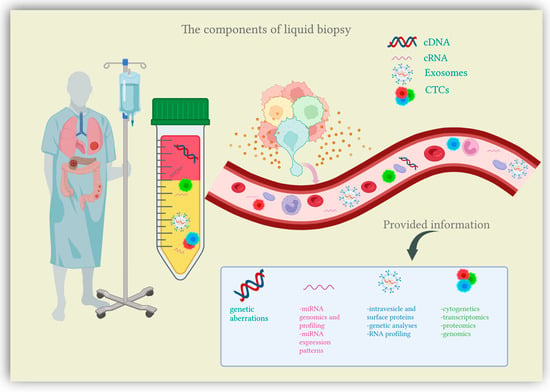
Recent research has been shedding light on a new diagnostic approach suited for cancer patients, the liquid biopsy. Liquid biopsy comes as a simple, minimally invasive diagnostic tool, attempting to overcome the limitations of conventional tissue biopsy by providing more comprehensive data on tumor heterogeneity and dynamics at different junctures in cancer development [
13]. Liquid biopsy refers to the biological fluids obtained from cancer patients and submitted to extensive analysis in order to isolate biomarkers indicative of malignancy. The liquid samples considered for testing can include any biological fluid (e.g., urine, pleural effusion, ascites, sputum, or cerebrospinal fluid), however, the main focus is peripheral blood [
14]. The main components of liquid biopsies are circulating tumor cells (CTCs), circulating nucleic acids (circulating tumor DNA and circulating microRNAs) and extracellular vesicles (exosomes and microvesicles) [
12,
15] (
Figure 1). Liquid biopsies allow a comprehensive analysis of plasma, also considered the somatic component of the blood, which can be manipulated for the isolation of CTCs, circulating nucleic acids and exosomes [
16]. Somatic mutations can be detected through a thorough examination of these plasma components, which are shed into the bloodstream directly from the primary tumor and distant metastasis, therefore offering an extensive characterization of the tumor mass [
17]. In this context, liquid biopsy analytes are currently finding their clinical application in the setting of CRC screening.
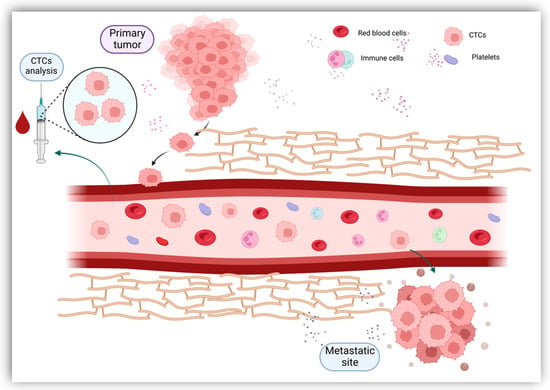
Originally described in 1869, CTCs are now gaining clinical importance in the management of patients with cancer [
18]. CTCs define cells derived from the primary tumor, metastases and recurrence sites that enter the circulatory system either as individual cells or as clusters [
19]. Tumor cells constitute these clusters alone or in association with fibroblasts, leukocytes, endothelial cells and platelets, forming tumor microemboli more resistant against the aggression of the host’s immune system [
20]. Once they have entered the bloodstream, CTCs bear the capacity to seed the disease to secondary sites, causing tumor metastases in distant organs and disease relapses [
19] (
Figure 2). Furthermore, CTCs have shown great plasticity through their ability to undergo epithelial-to-mesenchymal transition (EMT) [
21]. As most CTCs entering the bloodstream are exposed to mechanical and environmental factors (oxidative stress, shear stress, immunological response, and the absence of growth factors), their clearance is particularly rapid, with a half-life usually limited to 1–2 h [
19,
22]. The number of CTCs varies between 1 to 10 cells per 10 mL of blood, with higher counts detected in metastatic patients compared to early-stage cancers [
23,
24]. Given the extremely low count of CTCs, their adequate quantification requires special enrichment, detection and characterization technologies.
