A form of systemic vasculitis that affects mostly small and medium-sized vessels, Kawasaki disease (KD) is most commonly found in children under the age of 5 years old. Though its etiology is unknown, KD has been the most frequent acquired heart disease in developing countries. The most severe complications of KD are coronary artery lesions (CAL), including dilation, fistula, aneurysm, arterial remodeling, stenosis, and occlusion. Aneurysm formation has been observed in 20-25% of KD patients that do not receive intravenous immunoglobulin (IVIG) treatment, and in 3-5% that do receive it. Coronary artery dilation has been found in about 30% of KD patients in the acute stage, although mostly in the transient form. Diminishing the occurrence and regression of aneurysm is a vital part of treating KD. This review is focuing on coronary artery aneurysm prevention in KD.
- Kawasaki disease, aneurysm, prevention
Coronary aneurysm prevention in Kawasaki Disease
HO-CHANG KUO, MD, PhD, FAAAAI
Kawasaki Disease Center and Department of Pediatrics, Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Taoyuan, Taiwan. 83301.
erickuo48@yahoo.com.tw or dr.hckuo@gmail.com
Introduction
Kawasaki disease (KD) is recognized as the most frequent acquired heart disease in children. Dr. Kawasaki et al. first described this acute febrile systemic vasculitis in Japan in 1967. It mainly affects children under the age of 5 years old, especially those in such Asian countries as Japan, Korea, Taiwan, and China. The most severe complication is the formation of coronary artery lesions (CAL), such as myocardial infarction, coronary artery fistula, coronary artery dilatation, and coronary artery aneurysm, which may result in long-term sequelae like stenosis or obstruction and myocardial infarction. The etiology of KD continues to be unknown.
KD may be caused by a combination of genetic background (CD40, BLK, ITPKC, FCGR2A,FCGR2B,CD40L,CASP3. etc.), infectious agents (bacteria, virus, mycoplasma, COVID-19[1].etc.)[2][3][4] and the aberrant T cell immune response. The standard treatment for KD is high-dose aspirin and high-dose intravenous immunoglobulin, which have been shown to significantly decrease the rate of coronary artery aneurysms from 20-25% to 3-5%. The effectiveness of IVIG for treating KD is still under investigation, FCGR2A may be the key factor from evidence of genome-wide association study (GWAS) and methylation array results. Hypomethylation of CpG sites in the FCGR2A promoter region were related to KD susceptibility and IVIG resistance; mRNA gene expression also confirmed such findings.
While IVIG treatment significantly decreases the occurrence of coronary artery aneurysm formation, about 1/3 of KD patients will still develop coronary artery dilation in the acute stage. Identifying KD during the 5-10 days of disease onset is very important, as is treating KD with a more precise protocol, especially for those children with IVIG resistance, in a high-risk group, or with CAL formation. In this article, we demonstrate the clinical practice of preventing aneurysm formation and regression.
Typical and atypical Kawasaki disease
Clinical diagnosis criteria (Kuo Mnemonic: 1-2-3-4-5)
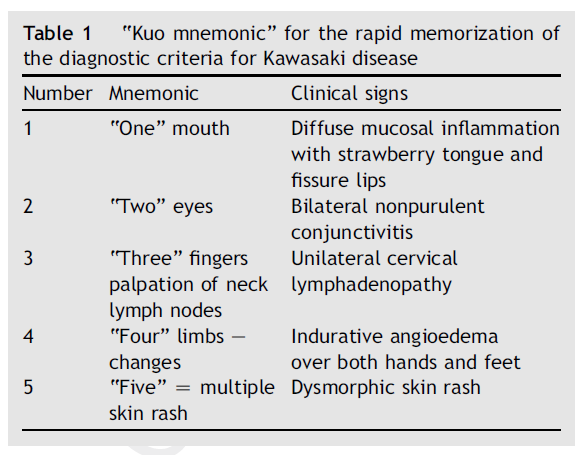
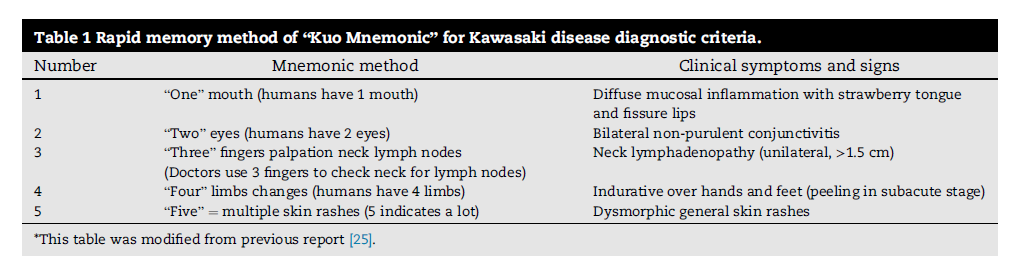
The clinical characteristics of KD include fever lasting for more than 5 days, as well as at least four of the following five symptoms: diffuse mucosal inflammation with strawberry tongue and fissure lips (1 mouth), bilateral non-purulent conjunctivitis (2 eyes), unilateral cervical lymphadenopathy (3 fingers check lymph node), indurative angioedema over the hands and feet (4 limbs), dysmorphic skin rashes (5 or more skin rashes). The “Kuo Mnemonic” help to quickly recall KD diagnosis criteria (as shown in Table 1). According to the Japanese Circulation Society Joint Working Groups’ criteria (JCS 2008, Guidelines for diagnosis and management of cardiovascular sequelae in KD), KD can be diagnosed even when a fever occurs for less than 5 days. However, according to the American Heart Association (AHA) criteria, a fever lasting for 4-5 days or more is essential for a diagnosis of KD.
