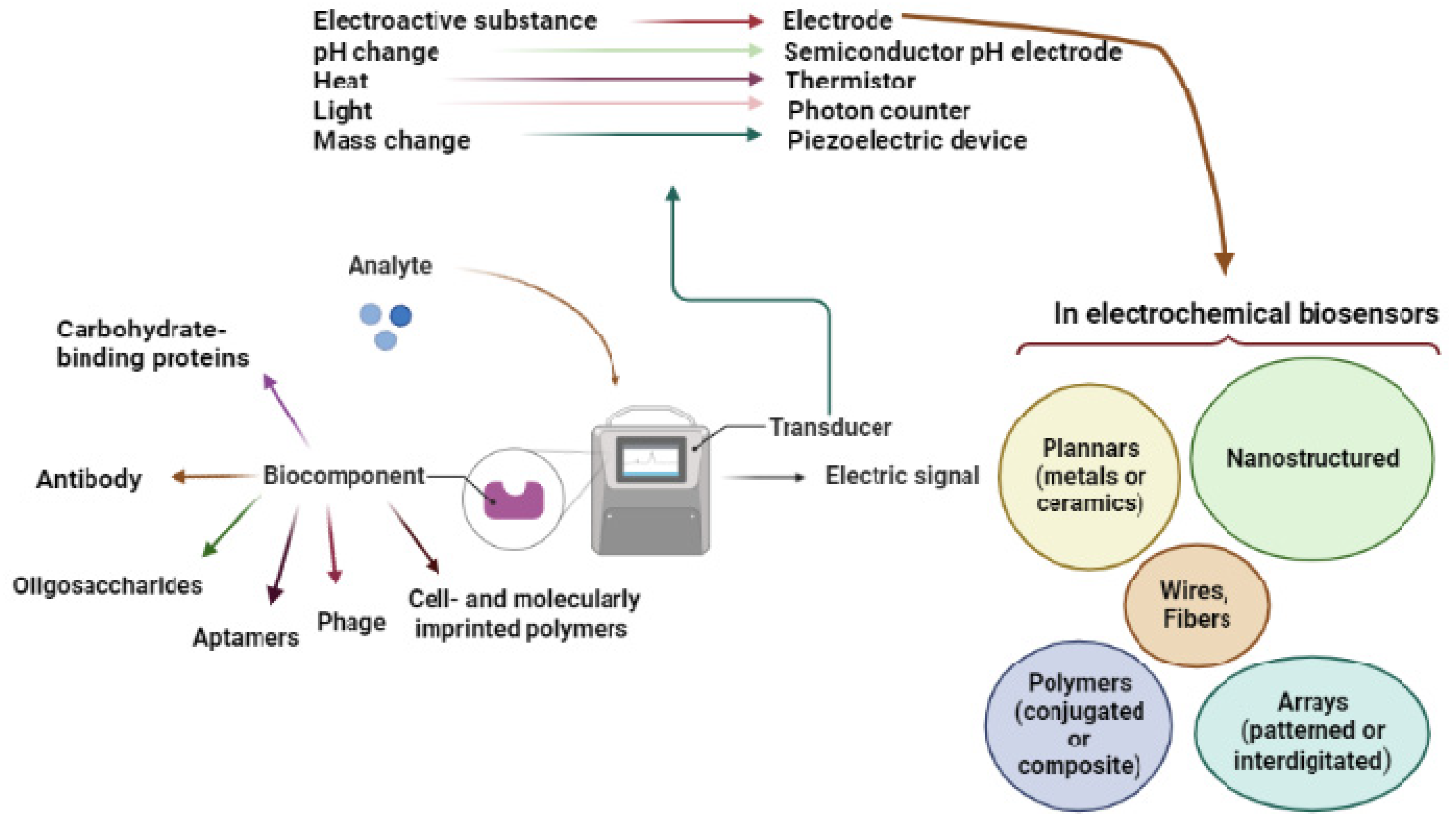
Electrochemical biosensors are a family of biosensors that use an electrochemical transducer to perform their functions. In recent decades, many electrochemical biosensors have been created for pathogen detection. These biosensors for detecting infections have been comprehensively studied in terms of transduction elements, biorecognition components, and electrochemical methods. The integration of transducers and electrode changes in biosensor design is a major discussion topic. Pathogen detection methods can be categorized by sample preparation and secondary binding processes. Diagnostics in medicine, environmental monitoring, and biothreat detection can benefit from electrochemical biosensors to ensure food and water safety.