Positive enhancement methods, also known as label-dependent, use specific antibodies targeting molecular markers expressed by CTCs (cell-surface antigens). The membrane protein most commonly used during positive enhancement selection is the epithelial cell adhesion molecule (EpCAM), however, other cytoplasmic markers expressed by CTCs may be exploited (e.g., cytokeratin-8, -18, -19) [
26]. EpCAM is a transmembrane glycoprotein overexpressed in most epithelial solid tumors (breast cancer, ovarian cancer, head and neck squamous cell cancer, as well as CRC) and it is associated with cell proliferation, migration, invasion motility and signal transduction [
27]. It has been proved that circulating epithelial cells identified in cancer patients frequently carry the same genetic alterations as those observed in the primary tumor [
28]. However, CTCs are described by phenotypical heterogeneity, with some CTCs failing the selection process due to a lack of marker expression [
29]. In these conditions, negative selection methods could successfully isolate CTCs by identifying and excluding from analysis various non-malignant cells using antibodies recognizing cell surface markers expressed by these circulating blood cells [
25,
30]. In comparison, label-independent CTC enrichment methods subject CTCs to separation based on biophysical features such as density, size, deformability, electrical characteristics and invasiveness [
31]. A new assay, isolation by size of tumor cells (ISET), was developed to aid the morphological, immunological and molecular description of CTCs. ISET allows CTCs isolation based on biophysical differences between cancerous cells and non-malignant blood cells, collecting tumor cells using specific filters and chemical substances [
32].
Once the sample has undergone enrichment processes, CTCs require individual recognition. CTC detection can be achieved through immunocytology, molecular biology, or functional assays [
33]. The most widely used approach for CTC detection facilitates direct immunological identification by using anti-EpCAM antibody-labeled ferrofluids targeting proteins expressed by CTCs, with the CTCs being further detected via fluorescence microscopy [
19]. The development of this technique led to the implementation of CellSearch System as the only FDA-approved biotechnology adopted by clinical studies to detect and enhance CTCs [
34]. Research has also investigated the use of diagnostic leukapheresis (DLA) as a tool for enabling CTC detection when associated with the CellSearch System. Studies have demonstrated that DLA facilitates the screening of greater blood volumes for the presence of CTCs, as CTCs have similar densities as mononuclear cells and can be extracted from the bloodstream during leukapheresis [
35]. Another compelling approach to CTC detection comes in the form of the CellCollector GILUPI device, assessed as an in vivo CTC detection technique [
36]. On a molecular level, CTCs can be detected by extracting nucleic acids (mRNA, DNA, miRNAs) and then further submitting them to analysis through real-time polymerase chain reaction (RT-PCR) or next-generation sequencing (NGS) [
37]. Functional assays have been extensively researched as different techniques suited for CTC detection. The EPISPOT assay was tested as an in vitro CTC detection tool, able to select viable CTCs by recognizing specific proteins that are either secreted, released, or shed by cancerous cells [
38]. The EPISPOT assay was tested, among other settings, in the CRC setting, with encouraging results [
39]. Another approach to CTC selection comes in the form of dielectrophoresis. By utilizing specific electric fields, the DEPArray system allows the separation of single cells that can be later advanced to further comprehensive molecular characterization [
40].
However, despite promising results reported by clinical trials, the scientific community will have to overcome several limitations in order to further use the information provided by CTCs in clinical practice.
2.3. Exosomes
Present in all biological fluids, exosomes represent cell-derived nanovesicles with sizes ranging from 30 to 150 nm in diameter [
114]. Exosomes develop from the intracellular endosomal compartment following a process of inward expansion from the limiting membrane that generates multivesicular bodies (MVBs) [
115]. MVBs are then discharged into the extracellular matrix as a result of their fusion with the cytoplasmic membrane, releasing their content in the form of exosomes [
116]. Exosomal secretion occurs in both physiological and pathological processes, with various types of cells producing exosomes (cancer cells, as well as adipocytes, immune cells and brain cells) [
117]. Exosomes play a series of roles within the cell, notably the removal of waste, antigen presentation and cytokine release [
118]. However, their essential function is intercell communication of molecular information [
119]. Exosomal cargo, mainly cytoplasmic components such as proteins, bio-functional lipids and nucleic acids (mRNA, miRNA and DNA fragments) are key players in the signaling pathways between cells [
120]. Communication between exosomes and their target cells can be acquired through interaction with surface-expressed ligands, through phagocytosis, or by exosomal fusion with cell membranes [
121].