Bacillus Calmette-Guérin (BCG) site induration is a specific sign for Kawasaki disease
In countries with a routine BCG immunization policy, an erythematous change over BCG scars will be observed in nearly 40-50% of KD patients. The bull's eye dermatoscopic sign can serve as a severity biomarker of CAL formation in KD. Redness or the formation of a crust at the BCG inoculation site is a useful sign for diagnosing KD in children. If a patient has less than 4 major signs of the KD clinical criteria, physicians should consider redness or crust formation at the BCG inoculation site as a possible indicator of KD.[5]
Consulting a Kawasaki disease expert
A KD expert (including cardiologist, immunologist, infectious disease specialist, or rheumatologist) should be consulted when fever lasts for more than 7 days without a definitive diagnosis. The major diagnosis of KD depend on five clinical symptoms and echocardiography, which causes diagnosis to be subjective. Consulting a KD expert will improve the subjectivity of making diagnosis for KD. Expertscape provides a good way to find KD experts throughout the world (www.expertscape.com).
AHA supplemental criteria
The AHA and American Academy of Pediatrics (AAP) released the KD supplemental laboratory criteria in 2004 for patients suspected of having KD but with an incomplete diagnosis, which included the following six components: (1) urine ≥10 white blood cells/high-power field; (2) albumin ≤3.0 g/dL; (3) elevation of alanine aminotransferase; (4) platelet count ≥450,000/mm3after 7 days of fever; (5) total white blood cell count ≥15,000/mm3; and (6) anemia by age. If a patient meets more than three of the supplementary criteria, incomplete KD can be diagnosed, and IVIG should be prescribed before arranging for echocardiography.[6]
Treating Kawasaki disease and IVIG resistance with precision medicine
IVIG
A single high dose of IVIG (2 g/kg in 10-12 hours infusion) within 5-10 days of disease onset and high-dose aspirin (30-50 or 80-100 mg/kg/day) are currently considered the gold standard for treating KD. IVIG treatment should not be spread out over 24 hours, 2 days, or 4 days. IVIG treatment should not be interrupted in case of fever occur during infusion.
Aspirin
Aspirin has been used to treat KD for more than 40 years, even before IVIG prescription. While aspirin has important anti-inflammatory (high dose) and anti-platelet (low dose) functions, it does not appear to reduce the occurrence of CAL formation. During acute-phase KD, aspirin is administered at 80 to 100 mg/kg per day (30-50 mg/kg in Japan). High-dose aspirin in the acute stage of KD does not affect the response rate of IVIG therapy, duration of fever, or incidence of CAL when children are also treated with a single infusion of high-dose IVIG. Administering high-dose aspirin in acute-stage of KD does not provide benefits with regard to inflammation markers (C-reactive protein, hepcidin, and hemoglobin levels). The use of high-dose aspirin in the acute stage of KD still needs multi-center randomized controlled trials before a conclusive determination can be reached. After the fever subsides, dosage of aspirin should be reduced to 3-5 mg/kg/day and should be continued for at least 6-8 weeks after disease onset or till normalization of CAL.[7]
IVIG resistance (non-responsiveness or failure)
KD with IVIG-resistance are at a higher risk of CAL formation and need more aggressive therapy. A second dose of IVIG (2 g/kg) , intravenous methylprednisolone pulse therapy (IVMP, 30 mg/kg with a maximum dose of 1000 mg), tumor necrosis factor-alpha blockade, cyclophosphamide, cyclosporine A, methotrexate, plasmapheresis , and plasma exchange have been reported to benefit KD patients with IVIG resistance. In the Kawasaki Disease Center of Kaohsiung Chang Gung Memorial Hospital in Taiwan, we used a secondary course of high-dose IVIG (2 g/kg in 10-12 hours) for initial IVIG-resistant KD patients; then we prescribed IVMP (30 mg/kg/day, for 3 days) for continued IVIG resistance in the secondary dose; and then anti-TNF-alpha agent for resistance to IVMP.[8]
Preventing coronary artery aneurysm formation
Treatment for KD patients with a proper dosage of IVIG (a single high dose of 2 g/kg) in the proper duration of 10-12 hours infusion, prescribed within the first 5-10 days of the illness will more effectively prevent aneurysm formation. If KD patients are found to be have CAL formation even before the 5th day from the onset of the disease, IVIG should be given. IVIG should also be administered to KD patients presenting after the 10th day of illness (i.e., children in whom the diagnosis was missed earlier) if they have either ongoing systemic inflammation, persistent fever without other explanation or aneurysm formation.