- electrochemical
- biosensors
- pathogen quantification
1. Introduction
| Recognition Element | Advantages | Disadvantages | Reference(s) |
|---|---|---|---|
| Antibodies | High affinity High selectivity |
Selectivity may be affected by antibody labeling Alteration of binding affinity to antigen Low temperature High cost |
[47][48][49] |
| Carbohydrate binding proteins | Binding ligands unique to the Target organism Low cost High-yield automated synthesis |
Pathogens detection abilities using electrochemical biosensors lack sufficient data | [41][50] |
| Oligosaccharides | Pathogens have receptors for Carbohydrate-specific trisaccharides Utilized with electrochemical biosensors |
Limited selectivity Low affinity Carbohydrate–protein interaction |
[41][51] |
| Oligonucleotides | Utilized with electrochemical biosensors Strong binding affinity and selectivity Low cost Feasible to extract and amplify particular binding sequences |
Possibility of cross-reactions Lack of repeatability when using different procedures Degradation of aptamers |
[52][53] |
| Cell-and molecular-imprinted polymers | Use morphology particular to target | Poor selectivity | [54][55] |
| Phages | Utilized with electrochemical biosensors Effective biorecognition component in water monitoring |
High cost | [56][57] |
| Bacteria/Virus | Method and Materials | Biorecognition Element | * LOD/LOQ | Year | Reference(s) |
|---|---|---|---|---|---|
| E. coli | Electrochemical impedance spectroscopy | Polyclonal anti-E. coli | 104 CFU/mL | 2005 | [58] |
| V. cholerae | Carbon electrode | Polyclonal anti-V. cholerae | 8 CFU/mL | 2006 | [59] |
| L. monocytogenes | Electrode nanostructuring | Monoclonal anti-L. monocytogenes | 4.7 × 102 CFU/mL | 2008 | [60] |
| S. typhimurium | Ceramic electrodes | Anti-S. typhimurium | 103 CFU/mL | 2009 | [61] |
| West Nile virus (WNV) | Anodic stripping voltammetry | Monoclonal anti-WNV | 0.02 viruses/mL | 2009 | [62] |
| B. anthracis | Ag electrode (Conductometry) | Monoclonal and polyclonal anti-B. anthracis | 420 spores/mL | 2009 | [63] |
| Campylobacter jejuni | Nanoparticles on carbon electrode | Monoclonal anti-Flagellin A | 103 CFU/mL | 2010 | [64] |
| Bovine viral diarrhea virus (BVDV) | Nanofiber array electrode (Conductometry) | Monoclonal and polyclonal anti-BVDV | 103 CCID **/mL | 2010 | [65] |
| Helicobacter pylori | Graphene interdigitated microelectrode array (Conductometry) | Odoranin-HP peptide | 100 cells | 2012 | [66] |
| L. innocua | Phage | L. innocua-specific bacteriophage | 1.1 × 104–105 CFU/mL | 2012 | [67] |
| E. coli | Cell- and molecularly imprinted polymers | Anti-E. coli | 1.6 × 108 Cells/mL | 2014 | [68] |
| E. coli | Composite on carbon electrode | Anti-E. coli | 13 CFU/mL | 2014 | [69] |
| S. typhimurium | Electrochemical Impedance Spectroscopy (EIS) | Monoclonal anti-S. typhimurium | 3 × 103 CFU/mL | 2015 | [70] |
| Enterococcus faecalis | Carbon-based electrodes on Au electrode | Clavanin A peptide | 103 CFU/mL | 2015 | [71] |
| Dengue virus | AuNPs on Au electrode | Anti-DENV | --------------- | 2015 | [72] |
| Norovirus | Au microelectrode (square wave voltammetry) | Anti-norovirus aptamer | 10 PFU ***/mL | 2016 | [73] |
| Rotavirus | Electrochemical Impedance Spectroscopy (EIS) and nano structuring | Anti-rotavirus | 2.3 PFU/mL R2 ****: 0.993 |
2016 | [74] |
| S. epidermidis | Au microelectrode (Electrochemical Impedance Spectroscopy) | S. epidermidis-imprinted polymer film | 103 CFU/mL | 2017 | [75] |
| Influenza A virus (H1N1) | Oligosaccharides (PEDOT:PSS) | Hemagglutinin-specific trisaccharide ligand | 0.13 HAU ***** | 2017 | [51] |
| E. coli and human influenza A virus | Polymer electrode | Hemagglutinin-specific trisaccharide ligand | 0.025 HAU | 2018 | [76] |
| E. coli | Carbohydrate binding proteins | Anti-E. coli | 12 CFU/ml ----------------- 6.0 × 103–9.2 × 107 CFU/mL |
2011 ------ 2019 |
[41][77] |
| SARS-CoV-2 | CRISPER-Cas | --------------- | Fold change: 10 | 2020 | [78] |
| S. typhimurium | DNA functionalized | Amine labeled S. Typhi | 6.8 × 10−25 molL−1 | 2022 | [79] |
| SARS-CoV-2 | Electrochemical immunosensor | SARS-CoV-2 spike protein | 12 ng/mL–40 ng/mL | 2022 | [80] |
2. Transduction Elements
2.1. Metal Electrodes
2.2. Ceramic Electrodes
2.3. Polymer Electrodes
2.4. The shape and Design of the Electrodes
This entry is adapted from the peer-reviewed paper 10.3390/bios12110927
References
- Dye, C. After 2015: Infectious diseases in a new era of health and development. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130426.
- Khan, R.S.; Khurshid, Z.; Yahya Ibrahim Asiri, F. Advancing point-of-care (poc) testing using human saliva as liquid biopsy. Diagnostics 2017, 7, 39.
- Moonla, C.; Lee, D.H.; Rokaya, D.; Rasitanon, N.; Kathayat, G.; Lee, W.-Y.; Kim, J.; Jeerapan, I. Review—Lab-in-a-mouth and advanced point-of-care sensing systems: Detecting bioinformation from the oral cavity and saliva. ECS Sens. Plus 2022, 1, 021603.
- Nasrollahzadeh, M.; Sajjadi, M.; Soufi, G.J.; Iravani, S.; Varma, R.S. Nanomaterials and nanotechnology-associated innovations against viral infections with a focus on coronaviruses. Nanomaterials 2020, 10, 1072.
- Hamid, H.; Khurshid, Z.; Adanir, N.; Zafar, M.S.; Zohaib, S. COVID-19 pandemic and role of human saliva as a testing biofluid in point-of-care technology. Eur. J. Dent. 2020, 14, S123–S129.