An increasing amount of evidence has identified exosomes as essential participants in cancer development processes. Exosomes secreted by tumor cells have been found responsible for alterations in the immune response that lead to suppression of antitumor response [
122]. In addition, exosomes play important roles in tumor microenvironment (TME) remodeling, angiogenesis and tumor growth, therefore favoring disease progression [
118]. Exosomes were found to promote EMT, migration and invasion, causing distant cancer dissemination through various proteins and miRNAs [
123]. Furthermore, research has proved that exosomal signaling pathways are also involved in therapy resistance [
123,
124]. Since exosomes have the ability to target specific cells [
125], technologies have investigated the possibility of manipulating exosomes for therapeutical purposes, by using them as potential vehicles for drug delivery inside tumor cells [
126].
Exosome concentration in biological fluids is relatively low, thus making their isolation, detection and further analysis relatively challenging. Isolation of exosomes can be achieved based on their physical properties (size and density), electromagnetic characteristics, or according to their immunological properties [
127]. Isolation through ultracentrifugation represents the gold standard, however, other techniques, such as ultrafiltration, chromatography, hydrostatic filtration dialysis, precipitation, microfluidic chips, or immunoaffinity-based methods, may also facilitate exosome isolation [
127]. Following isolation, the detection and characterization of exosomes from a morphological point of view is obtained through transmission electron microscopy [
128]. Nanoparticle tracking analysis can determine size and concentration characteristics [
129]. Protein expression and functions can be assessed using Western blot and ELISA methods, while exosome content can be identified via spectrophotometric assays and different other focused approaches (e.g., RT-qPCR, Western blot and mass spectrometry) [
127,
130].
Exosomal microRNAs have been attracting considerable attention as promising biomarkers suitable for cancer diagnosis. Multiple exosomal miRNAs have been studied, with some of them showing substantial value in identifying early cases of CRC .
Research has identified several significantly up-regulated miRNAs in the setting of CRC, including cases of early-stage disease. One study found miRNA-23a to have an important diagnostic accuracy with an area under the curve (AUC) of 0.953, while miRNA-1246 and miRNA-21 also showed encouraging results [
131]. Overexpression of exosomal miRNA-23a was successfully confirmed by another study that additionally investigated the diagnostic value of exosomal miRNA-301a [
132]. Another study conducted by a Chinese team demonstrated the overexpression of exosomal miRNA-6803-5p in the serum of CRC patients [
133]. Similarly, the expression of miRNA-486-5p in plasma exosomes was found to be significantly upregulated in CRC patients, corresponding to disease staging [
134]. Circulating exosomal miRNA-125a-3p is another upregulated analyte with confirmed value in detecting early-stage CRC patients. The predictive accuracy was improved when associating miRNA-125a-3p with CEA analysis [
135]. The same study found exosomal miRNA-320c to be up-regulated in plasma samples collected from CRC patients, validating it as a potential biomarker for early diagnosis [
135]. Downregulation of serum exosomal miRNA-150-5p proved to be a conclusive indicator of colorectal malignancy, while combined analysis with CEA resulted in a higher diagnostic value for CRC identification [
136]. Interestingly, expression of exosomal miRNA-92b was found to be significantly reduced in patients presenting with CRC, as well as individuals with adenomas of the colon [
137]. Furthermore, serum samples and serum exosomes isolated from CRC patients also showed a considerable expression of mRNA-196b-5p [
138]. Additional data identified a downregulation in exosomal miRNA-139-3p expression in plasma samples collected from patients with CRC, correlating with disease aggressiveness [
139]. Furthermore, plasma collected from CRC patients was found to express important levels of exosomal miRNA-27a and miRNA-130a [
140]. A different study found upregulation of miRNA-1359 in exosomes isolated from CRC patients, leading to an accurate differentiation of CRC cases from healthy individuals [
141]. Exosomal miRNAs are receiving a growing interest, with several other studies aiming to identify and validate promising biomarkers for early CRC diagnosis and population screening [
131,
142,
143,
144]. In the given circumstances, the need to improve the accuracy of these biomarkers is evident.
