Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Biology
Periprosthetic joint infection (PJI) is a major adverse event of primary total knee arthroplasty (TKA) from the patient’s perspective, and it is also costly for health care systems. Knowing the risk factors for PJI after TKA, especially those that are avoidable or controllable, is critical to minimizing (ideally preventing) this complication.
- periprosthetic joint infection
- risk factors
- total knee arthroplasty
1. Introduction
According to Carulli et al., total knee arthroplasty (TKA) is one of the most successful surgical techniques in orthopedic surgery, with good clinical outcomes and a high survival percentage of more than 90% of cases at long-term follow-up. The increasing mean population age, worsening of joint degenerative disorders, and joint sequelae related to previous fractures have caused a continuous rise in the number of TKAs in every country annually, along with an expected increase in adverse events [1]. A frequent cause of revision TKA following primary TKA is periprosthetic joint infection (PJI) [2,3,4,5,6]. PJI was published by the Musculoskeletal Infection Society (MSIS) in 2011 [7] (Table 1).
Table 1. MSIS definition of PJI [7].
| PJI Exists When | |
|---|---|
| 1 | There is a sinus tract communicating with the implant; or |
| 2 | A bacterium is isolated by culture from 2 or more separate tissue or fluid samples attained from the affected knee; or |
| 3 | When 4 of the following 6 criteria exist:
|
In 2018, Parvizi et al. reported an evidence-based definition for knee PJI that has demonstrated very good performance on formal external validation [8]. Two positive cultures or the existence of a sinus tract were deemed primary factors and diagnostic of PJI. The estimated weights of increased serum C-reactive protein (CRP) (>1 mg/dL), D-dimer (>860 ng/mL), and erythrocyte sedimentation rate (ESR) (>30 mm/h) were 2, 2, and 1 point, respectively. Moreover, increased synovial fluid white blood cell count (>3000 cells/μL), alpha-defensin (signal-to-cutoff ratio > 1), leukocyte esterase (++), polymorphonuclear percentage (>80%), and synovial CRP (>6.9 mg/L) were given 3, 3, 3, 2, and 1 point, respectively. Individuals with a total score of greater than or equal to 6 were deemed infected, whereas a score between 2 and 5 needed the addition of intraoperative findings for proving or disproving the diagnosis. Intraoperative findings of positive histology, purulence, and single positive culture were given 3, 3, and 2 points, respectively. Put together with the preoperative score, an aggregate of greater than or equal to 6 was deemed infected, a score between 4 and 5 was uncertain, and a score of 3 or less was not infected. These standards showed a greater sensitivity of 97.7% compared with the MSIS (79.3%) and the International Consensus Meeting definition (86.9%), with an akin specificity of 99.5% [8].
In 2021, McNally et al. reported the result of a plan created by the European Bone and Joint Infection Society (EBJIS) and endorsed by the MSIS and the European Society of Clinical Microbiology and Infectious Diseases Study Group for Implant-Associated Infections (ESGIAI). McNally et al. defined PJI using a three-degree method to the diagnostic sequence, leading to a definition set and guidance that was fully backed by the EBJIS, MSIS, and ESGIAI [9]. There are three possibilities: infection unlikely, infection likely, and infection established based on the following data: clinical and blood workup (clinical features, CRP); synovial fluid cytological analysis (leukocyte count (cells/µL); polymorphonuclear percentage); synovial fluid biomarkers (alpha-defensin); microbiology (aspiration fluid, intraoperative fluid and tissue, sonication (CFU/mL); and histology (high-power field, 400× magnification). This new EBJIS definition can now be used worldwide [9].
PJI is a severe complication of primary TKA from the patient’s perspective, and it is also very costly for health care systems [10]. In fact, PJI is one of the most overwhelming adverse events of TKA [11].
Although one-stage revision TKA is performed in certain situations and centers, a PJI usually requires a two-stage revision TKA, which involves a double surgical intervention. First, the removal of the infected implant (septic loosening) is required. Following this procedure, a period of several weeks of antibiotic treatment is needed until the infection is considered cured (normalization of the ESR and CRP and healing of the surgical wound). The second intervention is the insertion of a new implant, using a model that is stable for proper functioning of the knee [11]. Figure 1 shows a case of PJI (septic loosening) that was solved by a two-stage revision TKA.