- Yi, Z.; de Dieu Habimana, J.; Mukama, O.; Li, Z.; Odiwuor, N.; Jing, H.; Nie, C.; Hu, M.; Lin, Z.; Wei, H.; et al. Rational programming of cas12a for early-stage detection of COVID-19 by lateral flow assay and portable real-time fluorescence readout facilities. Biosensors 2022, 12, 11.
- Simoska, O.; Stevenson, K.J. Electrochemical sensors for rapid diagnosis of pathogens in real time. Analyst 2019, 144, 6461–6478.
- Dhar, B.C. Diagnostic assay and technology advancement for detecting SARS-CoV-2 infections causing the COVID-19 pandemic. Anal. Bioanal. Chem. 2022, 414, 2903–2934.
- Liu, Y.; Wang, J.; Song, X.; Xu, K.; Chen, H.; Zhao, C.; Li, J. Colorimetric immunoassay for listeria monocytogenes by using core gold nanoparticles, silver nanoclusters as oxidase mimetics, and aptamer-conjugated magnetic nanoparticles. Microchim. Acta 2018, 185, 360.
- Cesewski, E.; Johnson, B.N. Electrochemical biosensors for pathogen detection. Biosens. Bioelectron. 2020, 159, 112214.
- Cassedy, A.; Parle-McDermott, A.; O’Kennedy, R. Virus detection: A review of the current and emerging molecular and immunological methods. Front. Mol. Biosci. 2021, 76, 637559.
- Alahi, M.E.E.; Mukhopadhyay, S.C. Detection methodologies for pathogen and toxins: A review. Sensors 2017, 17, 1885.
- Lazcka, O.; Del Campo, F.J.; Munoz, F.X. Pathogen detection: A perspective of traditional methods and biosensors. Biosens. Bioelectron. 2007, 22, 1205–1217.
- Zhao, G.; Xing, F.; Deng, S. A disposable amperometric enzyme immunosensor for rapid detection of vibrio parahaemolyticus in food based on agarose/nano-au membrane and screen-printed electrode. Electrochem. Commun. 2007, 9, 1263–1268.
- Law, J.W.-F.; Ab Mutalib, N.-S.; Chan, K.-G.; Lee, L.-H. Rapid methods for the detection of foodborne bacterial pathogens: Principles, applications, advantages and limitations. Front. Microbiol. 2015, 5, 770.
- Klein, D. Quantification using real-time pcr technology: Applications and limitations. Trends Mol. Med. 2002, 8, 257–260.
- Malorny, B.; Tassios, P.T.; Rådström, P.; Cook, N.; Wagner, M.; Hoorfar, J. Standardization of diagnostic pcr for the detection of foodborne pathogens. Int. J. Food Microbiol. 2003, 83, 39–48.
- Yang, S.; Rothman, R.E. Pcr-based diagnostics for infectious diseases: Uses, limitations, and future applications in acute-care settings. Lancet Infect. Dis. 2004, 4, 337–348.
- Zeng, D.; Chen, Z.; Jiang, Y.; Xue, F.; Li, B. Advances and challenges in viability detection of foodborne pathogens. Front. Microbiol. 2016, 7, 1833.
- Czajka, J.; Bsat, N.; Piani, M.; Russ, W.; Sultana, K.; Wiedmann, M.; Whitaker, R.; Batt, C. Differentiation of listeria monocytogenes and listeria innocua by 16s rrna genes and intraspecies discrimination of listeria monocytogenes strains by random amplified polymorphic DNA polymorphisms. Appl. Environ. Microbiol. 1993, 59, 304–308.
- Hansen, B.M.; Hendriksen, N.B. Detection of enterotoxic bacillus cereus and bacillus thuringiensis strains by pcr analysis. Appl. Environ. Microbiol. 2001, 67, 185–189.
- Kim, S.-O.; Kim, S.-S. Bacterial pathogen detection by conventional culture-based and recent alternative (polymerase chain reaction, isothermal amplification, enzyme linked immunosorbent assay, bacteriophage amplification, and gold nanoparticle aggregation) methods in food samples: A review. J. Food Saf. 2021, 41, e12870.
- Sakamoto, S.; Putalun, W.; Vimolmangkang, S.; Phoolcharoen, W.; Shoyama, Y.; Tanaka, H.; Morimoto, S. Enzyme-linked immunosorbent assay for the quantitative/qualitative analysis of plant secondary metabolites. J. Nat. Med. 2018, 72, 32–42.
- Justino, C.I.; Duarte, A.C.; Rocha-Santos, T.A. Recent progress in biosensors for environmental monitoring: A review. Sensors 2017, 17, 2918.
- Scognamiglio, V.; Rea, G.; Arduini, F.; Palleschi, G. Biosensors for Sustainable Food-New Opportunities and Technical Challenges; Elsevier: Amsterdam, The Netherlands, 2016.
- Sin, M.L.; Mach, K.E.; Wong, P.K.; Liao, J.C. Advances and challenges in biosensor-based diagnosis of infectious diseases. Expert Rev. Mol. Diagn. 2014, 14, 225–244.
- Clark, K.D.; Zhang, C.; Anderson, J.L. Sample Preparation for Bioanalytical and Pharmaceutical Analysis; ACS Publications: Washington, DC, USA, 2016.
- Silverman, J.D.; Bloom, R.J.; Jiang, S.; Durand, H.K.; Mukherjee, S.; David, L.A. Measuring and mitigating pcr bias in microbiome data. PLoS Comput. Biol. 2021, 17, e1009113.