3. The Future Applications of Liquid Biopsies in CRC
Over the past few years, immunotherapy has changed the treatment paradigm for many cancer types. In CRC, the MSI-high phenotype was associated with a significant response to immune checkpoint inhibitors (ICIs) [
145]. Moreover, the tumor mutational burden (TMB), referring to the number of somatic mutations, was significantly correlated with the outcome of CRC patients treated with ICIs [
146]. Despite the promising results reported by the scientific community, we face a poor prediction of response to ICIs, along with important rates of innate or acquired resistance leading to heterogenous responses among patients [
147]. Biomarker-directed use immunotherapy is an important frontier in precision medicine.
To date, liquid biopsies are investigated for use as biomarkers to predict and evaluate the response to immunotherapy. CTCs, circulating DNA (cDNA), circulating RNA (cRNA) and exosomes hold a generous amount of tumor-related information. Moreover, liquid biopsies may provide a more comprehensive and dynamic overview of the tumor microenvironment and heterogeneity than single-site tissue biopsies [
148]. The utility of cDNA as a prognostic and predictive biomarker for immunotherapy was shown in a phase II trial including patients with advanced or metastatic solid tumors treated with an anti-PD1 agent. The study reported that higher pretreatment variant allele frequencies (VAF) were associated with a poorer OS. However, on-treatment VAF and on-treatment reduction in VAF were correlated with longer PFS and OS [
149]. These findings suggest that on-treatment cDNA variations can predict a beneficial response to ICIs. Similarly, another phase II prospective trial assessed cDNA in patients with advanced solid tumors under treatment with pembrolizumab. Low baseline cDNA levels were correlated with PFS, OS, clinical response and clinical benefit. Moreover, the reduction of cDNA after only two cycles of pembrolizumab and cDNA clearance on-treatment identified a good prognosis subset of patients [
150].
A better selection of the patients receiving immunotherapy could be guided by specific somatic mutations detectable in cDNA. In this regard, a genomic mutation signature was developed to characterize immunophenotypes and predict response to immunotherapy in gastrointestinal cancers [
151]. As mentioned above, the number of somatic mutations known as TMB represents an independent predictor of response to ICIs in many solid tumors, including CRC. TMB-high cases (≥20 mutations/megabase) typically occur in microsatellite instable tumors (MSI) or those harboring pathogenic mutations emerging in the DNA polymerases POLD and POLE [
152]. Currently, the standard evaluation for TMB is based on tissue samples and encounters many limitations. Tissue-based biopsies cannot correctly assess intratumoral heterogeneity or evaluate the changes occurring during treatment [
153]. In this regard, cDNA-based evaluation of TMB (cTMB) is currently being investigated in clinical trials, with encouraging results obtained in non-small cell lung cancer (NSCLC). The concordance between tissue-based TMB and cDNA-based TMB was strong in clinical trials, suggesting that cTMB could be a feasible predictive biomarker for ICIs [
154]. Due to recent technological advances, circulating tumor cell PD-L1 expression is being investigated in clinical trials as a predictive biomarker for response to ICIs [
155]. However, further scientific evidence is needed to clarify the similarities between PD-L1 detection on CTCs and tissue expression of PD-L1. Moreover, considering their rarity in the bloodstream, the utility of CTCs in immunotherapy is still in the early stages [
156]. Nonetheless, emerging studies are documenting the role of extravesicles (EVs) as potential biomarkers for immunotherapy. Therefore, EV-based liquid biopsies could eventually identify tumor-expressed proteins, DNA mutations, RNA landscape, and T-cell reactivity in patients under treatment with ICIs [
157].
