Extracellular vesicles (EVs) are nanoscale vesicles secreted by most types of cells as natural vehicles to transfer molecular information between cells. Due to their low toxicity and high biocompatibility, EVs have attracted increasing attention as drug delivery systems. We summarize the techniques and methods to increase EV yield, enhance nucleic acid loading efficiency, extend circulation time, and improve targeted delivery.
- extracellular vesicles
- engineering
- cancer therapy
1. Introduction
Cancer is one of the most significant burdens a person can bear. Cancer is responsible for one out of every six deaths worldwide, according to the World Health Organization [1]. Most traditional antitumor small molecule chemotherapeutics and antibody drugs work by binding to target proteins, but the druggability of the target proteins limits their development. Only 3000 of the roughly 20,000 proteins encoded by the human genome are druggable, and only 700 have corresponding drugs in development [2,3]. Nucleic acid drugs can modulate extracellular and cell membrane proteins, whereas antibody drugs only act on cell membranes and extracellular proteins.
Cancer is caused by changes in genetic material, such as genetic mutations and chromosomal aberrations, which eventually lead to continued proliferation and metastasis. Nucleic acid drug therapy can begin at the source of the disease by exogenously introducing the therapeutic genes into diseased cells, correcting the disease caused by gene defect and abnormality, and achieving a therapeutic effect on the tumor [4]. Gene drugs can achieve breakthroughs in difficult-to-make protein targets and have a high potential for developing drugs for “untargetable” and “undruggable” diseases [5].
Extracellular vesicles (EVs), which are cell-derived, phospholipid-based bilayer membrane particles, are considered potential bioderived nanocarriers. Compared with synthetic lipid nanoparticles, EVs have natural biological advantages: low toxicity, low immunogenicity, exudation in tissues, ability to cross biological barriers, targeting of specific cell types, easy fusion with cell membranes, and ability to achieve endo/lysosomal escape. Moreover, nucleic acid drugs loaded in EVs are naturally protected from circulation degradation, which is a major advantage of EVs as drug delivery systems (DDS) [6-8].
2. EVs as Nucleic Acid Drug Delivery Vehicles
The International Society for Extracellular Vesicles (ISEV) is a professional social group composed of researchers and scientists in the field of EVs. It is committed to promoting global EV research and is one of the most authoritative societies in the field of EVs. As defined by the ISEV, EVs are the general term for particles that are naturally released from cells, which are separated by lipid bilayers and cannot replicate, i.e., do not contain a functional nucleus [9]. They can be endosome-derived (termed exosomes, diameter 30~150 nm) or are generated by membrane outward budding (termed ectosomes, diameter 50~1000 nm) [10]. Based on this, EVs can be applied in targeted therapy, cell-free therapy, and drug delivery systems [11,12].
Many types of cells are suitable for producing EVs based on their natural properties. Stem cells are favored for their high safety and high EV secretion and have been used in clinical studies [13]. However, as a drug delivery system, the following aspects still need to be considered: (1) EV secretion varies widely among different cell types and subpopulations [14] and may be further influenced by cell state and growth conditions [15]. Since various types of cells can generate EVs in response to endogenous or exogenous stimuli, how to improve the production of EVs is a key step for the widespread application and industrialization of EVs as DDS [16]. (2) Improving the encapsulation rate of nucleic acid drugs is also a consideration for realizing industrialization. (3) Although EVs themselves can circumvent the clearance of the mononuclear phagocytic system to a certain extent (clearing circulating particles larger than 100 nm), engineering modifications are required to maximize their circulation time and emphasize their advantages in intercellular communication [17]. (4) The different characteristics of EV producers and target cells may lead to significant differences in the efficiency of cell-to-cell communication. The efficiency of cellular uptake may be affected by surface-specific proteins, lipopolysaccharide decoration, and the overall potential (usually negative charge) of EVs. Therefore, targeting modifications for EVs have been extensively studied [18,19]. Given the foregoing, it is critical to design EVs to improve the efficiency and quality of nucleic acid drug delivery vehicles.