- Thévenot, D.R.; Toth, K.; Durst, R.A.; Wilson, G.S. Electrochemical biosensors: Recommended definitions and classification. Biosens. Bioelectron. 2001, 16, 121–131.
- Ferrari, A.G.-M.; Crapnell, R.D.; Banks, C.E. Electroanalytical overview: Electrochemical sensing platforms for food and drink safety. Biosensors 2021, 11, 291.
- Daniels, J.S.; Pourmand, N. Label-free impedance biosensors: Opportunities and challenges. Electroanal. Int. J. Devoted Fundam. Pract. Asp. Electroanal. 2007, 19, 1239–1257.
- Rapp, B.E.; Gruhl, F.J.; Länge, K. Biosensors with label-free detection designed for diagnostic applications. Anal. Bioanal. Chem. 2010, 398, 2403–2412.
- Sang, S.; Wang, Y.; Feng, Q.; Wei, Y.; Ji, J.; Zhang, W. Progress of new label-free techniques for biosensors: A review. Crit. Rev. Biotechnol. 2016, 36, 465–481.
- Vestergaard, M.; Kerman, K.; Tamiya, E. An overview of label-free electrochemical protein sensors. Sensors 2007, 7, 3442–3458.
- Resch-Genger, U.; Grabolle, M.; Cavaliere-Jaricot, S.; Nitschke, R.; Nann, T. Quantum dots versus organic dyes as fluorescent labels. Nat. Methods 2008, 5, 763–775.
- Cooper, M.A. Label-Free Biosensors: Techniques and Applications; Cambridge University Press: Cambridge, UK, 2009.
- Syahir, A.; Usui, K.; Tomizaki, K.-y.; Kajikawa, K.; Mihara, H. Label and label-free detection techniques for protein microarrays. Microarrays 2015, 4, 228–244.
- Yoo, S.M.; Lee, S.Y. Optical biosensors for the detection of pathogenic microorganisms. Trends Biotechnol. 2016, 34, 7–25.
- Felix, F.S.; Angnes, L. Electrochemical immunosensors–a powerful tool for analytical applications. Biosens. Bioelectron. 2018, 102, 470–478.
- Da Silva Neves, M.M.P.; González-García, M.B.; Hernandez-Santos, D.; Fanjul-Bolado, P. Future trends in the market for electrochemical biosensing. Curr. Opin. Electrochem. 2018, 10, 107–111.
- Saucedo, N.M.; Srinives, S.; Mulchandani, A. Electrochemical biosensor for rapid detection of viable bacteria and antibiotic screening. J. Anal. Test. 2019, 3, 117–122.
- Amiri, M.; Bezaatpour, A.; Jafari, H.; Boukherroub, R.; Szunerits, S. Electrochemical methodologies for the detection of pathogens. ACS Sens. 2018, 3, 1069–1086.
- Duffy, G.; Moore, E. Electrochemical immunosensors for food analysis: A review of recent developments. Anal. Lett. 2017, 50, 1–32.
- Furst, A.L.; Francis, M.B. Impedance-based detection of bacteria. Chem. Rev. 2018, 119, 700–726.
- Mishra, G.K.; Sharma, V.; Mishra, R.K. Electrochemical aptasensors for food and environmental safeguarding: A review. Biosensors 2018, 8, 28.
- Monzó, J.; Insua, I.; Fernandez-Trillo, F.; Rodriguez, P. Fundamentals, achievements and challenges in the electrochemical sensing of pathogens. Analyst 2015, 140, 7116–7128.
- Chin, S.F.; Lim, L.S.; Pang, S.C.; Sum, M.S.H.; Perera, D. Carbon nanoparticle modified screen printed carbon electrode as a disposable electrochemical immunosensor strip for the detection of japanese encephalitis virus. Microchim. Acta 2017, 184, 491–497.
- Bhardwaj, J.; Devarakonda, S.; Kumar, S.; Jang, J. Development of a paper-based electrochemical immunosensor using an antibody-single walled carbon nanotubes bio-conjugate modified electrode for label-free detection of foodborne pathogens. Sens. Actuators B Chem. 2017, 253, 115–123.
- Mathelié-Guinlet, M.; Cohen-Bouhacina, T.; Gammoudi, I.; Martin, A.; Beven, L.; Delville, M.-H.; Grauby-Heywang, C. Silica nanoparticles-assisted electrochemical biosensor for the rapid, sensitive and specific detection of escherichia coli. Sens. Actuators B Chem. 2019, 292, 314–320.
- Zhang, Q.; Li, L.; Qiao, Z.; Lei, C.; Fu, Y.; Xie, Q.; Yao, S.; Li, Y.; Ying, Y. Electrochemical conversion of Fe3O4 magnetic nanoparticles to electroactive prussian blue analogues for self-sacrificial label biosensing of avian influenza virus h5n1. Anal. Chem. 2017, 89, 12145–12151.
- Hai, W.; Goda, T.; Takeuchi, H.; Yamaoka, S.; Horiguchi, Y.; Matsumoto, A.; Miyahara, Y. Specific recognition of human influenza virus with pedot bearing sialic acid-terminated trisaccharides. ACS Appl. Mater. Interfaces 2017, 9, 14162–14170.
- Chand, R.; Neethirajan, S. Microfluidic platform integrated with graphene-gold nano-composite aptasensor for one-step detection of norovirus. Biosens. Bioelectron. 2017, 98, 47–53.