RAS assessment in mCRC is essential to select patients suitable for anti-EGFR therapy. The concordance between tissue detection and somatic mutations detected in ctDNA appeared high in patients with advanced tumors, supporting blood-based testing. Moreover, ctDNA was shown to be highly useful for monitoring treatment response. However, some clinicopathological features, including tumor histology (mucinous) and metastatic sites (peritoneal, lung), negatively influenced RAS detection in ctDNA [
158]. Along with RAS mutation, TP53 mutations were widely detected in the ctDNA of CRC patients, with a high correlation between tissue and plasma detection. In CRC patients who did not progress to metastatic disease after primary surgery, the VAF for TP53 mutations decreased. By contrast, increased levels were associated with the development of liver metastasis [
159]. Moreover, TP53 mutations were significantly correlated with increased VEGFA mRNA tissue expression, suggesting that these patients are expected to benefit from anti-VEGF therapy [
160]. Nonetheless, TP53 mutations might occur as a consequence of several treatment strategies. In CRC, these mutations were particularly linked to cetuximab therapy, leading to resistant clones, and, therefore, influencing treatment opportunities [
161].
Immunotherapy and targeted therapy are major therapeutic breakthroughs in cancer care, and one of the most challenging concerns is proper patient selection. To overcome these shortcomings, liquid biopsy-based biomarkers represent a promising tool, hence they require detection methods with sufficient specificity, sensitivity and predictive power [
162].
4. Remaining Obstacles in Clinical Applications of Liquid Biopsy
Despite many pieces of scientific evidence highlighting the potential benefits of liquid biopsies in cancer care, numerous limitations remain for their clinical use.
CTCs have great potential as diagnostic, prognostic, predictive, as well as monitoring tools. However, their translation into clinical practice is still restricted amid their isolation from the bloodstream [
163]. To correctly identify and analyze CTCs, it is essential to understand the obstacles surrounding their use. An important challenge is their extreme rarity, which makes them hard to locate. Among blood cells, CTCs are considered to beone in a million, or a billion [
164]. Moreover, their concentration is much lower in the early stages compared to metastatic disease. Another important issue regards the size, physical characteristics and complexity of surface protein expression [
165]. The main techniques used for CTCs enrichment are antigen-dependent (positive or negative selection), antigenindependent, or a combination of both [
166]. In the case of positive selection, the efficacy of CTCs affinity is mainly influenced by antibody selectivity in the enrichment process. In this regard, the antibodies utilized may suffer from low selectivity as the target cell-surface proteins could also be expressed on other cells. Antibody cocktails targeting several cellsurface proteins have been used to overcome this limitation [
166]. Moreover, the negative enrichment methods using magnetic bands to deplete circulating platelets and leucocytes have also been used to overcome the limitations of positive enrichment [
167]. While using antigen-independent methods, the isolation of CTCs depends on the electric charge, density, size and deformability. However, with these techniques, CTCs purity is usually low due to size overlapping with WBC [
168].
For exosomal segregation, ultracentrifugation is thought to be the most efficient method. Although convenient and requiring reasonable costs, ultracentrifugation encounters several limitations. A significant concern is the co-purification of lipoproteins and protein aggregates along with EVs [
169]. Hence, it could be overcome by combining ultracentrifugation with density-gradient mechanisms. However, the structures with similar densities are indistinguishable. Immune isolation targets EVs with a particular surface marker representing a more specific method. Nonetheless, the targeted surface marker could also be found on other EV subsets [
170].