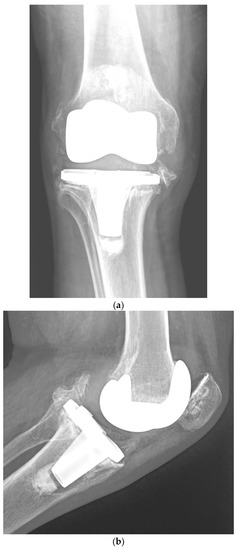


Figure 1. (a–d). Periprosthetic joint infection of a primary total knee arthroplasty (TKA) that was resolved by a two-stage revision TKA: (a) preoperative anteroposterior (AP) radiograph; (b) preoperative lateral image; (c) postoperative AP radiograph showing the prosthesis implanted in the second-stage revision (rotational hinge design); (d) lateral image of the aforementioned prosthesis.
It is important to emphasize that debridement, antibiotics, and implant retention (DAIR) is today a frequently utilized procedure in early infections [12,13,14,15,16]. Toh et al. reported that DAIR is the procedure of preference for individuals with acute postoperative and acute hematogenous PJI [15]. They stated that DAIR failure was related to premature mortality. Repeated DAIRs, increased ESR > 107.5, and S. aureus PJI were related to treatment failure, and two-stage revision TKA was advised. It is also relevant to remark that the likelihood of PJI after primary TKA can be reduced by decreasing the patient’s weight, which will also minimize the risk of implant failure [17].
2. Risk Factors for Periprosthetic Joint Infection following Primary TKA
2.1. Patient-Related Risk Factors
2.1.1. Male Gender, Procedure Type (bilateral), Length of Stay over 35 Days, and Usage of Transfusions Have Been Shown to Be Risk Factors for Postoperative PJI
In 2021, Ko et al. found that male sex, low family earnings, surgical technique type (bilateral), length of stay (LOS) ≥ 35 days, and transfusions were risk factors for postoperative adverse events after TKA in individuals with idiopathic knee osteoarthritis. The aforementioned authors analyzed 560,954 individuals older than 50 years. The risk of PJI was evaluated with 8 independent parameters: sex, age, place of residence, family earnings, hospital bed size, type of surgical technique (unilateral or bilateral, primary or revision TKA), LOS, and the use of transfusions [21].
2.1.2. Male Gender, Younger Age, Type II Diabetes, Posttraumatic Osteoarthritis, Patellar Resurfacing, and Discharge to Nursing Home Were Related to an Increased Risk of PJI
In 2022, the MAC carried a population-based cohort investigation utilizing linked administrative databases. The multivariable analysis showed that male gender, younger age, type II diabetes, posttraumatic osteoarthritis, patellar resurfacing, and discharge to convalescent care were related to an increased risk of PJI [11].
In an article with level 2 evidence (prognostic study), the independent risk factors for PJI (in diminishing order of importance) were congestive heart failure, chronic pulmonary illness, preoperative anemia, diabetes, depression, renal illness, pulmonary circulation disorders, obesity, rheumatologic illness, psychoses, metastatic tumor, peripheral vascular illness, and valvular illness [22].
In 2013, Chen et al. showed that the principal factors associated with PJI following TKA were body mass index (BMI), diabetes mellitus, hypertension, steroid treatment, and rheumatoid arthritis. The study had insufficient evidence to demonstrate that the male sex was associated with PJI after TKA. A statistical analysis showed no correlations between urinary tract infection, fixation technique, American Society of Anesthesiology (ASA) score, bilateral procedure, age, transfusion, antibiotics, bone graft, and PJI [23].
A study with level 2 evidence (prognostic study) reported by Kurtz et al. in 2010 showed that women had a lower risk of PJI than men. Comorbidities also increased TKA infection risk. Individuals receiving public assistance for Medicare premiums were at increased risk for PJI. Hospital factors did not contribute to an increased risk of infection. PJI occurred at a fairly elevated percentage in Medicare individuals, with the greatest risk of PJI within the first 2 years following TKA; nonetheless, around 25% of all PJIs occurred after 2 years [20].
Cordtz et al. observed that individuals with rheumatoid arthritis had a diminished 10-year risk of revision TKA, whereas the risk of PJI was increased compared with individuals with osteoarthritis after TKA. Previous treatment with biological disease-modifying antirheumatic drugs was not related to an increased risk of PJI [24].
In an investigation with level 3 evidence (therapeutic study), Pancio et al. found that a higher proportion of individuals who had undergone multi-ligament knee surgery experienced infections compared with matched controls (7% vs. 1%), respectively. Previous multi-ligament surgery was associated with a greater risk of PJI [25].
2.1.3. Previous Septic Arthritis Has Been Shown to Be a Risk Factor for Postoperative PJI
Previous septic arthritis has also been recognized as a PJI risk factor [25]. Pooled data from more than 1300 arthroplasties in published papers revealed a PJI rate of 5.96% when a previous infection occurred in the same articulation. The risk of infection was lower because the TKA surgery was delayed from the resolution of the previous infection.