- Abbaspour, A.; Norouz-Sarvestani, F.; Noori, A.; Soltani, N. Aptamer-conjugated silver nanoparticles for electrochemical dual-aptamer-based sandwich detection of staphylococcus aureus. Biosens. Bioelectron. 2015, 68, 149–155.
- Idil, N.; Hedström, M.; Denizli, A.; Mattiasson, B. Whole cell based microcontact imprinted capacitive biosensor for the detection of escherichia coli. Biosens. Bioelectron. 2017, 87, 807–815.
- Nahhas, A.F.; Nahhas, A.F.; Webster, T.J. Nanoscale pathogens treated with nanomaterial-like peptides: A platform technology appropriate for future pandemics. Nanomedicine 2021, 16, 1237–1254.
- Huang, C.; Zhao, J.; Lu, R.; Wang, J.; Nugen, S.R.; Chen, Y.; Wang, X. A phage-based magnetic relaxation switching biosensor using bioorthogonal reaction signal amplification for salmonella detection in foods. Food Chem. 2023, 400, 134035.
- Wang, J.; Li, H.; Li, C.; Ding, Y.; Wang, Y.; Zhu, W.; Wang, J.; Shao, Y.; Pan, H.; Wang, X. Eis biosensor based on a novel myoviridae bacteriophage sep37 for rapid and specific detection of salmonella in food matrixes. Food Res. Int. 2022, 158, 111479.
- Radke, S.M.; Alocilja, E.C. A high density microelectrode array biosensor for detection of E. Coli O157: H7. Biosens. Bioelectron. 2005, 20, 1662–1667.
- Sharma, M.; Goel, A.; Singh, L.; Rao, V. Immunological biosensor for detection of vibrio cholerae o1in environmental water samples. World J. Microbiol. Biotechnol. 2006, 22, 1155–1159.
- Wang, R.; Ruan, C.; Kanayeva, D.; Lassiter, K.; Li, Y. Tio2 nanowire bundle microelectrode based impedance immunosensor for rapid and sensitive detection of listeria monocytogenes. Nano Lett. 2008, 8, 2625–2631.
- Das, R.D.; RoyChaudhuri, C.; Maji, S.; Das, S.; Saha, H. Macroporous silicon based simple and efficient trapping platform for electrical detection of salmonella typhimurium pathogens. Biosens. Bioelectron. 2009, 24, 3215–3222.
- Nguyen, B.T.; Koh, G.; Lim, H.S.; Chua, A.J.; Ng, M.M.; Toh, C.-S. Membrane-based electrochemical nanobiosensor for the detection of virus. Anal. Chem. 2009, 81, 7226–7234.
- Pal, S.; Alocilja, E.C. Electrically active polyaniline coated magnetic (eapm) nanoparticle as novel transducer in biosensor for detection of bacillus anthracis spores in food samples. Biosens. Bioelectron. 2009, 24, 1437–1444.
- Huang, J.; Yang, G.; Meng, W.; Wu, L.; Zhu, A. An electrochemical impedimetric immunosensor for label-free detection of campylobacter jejuni in diarrhea patients’ stool based on o-carboxymethylchitosan surface modified Fe3O4 nanoparticles. Biosens. Bioelectron. 2010, 25, 1204–1211.
- Luo, Y.; Nartker, S.; Miller, H.; Hochhalter, D.; Wiederoder, M.; Wiederoder, S.; Setterington, E.; Drzal, L.T.; Alocilja, E.C. Surface functionalization of electrospun nanofibers for detecting E. Coli O157: H7 and bvdv cells in a direct-charge transfer biosensor. Biosens. Bioelectron. 2010, 26, 1612–1617.
- Mannoor, M.S.; Tao, H.; Clayton, J.D.; Sengupta, A.; Kaplan, D.L.; Naik, R.R.; Verma, N.; Omenetto, F.G.; McAlpine, M.C. Graphene-based wireless bacteria detection on tooth enamel. Nat. Commun. 2012, 3, 763.
- Tolba, M.; Ahmed, M.U.; Tlili, C.; Eichenseher, F.; Loessner, M.J.; Zourob, M. A bacteriophage endolysin-based electrochemical impedance biosensor for the rapid detection of listeria cells. Analyst 2012, 137, 5749–5756.
- Samardzic, R.; Sussitz, H.F.; Jongkon, N.; Lieberzeit, P.A. Quartz crystal microbalance in-line sensing of Escherichia coli in a bioreactor using molecularly imprinted polymers. Sens. Lett. 2014, 12, 1152–1155.
- Chen, G.-Z.; Yin, Z.-Z.; Lou, J.-F. Electrochemical immunoassay of Escherichia coli O157: H7 using 2 nanoparticles as labels. J. Anal. Methods Chem. 2014, 2014, 247034.
- Dastider, S.G.; Barizuddin, S.; Yuksek, N.S.; Dweik, M.; Almasri, M.F. Efficient and rapid detection of salmonella using microfluidic impedance based sensing. J. Sens. 2015, 2015, 293461.
- Andrade, C.A.; Nascimento, J.M.; Oliveira, I.S.; de Oliveira, C.V.; de Melo, C.P.; Franco, O.L.; Oliveira, M.D. Nanostructured sensor based on carbon nanotubes and clavanin a for bacterial detection. Colloids Surf. B Biointerfaces 2015, 135, 833–839.