ctDNA is a small fraction representing about 0.01% of cfDNA. One of the main logistical reasons limiting the extensive use of cDNA-based analysis is represented by their feasibility outside the academic cancer centers [
171]. The available techniques for cDNA detection are based on PCR and NGS. These techniques were updated over time to better fit the low concentrations in the bloodstream. However, despite their sensitivity, PCR-based assays are limited by a low multiplexing capacity that permits the analysis of a small number of loci [
172]. On the other hand, the sensitivity of NGS-based assays is low and inversely proportional to the examined loci [
163,
173]. Another concerning issue implies the predictive value of a small set of mutations which could also be found in healthy individuals due to clonal hematopoiesis [
173]. Moreover, the preanalytical sample preparation of cDNA lacks standardization limiting its implementation into clinical practice. Currently, a significant limitation preventing cDNA molecular panels in CRC is the lack of precise data showing that liquid biopsy findings could drive the therapeutic approach [
174]. Similar to cDNA, the most relevant limitation in cRNA analysis is represented by preanalytical and analytical phases, along with a lack of standard extraction protocols [
175]. A critical issue implies the hemolytic process, which occurs during extraction and preparation and can influence the levels of detected miRNAs. For this reason, monitoring the hemolysis of all samples in a pre-analytical phase is mandatory [
176]. Another essential constraint regards residual platelets and microparticles resulting from plasma processing that can influence miRNA measurements [
177]. Moreover, it is difficult to determine if the levels of plasma miRNA are confounded by comorbidities or are cancer-related. Therefore, a significant challenge is establishing which body fluid detection method is the most appropriate for CRC screening [
78].
Even if several logistic and biological limitations are encountered at the present moment, liquid biopsies will more likely become a fundamental tool in the management of CRC patients in all stages of disease-related interventions. Evaluation of ctDNA levels in patients with stage II CRC has led to a decrease in adjuvant chemotherapy administration while maintaining a favorable recurrence-free survival (DYNAMIC II study) [
178]. Additionally, the ongoing DYNAMIC III study attempts to evaluate a ctDNA-guided treatment approach in the setting of stage III CRC [
179]. Liquid biopsy also plays an important role in assessing minimal residual disease, guiding the timing of therapeutic interventions based on ctDNA levels obtained at crucial points during treatment [
180]. Furthermore, extensive research has proved that liquid biopsy offers strong indicators of early disease recurrence, with a significant median lead time of 8.7 months over conventional assessment methods [
181]. Liquid biopsies have demonstrated valuable clinical application in detecting patients with acquired resistance to anti-EGFR therapy, therefore allowing a better selection of cases who may benefit from an EGFR rechallenge [
182]. For CRC early diagnosis, however, comprehensive studies comparing the available data on liquid biopsy to current screening methods are necessary in order to find the most advantageous clinical use in everyday practice.
5. Conclusions
Despite the implementation of extensive programs designed to diagnose CRC in the early stages, the adherence of the general population to screening protocols remains unsatisfactory. Liquid biopsy comes as a novel, minimally invasive tool, adequate for early diagnosis of malignancy while also attempting to overcome the limitation showed by traditional CRC screening and tissue sampling methods. Research has proved that liquid biopsy analytes and biomarkers offer valuable information regarding carcinogenesis and could indeed single out individuals at risk for developing CRC or those presenting early-stage CRC otherwise undetected during conventional screening tests.
Since FDA has taken the necessary steps to approve CellSearch System for CTC detection and enhancement during clinical studies, the scientific community could soon implement the test in everyday clinical practice. In addition, studies have identified numerous methylation markers indicative of malignancy. In this regard, the detection of SEPT9 gene methylation in DNA fragments derivative from tumor masses is the most widely explored sequence and therefore experiences more promising results. As a result of thorough research, the SEPT9 methylation model comes within reach of validation for current practice, with tests such as Epi proColon expressing significant diagnostic values for CRC early detection. Several extensively researched miRNAs are also approaching clinical utility in everyday practice. miRNA-92a proves relevant sensitivity and specificity values in detecting early CRC cases, as well as advanced adenomas, while panels including multiple miRNAs show improved accuracy when compared to single markers. Additionally, exosomal miRNA-23a has been shown to differentiate patients with early-stage disease with high accuracy, indicating that protocols defining its clinical applicability could be imminent.
However, in order to successfully isolate compelling biomarkers, blood samples require complex manipulation techniques that often show unsatisfactory efficiency and prove to be time-consuming and costly. Studies conducted thus far have demonstrated encouraging accuracy, yet further research is critical in order to validate liquid biopsy as a screening and early diagnostic technique. Furthermore, the utility of liquid biopsies in the era of precision medicine is an important frontier that demands thorough inquiry.