by simulation in prehospital emergency care—An integrative literature review. Scand. J. Caring Sci. 2015, 30, 234–240.
- Patel, D.; Hawkins, J.; Chehab, L.Z.; Martin-Tuite, P.; Feler, J.; Tan, A.; Alpers, B.S.; Pink, S.; Wang, J.; Freise, J.; et al. Developing Virtual Reality Trauma Training Experiences Using 360-Degree Video: Tutorial. J. Med. Internet Res. 2020, 22, e22420.
- Taylor, D.; Patel, V.; Cohen, D.; Aggarwal, R.; Kerr, K.; Sevdalis, N.; Batrick, N.; Darzi, A. Single and Multi-User Virtual Patient Design in the Virtual World. Med. Meets Virtual Real. 18 2011, 163, 650–652.
- Cohen, D.; Sevdalis, N.; Taylor, D.; Kerr, K.; Heys, M.; Willett, K.; Batrick, N.; Darzi, A. Emergency preparedness in the 21st century: Training and preparation modules in virtual environments. Resuscitation 2013, 84, 78–84.
- Kuhlenschmidt, K.M.; Houshmand, N.; Bisgaard, E.; Grant, J.; Dumas, R.; Park, C.; Cripps, M.W. Simulation-Based Skill Training in Trauma: A Much Needed Confidence Boost. J. Am. Coll. Surg. 2020, 231, S256.
- Doumouras, A.G.; Engels, P.T. Early crisis nontechnical skill teaching in residency leads to long-term skill retention and improved performance during crises: A prospective, nonrandomized controlled study. Surgery 2017, 162, 174–181.
- Ziesmann, M.T.; Widder, S.; Park, J.; Kortbeek, J.B.; Brindley, P.; Hameed, M.; Paton-Gay, J.D.; Engels, P.T.; Hicks, C.; Fata, P.; et al. S.T.A.R.T.T.: Development of a national, multidisciplinary trauma crisis resource management curriculum-results from the pilot course. J. Trauma Acute Care Surg. 2013, 75, 753–758.
- Gillman, L.M.; Brindley, P.; Paton-Gay, J.D.; Engels, P.T.; Park, J.; Vergis, A.; Widder, S. Simulated Trauma and Resuscitation Team Training course—Evolution of a multidisciplinary trauma crisis resource management simulation course. Am. J. Surg. 2016, 212, 188–193.e3.
- Harrington, C.M.; Kavanagh, D.O.; Quinlan, J.F.; Ryan, D.; Dicker, P.; O’Keeffe, D.; Traynor, O.; Tierney, S. Development and evaluation of a trauma decision-making simulator in Oculus virtual reality. Am. J. Surg. 2018, 215, 42–47.
- Walker, R.; Phieffer, L.S.; Bishop, J.Y. Four Successive Years of Trauma-Based Objective Structured Clinical Evaluations: What Have We Learned? J. Surg. Educ. 2016, 73, 648–654.
- Fernandez, G.L.; Page, D.W.; Coe, N.P.; Lee, P.C.; Patterson, L.A.; Skylizard, L.; Louis, M.S.; Amaral, M.H.; Wait, R.B.; Seymour, N.E. Boot Camp: Educational Outcomes After 4 Successive Years of Preparatory Simulation-Based Training at Onset of Internship. J. Surg. Educ. 2012, 69, 242–248.
- Montán, K.L.; Hreckovski, B.; Dobson, B.; Örtenwall, P.; Montán, C.; Khorram-Manesh, A.; Lennquist, S. Development and evaluation of a new simulation model for interactive training of the medical response to major incidents and disasters. Eur. J. Trauma Emerg. Surg. 2013, 40, 429–443.
- Jawaid, M.; Memon, A.A.; Masood, Z.; Alam, S.N. Effectiveness of the Primary Trauma Care Course: Is the outcome satisfactory? Pak. J. Med. Sci. 2013, 29, 1265–1268.
- Figueroa, F.O.; Moftakhar, Y.; Iv, A.L.D.; Khan, R.; Dasgupta, R.; Blanda, R.; Marchand, T.; Ahmed, R. Trauma Boot Camp: A Simulation-Based Pilot Study. Cureus 2016, 8, e463.
- Ali, J.; Dunn, J.; Eason, M.; Drumm, J. Comparing the Standardized Live Trauma Patient and the Mechanical Simulator Models in the ATLS Initial Assessment Station. J. Surg. Res. 2010, 162, 7–10.
- Wallenstein, J.; Heron, S.; Santen, S.; Shayne, P.; Ander, D. A Core Competency-based Objective Structured Clinical Examination (OSCE) Can Predict Future Resident Performance. Acad. Emerg. Med. 2010, 17, S67–S71.
- Cohen, D.C.; Sevdalis, N.; Patel, V.; Taylor, D.; Batrick, N.; Darzi, A.W. Major Incident Preparation for Acute Hospitals: Current State-of-the-Art, Training Needs Analysis, and the Role of Novel Virtual Worlds Simulation Technologies. J. Emerg. Med. 2012, 43, 1029–1037.
- Dausey, D.J.; Buehler, J.W.; Lurie, N. Designing and conducting tabletop exercises to assess public health preparedness for manmade and naturally occurring biological threats. BMC Public Health 2007, 7, 92.
- Issenberg, S.B.; McGaghie, W.; Petrusa, E.R.; Gordon, D.L.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28.
- Amiel, I.; Simon, D.; Merin, O.; Ziv, A. Mobile in Situ Simulation as a Tool for Evaluation and Improvement of Trauma Treatment in the Emergency Department. J. Surg. Educ. 2016, 73, 121–128.
- Pringle, K.; Mackey, J.; Ruskis, J.; Modi, P.; Foggle, J.; Levine, A. A Short Trauma Course for Physicians in a Resource-Limited Setting: Is Low-Cost Simulation Effective? Ann. Emerg. Med. 2013, 62, S100.
- Springer, R.; Mah, J.; Shusdock, I.; Bräutigam, R.; Donahue, S.; Butler, K. Simulation Training in Critical Care: Does Practice Make Perfect? J. Surg. Res. 2013, 179, 229.
This entry is offline, you can click here to edit this entry!