- Luna, D.M.; Avelino, K.Y.; Cordeiro, M.T.; Andrade, C.A.; Oliveira, M.D. Electrochemical immunosensor for dengue virus serotypes based on 4-mercaptobenzoic acid modified gold nanoparticles on self-assembled cysteine monolayers. Sens. Actuators B Chem. 2015, 220, 565–572.
- Kitajima, M.; Wang, N.; Tay, M.Q.; Miao, J.; Whittle, A.J. Development of a mems-based electrochemical aptasensor for norovirus detection. Micro Nano Lett. 2016, 11, 582–585.
- Attar, A.; Mandli, J.; Ennaji, M.M.; Amine, A. Label-free electrochemical impedance detection of rotavirus based on immobilized antibodies on gold sononanoparticles. Electroanalysis 2016, 28, 1839–1846.
- Golabi, M.; Kuralay, F.; Jager, E.W.; Beni, V.; Turner, A.P. Electrochemical bacterial detection using poly (3-aminophenylboronic acid)-based imprinted polymer. Biosens. Bioelectron. 2017, 93, 87–93.
- Hai, W.; Goda, T.; Takeuchi, H.; Yamaoka, S.; Horiguchi, Y.; Matsumoto, A.; Miyahara, Y. Human influenza virus detection using sialyllactose-functionalized organic electrochemical transistors. Sens. Actuators B Chem. 2018, 260, 635–641.
- Jantra, J.; Kanatharana, P.; Asawatreratanakul, P.; Hedström, M.; Mattiasson, B.; Thavarungkul, P. Real-time label-free affinity biosensors for enumeration of total bacteria based on immobilized concanavalin a. J. Environ. Sci. Health Part A 2011, 46, 1450–1460.
- Hou, T.; Zeng, W.; Yang, M.; Chen, W.; Ren, L.; Ai, J.; Wu, J.; Liao, Y.; Gou, X.; Li, Y. Development and evaluation of a rapid crispr-based diagnostic for COVID-19. PLoS Pathog. 2020, 16, e1008705.
- Bacchu, M.S.; Ali, M.R.; Das, S.; Akter, S.; Sakamoto, H.; Suye, S.I.; Rahman, M.M.; Campbell, K.; Khan, M.Z.H. A DNA functionalized advanced electrochemical biosensor for identification of the foodborne pathogen salmonella enterica serovar typhi in real samples. Anal. Chim. Acta 2022, 1192, 339332.
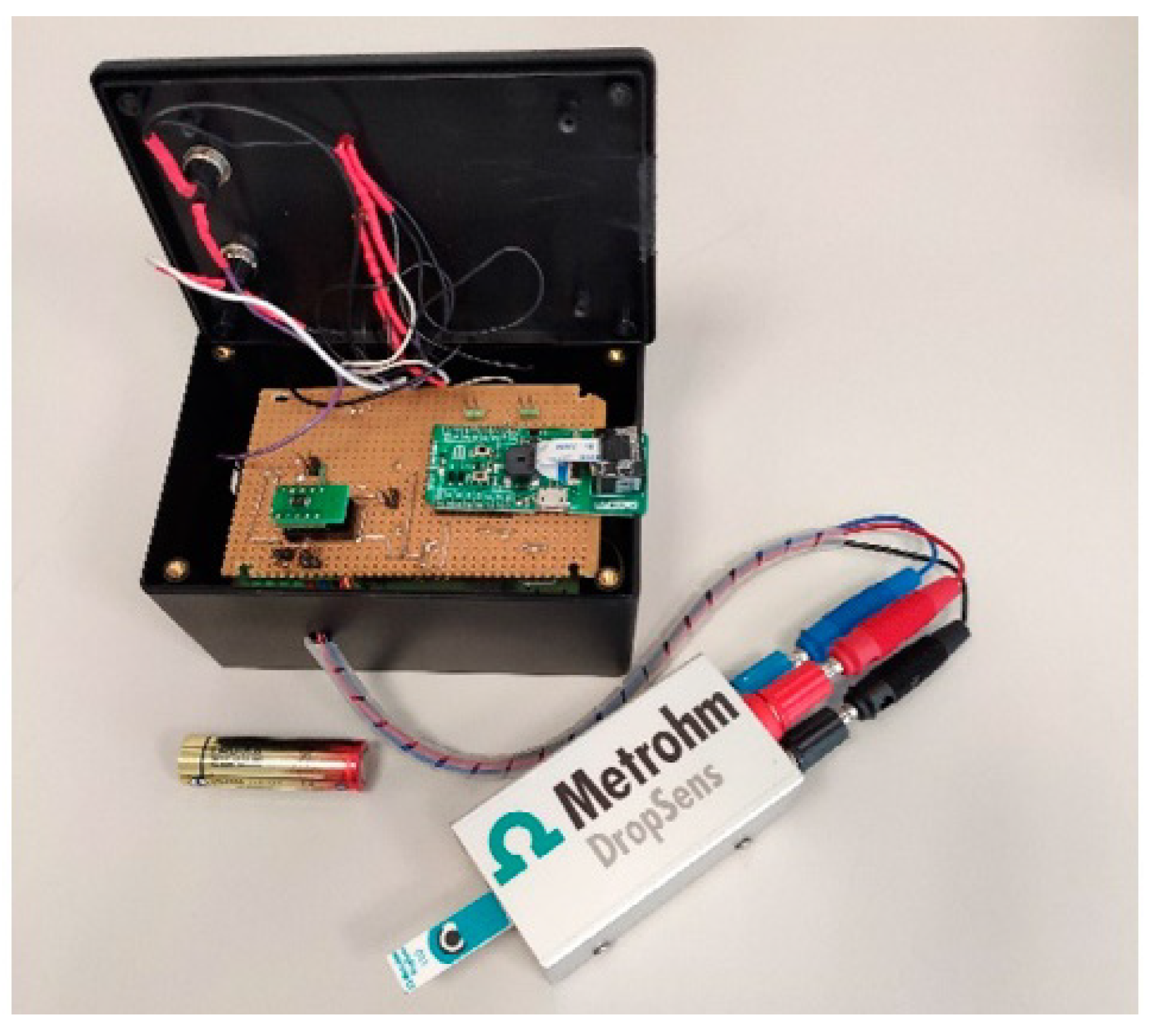
- Fortunati, S.; Giliberti, C.; Giannetto, M.; Bolchi, A.; Ferrari, D.; Donofrio, G.; Bianchi, V.; Boni, A.; De Munari, I.; Careri, M. Rapid quantification of SARS-CoV-2 spike protein enhanced with a machine learning technique integrated in a smart and portable immunosensor. Biosensors 2022, 12, 426.