2.1.4. Smoking Is related to Higher Percentages of PJI
In 2015, Singh et al. found that smoking was related to an elevated risk of PJI after primary TKA. Tobacco use status was accessible for 7926 (95%) individuals and was not accessible for 446 (5%); 565 (7%) currently smoked tobacco. The hazard ratios for PJI were higher in current tobacco users than in nonusers [26]. Cessation of smoking before TKA is strongly recommended.
2.1.5. Hypoalbuminemia and Obesity Class II Are Dependable Predictors of PJI
According to Man et al., malnutrition is a relevant but changeable risk factor for postoperative adverse events and unfavorable results in orthopedic surgery [27]. They sought to detect biomarkers of malnutrition in individuals undergoing TKA that could be predictive of adverse postoperative complications in the hospital, to identify patients at risk and optimize their nutritional status prior to TKA. These authors analyzed 624 patients in whom possible biomarkers of pre-operative malnutrition, including hypoalbuminemia (serum albumin < 3.5 g/dL), total lymphocyte count (TLC) (<1500 cells/mm3), and BMI, were evaluated for associations with in-hospital postoperative adverse events. The frequencies of hypoalbuminemia, low TLC, overweight, obesity class I, and obesity class II were 2.72%, 33.4%, 14.8%, 44.5%, and 26.9%, respectively. There were significant relationships between hypoalbuminemia and type II obesity (BMI ≥ 30.0 kg/m2) and PJI percentages and no significant relationships between these adverse events and low TLC, overweight, or type I obesity. It was also found that individuals with hypoalbuminemia or type II obesity with gouty arthritis were more prone to experience PJI. The authors concluded that hypoalbuminemia and type II obesity together were dependable biomarkers of preoperative malnutrition that could predict PJI following TKA; however, low TLC, overweight, and type I obesity were not significantly related to an increased risk of PJI [27].
2.1.6. Intra-Articular Injections Prior to TKA Are Related to a Higher Risk of PJI
In a level 3 evidence study (therapeutic study) published in 2017, Bedard et al. observed that intra-articular knee injections with corticosteroids, hyaluronic acid, or other drugs prior to TKA were related to an increased risk of PJI, and this association appeared to be time dependent: the shorter the delay between injection and TKA, the greater the likelihood of PJI [28]. The proportion of patients undergoing TKAs who developed PJI was greater in those who were given an injection prior to TKA than in those who were not (4.4% vs. 3.6%). Similarly, the proportion of patients undergoing TKAs who developed PJI requiring surgical reintervention was also greater among those who received an injection prior to TKA than in those who did not (1.49% vs. 1.04%). An analysis of the months between injection and TKA showed that the odds of PJI were greater for patients injected up to 6 months between injection and TKA, as were the odds of surgical intervention for TKA infection when the injection was within 7 months of TKA. When the time span between injection and TKA was longer than 6–7 months, the ORs were no longer raised [28].
2.1.7. Greater Glucose Variability in the Postoperative Period Is Related to Higher Percentages of PJI
In 2018, Shohat et al. investigated the relationship between glucose variability and postoperative adverse events after TKA (level 4 of evidence study) [29]. They analyzed data on 2698 individuals who had experienced TKA at a single center. Individuals with a minimum of two postoperative glucose values per day or more than three values overall were included in the research. Glucose variability was evaluated utilizing a coefficient of variation. The MSIS criteria were utilized to establish PJI. Some 19.9% of the patients had diabetes. Greater glycemic variability was related to increased LOS, 90-day mortality, PJI, and SSI. Adjusted analyses showed that for every 10-percentage-point rise in the coefficient of variation, the LOS increased by 6.1%, and the risks of PJI and SSI increased by 20% and 14%, respectively. These associations were independent of the year of the surgical procedure, age, BMI, Elixhauser comorbidity index, diagnosis of diabetes, in-hospital utilization of insulin or steroids, or mean glucose values throughout hospitalization. They concluded that greater glucose variability in the postoperative period was related to increased percentages of SSI and PJI after TKA. According to Shohat et al., it is paramount to control glucose variability in the early postoperative phase [29].
2.1.8. Reduction of Patient’s Weight Diminishes the Probability of PJI and Minimizes Implant Failure
It has been published that the likelihood of PJI following primary TKA can be reduced by decreasing the patient’s weight, which will also minimize the risk of implant failure [17].
This entry is adapted from the peer-reviewed paper 10.3390/jcm11206128
This entry is offline, you can click here to edit this entry!