Echocardiography should be considered for patients who were suspected to have KD with peeling (or even those not) at admission but did not meet the diagnostic criteria after they are discharged from the hospital. Clinicians should pay special attention to those who with elevated neutrophil-to-lymphocyte ratios (> 1.33) and CRP levels (>33 mg/L) and closely follow up such patients.[9] For patients with severe KD or those in a high-risk for IVIG resistance, adding prednisolone to IVIG could significantly improve coronary artery outcomes.
Conclusion
Increasing KD awareness with the rapid memory methods of the Kuo Mnemonic, early diagnosis (through echocardiography, supplemental criteria, and BCG induration), precise treatment (IVIG, 2nd dose IVIG, IVMP, anti-TNF-alpha) and precision medicine (steroid or dextromethorphan or other anti-inflammatory agents) will all help diminish the coronary artery damage from KD and prevent aneurysm.[10]
References
- Ho-Chang Kuo; Kawasaki-like disease among Italian children in the COVID-19 era. The Journal of Pediatrics 2020, 224, 179-183, 10.1016/j.jpeds.2020.07.022.
- Yi-Ching Lee; Ho-Chang Kuo; Jeng-Sheng Chang; Luan-Yin Chang; Li-Min Huang; Ming-Ren Chen; Chi-Di Liang; Hsin Chi; Fu-Yuan Huang; Meng-Luen Lee; et al. Two new susceptibility loci for Kawasaki disease identified through genome-wide association analysis. Nature Genetics 2012, 44, 522-525, 10.1038/ng.2227.
- Ho-Chang Kuo; Jen-Chieh Chang; Hsing-Chun Kuo; Hong-Ren Yu; Chih-Lu Wang; Chiu-Ping Lee; Li-Tong Huang; Kuender D. Yang; Identification of an Association Between Genomic Hypomethylation ofFCGR2Aand Susceptibility to Kawasaki Disease and Intravenous Immunoglobulin Resistance by DNA Methylation Array. Arthritis & Rheumatology 2015, 67, 828-836, 10.1002/art.38976.
- Tai-Ming Ko; Ho-Chang Kuo; Jeng-Sheng Chang; Shih-Ping Chen; Yi-Min Liu; Hui-Wen Chen; Fuu-Jen Tsai; Yi-Ching Lee; Chien-Hsiun Chen; Jer-Yuarn Wu; et al. CXCL10/IP-10 Is a Biomarker and Mediator for Kawasaki Disease. Circulation Research 2015, 116, 876-883, 10.1161/circresaha.116.305834.
- Han-Chi Tseng; Ji-Chen Ho; Mindy Ming‐Huey Guo; Mao‐Hung Lo; Kai‐Sheng Hsieh; Wen‐Chien Tsai; Ho-Chang Kuo; Chih-Hung Lee; Bull's eye dermatoscopy pattern at bacillus Calmette-Guérin inoculation site correlates with systemic involvements in patients with Kawasaki disease. The Journal of Dermatology 2016, 43, 1044-1050, 10.1111/1346-8138.13315.
- Brian W. McCrindle; Anne H. Rowley; Jane W. Newburger; Jane C. Burns; Anne F. Bolger; Michael Gewitz; Annette L. Baker; Mary Anne Jackson; Masato Takahashi; Pinak B. Shah; et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation 2017, 135, e927-e999, 10.1161/cir.0000000000000484.
- Ho-Chang Kuo; Mao-Hung Lo; Kai-Sheng Hsieh; Mindy Ming-Huey Guo; Ying-Hsien Huang; High-Dose Aspirin Is Associated with Anemia and Does Not Confer Benefit to Disease Outcomes in Kawasaki Disease. PLOS ONE 2015, 10, e0144603, 10.1371/journal.pone.0144603.
- Ling-Sai Chang; Ho-Chang Kuo; The role of corticosteroids in the treatment of Kawasaki disease.. Expert Review of Anti-infective Therapy 2020, 18, 155-164, 10.1080/14787210.2020.1713752.
- Jia-Huei Yan; Ling-Sai Chang; Yi-Ju Lin; Mindy Ming-Huey Guo; Ying-Hsien Huang; Ho-Chang Kuo; Clinical Characteristics for Differentiating Febrile Children With Suspected Kawasaki Disease Diagnosis. Frontiers in Pediatrics 2020, 8, 221, 10.3389/fped.2020.00221.
- Ho-Chang Kuo; Preventing coronary artery lesions in Kawasaki disease. Biomedical Journal 2017, 40, 141-146, 10.1016/j.bj.2017.04.002.