- Yamanaka, K.; Vestergaard, M.d.C.; Tamiya, E. Printable electrochemical biosensors: A focus on screen-printed electrodes and their application. Sensors 2016, 16, 1761.
- Arduini, F.; Micheli, L.; Moscone, D.; Palleschi, G.; Piermarini, S.; Ricci, F.; Volpe, G. Electrochemical biosensors based on nanomodified screen-printed electrodes: Recent applications in clinical analysis. TrAC Trends Anal. Chem. 2016, 79, 114–126.
- Singh, S.; Wang, J.; Cinti, S. An overview on recent progress in screen-printed electroanalytical (bio) sensors. ECS Sens. Plus 2022, 1, 023401.
- Wang, X.; Zhang, Z.; Wu, G.; Xu, C.; Wu, J.; Zhang, X.; Liu, J. Applications of electrochemical biosensors based on functional antibody modified screen printed electrodes: A review. Anal. Methods 2021, 14, 7–16.
- Faulkner, L.R.; Bard, A.J. Electrochemical Methods: Fundamentals and Applications; John Wiley and Sons: Hoboken, NJ, USA, 2002.
- Hierlemann, A.; Brand, O.; Hagleitner, C.; Baltes, H. Microfabrication techniques for chemical/biosensors. Proc. IEEE 2003, 91, 839–863.
- Taleat, Z.; Khoshroo, A.; Mazloum-Ardakani, M. Screen-printed electrodes for biosensing: A review (2008–2013). Microchim. Acta 2014, 181, 865–891.
- Bhat, K.S.; Ahmad, R.; Yoo, J.-Y.; Hahn, Y.-B. Fully nozzle-jet printed non-enzymatic electrode for biosensing application. J. Colloid Interface Sci. 2018, 512, 480–488.
- Medina-Sánchez, M.; Martínez-Domingo, C.; Ramon, E.; Merkoçi, A. An inkjet-printed field-effect transistor for label-free biosensing. Adv. Funct. Mater. 2014, 24, 6291–6302.
- Pavinatto, F.J.; Paschoal, C.W.; Arias, A.C. Printed and flexible biosensor for antioxidants using interdigitated ink-jetted electrodes and gravure-deposited active layer. Biosens. Bioelectron. 2015, 67, 553–559.
- Foo, C.; Lim, H.; Mahdi, M. Three-dimensional printed electrode and its novel applications in electronic devices. Sci. Rep. 2018, 8, 7399.
- Loo, A.H.; Chua, C.K.; Pumera, M. DNA biosensing with 3d printing technology. Analyst 2017, 142, 279–283.
- Ambrosi, A.; Moo, J.G.S.; Pumera, M. Helical 3d-printed metal electrodes as custom-shaped 3d platform for electrochemical devices. Adv. Funct. Mater. 2016, 26, 698–703.
- Dos Santos, M.B.; Azevedo, S.; Agusil, J.; Prieto-Simón, B.; Sporer, C.; Torrents, E.; Juárez, A.; Teixeira, V.; Samitier, J. Label-free ito-based immunosensor for the detection of very low concentrations of pathogenic bacteria. Bioelectrochemistry 2015, 101, 146–152.
- Aydın, E.B.; Sezgintürk, M.K. Indium tin oxide (ito): A promising material in biosensing technology. TrAC Trends Anal. Chem. 2017, 97, 309–315.
- Yang, L.; Li, Y. Afm and impedance spectroscopy characterization of the immobilization of antibodies on indium–tin oxide electrode through self-assembled monolayer of epoxysilane and their capture of Escherichia coli O157: H7. Biosens. Bioelectron. 2005, 20, 1407–1416.
- Wenzel, T.; Härtter, D.; Bombelli, P.; Howe, C.J.; Steiner, U. Porous translucent electrodes enhance current generation from photosynthetic biofilms. Nat. Commun. 2018, 9, 1299.
- Guimard, N.K.; Gomez, N.; Schmidt, C.E. Conducting polymers in biomedical engineering. Prog. Polym. Sci. 2007, 32, 876–921.
- Arshak, K.; Velusamy, V.; Korostynska, O.; Oliwa-Stasiak, K.; Adley, C. Conducting polymers and their applications to biosensors: Emphasizing on foodborne pathogen detection. IEEE Sens. J. 2009, 9, 1942–1951.
- Kaur, G.; Adhikari, R.; Cass, P.; Bown, M.; Gunatillake, P. Electrically conductive polymers and composites for biomedical applications. RSC Adv. 2015, 5, 37553–37567.
- Terán-Alcocer, Á.; Bravo-Plascencia, F.; Cevallos-Morillo, C.; Palma-Cando, A. Electrochemical sensors based on conducting polymers for the aqueous detection of biologically relevant molecules. Nanomaterials 2021, 11, 252.
- Wang, G.; Morrin, A.; Li, M.; Liu, N.; Luo, X. Nanomaterial-doped conducting polymers for electrochemical sensors and biosensors. J. Mater. Chem. B 2018, 6, 4173–4190.
- Rahman, M.A.; Kumar, P.; Park, D.-S.; Shim, Y.-B. Electrochemical sensors based on organic conjugated polymers. Sensors 2008, 8, 118–141.
- Soylemez, S.; Kaya, H.Z.; Udum, Y.A.; Toppare, L. A multipurpose conjugated polymer: Electrochromic device and biosensor construction for glucose detection. Org. Electron. 2019, 65, 327–333.
- Pavase, T.R.; Lin, H.; Shaikh, Q.-u.-a.; Hussain, S.; Li, Z.; Ahmed, I.; Lv, L.; Sun, L.; Shah, S.B.H.; Kalhoro, M.T. Recent advances of conjugated polymer (cp) nanocomposite-based chemical sensors and their applications in food spoilage detection: A comprehensive review. Sens. Actuators B Chem. 2018, 273, 1113–1138.
- Dong, J.; Zhao, H.; Xu, M.; Ma, Q.; Ai, S. A label-free electrochemical impedance immunosensor based on aunps/pamam-mwcnt-chi nanocomposite modified glassy carbon electrode for detection of salmonella typhimurium in milk. Food Chem. 2013, 141, 1980–1986.
- Lee, D.; Chander, Y.; Goyal, S.M.; Cui, T. Carbon nanotube electric immunoassay for the detection of swine influenza virus h1n1. Biosens. Bioelectron. 2011, 26, 3482–3487.
- Li, Y.; Cheng, P.; Gong, J.; Fang, L.; Deng, J.; Liang, W.; Zheng, J. Amperometric immunosensor for the detection of Escherichia Coli O157: H7 in food specimens. Anal. Biochem. 2012, 421, 227–233.
- Viswanathan, S.; Rani, C.; Ho, J.-a.A. Electrochemical immunosensor for multiplexed detection of food-borne pathogens using nanocrystal bioconjugates and mwcnt screen-printed electrode. Talanta 2012, 94, 315–319.
- Tamara, F.R.; Lin, C.; Mi, F.-L.; Ho, Y.-C. Antibacterial effects of chitosan/cationic peptide nanoparticles. Nanomaterials 2018, 8, 88.
- Xu, M.; Obodo, D.; Yadavalli, V.K. The design, fabrication, and applications of flexible biosensing devices. Biosens. Bioelectron. 2019, 124, 96–114.
- Kong, Y.L.; Tamargo, I.A.; Kim, H.; Johnson, B.N.; Gupta, M.K.; Koh, T.-W.; Chin, H.-A.; Steingart, D.A.; Rand, B.P.; McAlpine, M.C. 3d printed quantum dot light-emitting diodes. Nano Lett. 2014, 14, 7017–7023.
- Liu, S.; He, P.; Hussain, S.; Lu, H.; Zhou, X.; Lv, F.; Liu, L.; Dai, Z.; Wang, S. Conjugated polymer-based photoelectrochemical cytosensor with turn-on enable signal for sensitive cell detection. ACS Appl. Mater. Interfaces 2018, 10, 6618–6623.
- Kim, J.; Campbell, A.S.; de Ávila, B.E.-F.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406.
- Mohankumar, P.; Ajayan, J.; Mohanraj, T.; Yasodharan, R. Recent developments in biosensors for healthcare and biomedical applications: A review. Measurement 2021, 167, 108293.
- Lee, Y.; Kim, J.; Joo, H.; Raj, M.S.; Ghaffari, R.; Kim, D.H. Wearable sensing systems with mechanically soft assemblies of nanoscale materials. Adv. Mater. Technol. 2017, 2, 1700053.
- Cesewski, E.; Haring, A.P.; Tong, Y.; Singh, M.; Thakur, R.; Laheri, S.; Read, K.A.; Powell, M.D.; Oestreich, K.J.; Johnson, B.N. Additive manufacturing of three-dimensional (3d) microfluidic-based microelectromechanical systems (mems) for acoustofluidic applications. Lab A Chip 2018, 18, 2087–2098.
- Xu, Y.; Wu, X.; Guo, X.; Kong, B.; Zhang, M.; Qian, X.; Mi, S.; Sun, W. The boom in 3d-printed sensor technology. Sensors 2017, 17, 1166.
- Varshney, M.; Li, Y. Interdigitated array microelectrodes based impedance biosensors for detection of bacterial cells. Biosens. Bioelectron. 2009, 24, 2951–2960.
- Yang, L.; Li, Y. Detection of viable salmonella using microelectrode-based capacitance measurement coupled with immunomagnetic separation. J. Microbiol. Methods 2006, 64, 9–16.
- Yang, H.; Rahman, M.T.; Du, D.; Panat, R.; Lin, Y. 3-d printed adjustable microelectrode arrays for electrochemical sensing and biosensing. Sens. Actuators B Chem. 2016, 230, 600–606.