3. Improvements in EV Drug Delivery Systems
EVs are nano-scale vesicles with surfaces composed of a heterogeneous mixture of lipids and proteins, and naturally have the advantages of stealth, biocompatibility, and intrinsic homing ability. Although natural EVs already have certain targeting, long-term circulation, and cell entry capabilities, researchers are not limited to using natural EVs but intend to engineer them for better effects [5,20,21]. Here, we discuss improvement strategies according to the following four purposes (Figure 1): (A) to increase EV production; (B) to improve nucleic acid drug loading efficiency; (C) to extend circulation time; (D) to improve targeting capability and introduce corresponding modification methods (Table 1). At the end of this section, we compare the advantages and disadvantages of various strategies for modification purposes (Figure 2).
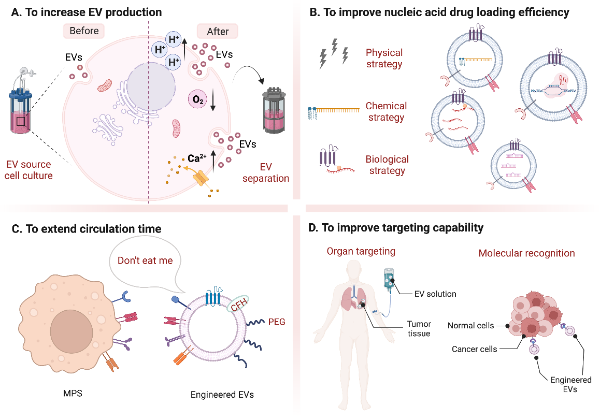
Figure 1. Summary of different modification strategies for EVs. (Created with BioRender.com, accessed on 23 August 2022).
4. Conclusions and Research Prospects
Currently, the application of EVs is facing the following questions: (1) Quality control is a problem. (2) The drug loading rate is still not ideal. (3) Stability is difficult to guarantee. (4) Metabolism and dynamics tracking are difficult to achieve.
In the future, commercial EV production requires stricter GMP specifications, including the selection of EV sources, standardized cell culture techniques, downstream EV isolation, purification, and quality assessment protocols, EV detection and tracking, and the stability of EV-based preparations [22].
References
1. Global cancer facts reported from the WHO. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cancer (accessed on 25 August 2022).
2. Overington, J.P.; Al-Lazikani, B.; Hopkins, A.L. Opinion - How many drug targets are there? Nature Reviews Drug Discovery 2006, 5, 993-996, https://doi.org/10.1038/nrd2199.
3. Warner, K.D.; Hajdin, C.E.; Weeks, K.M. Principles for targeting RNA with drug-like small molecules. Nat Rev Drug Discov 2018, 17, 547-558, https://doi.org/10.1038/nrd.2018.93.
4. Tan, A.; Rajadas, J.; Seifalian, A.M. Exosomes as nano-theranostic delivery platforms for gene therapy. Advanced Drug Delivery Reviews 2013, 65, 357-367, https://doi.org/10.1016/j.addr.2012.06.014.
5. Xue, V.W.; Wong, S.C.C.; Song, G.; Cho, W.C.S. Promising RNA-based cancer gene therapy using extracellular vesicles for drug delivery. Expert Opin Biol Ther 2020, 20, 767-777, https://doi.org/10.1080/14712598.2020.1738377.
6. Alvarez-Erviti, L.; Seow, Y.Q.; Yin, H.F.; Betts, C.; Lakhal, S.; Wood, M.J.A. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nature Biotechnology 2011, 29, 341-U179, https://doi.org/10.1038/nbt.1807.
7. Tarasov, V.V.; Svistunov, A.A.; Chubarev, V.N.; Dostdar, S.A.; Sokolov, A.V.; Brzecka, A.; Sukocheva, O.; Neganova, M.E.; Klochkov, S.G.; Somasundaram, S.G.; et al. Extracellular vesicles in cancer nanomedicine. Semin Cancer Biol 2021, 69, 212-225, https://doi.org/10.1016/j.semcancer.2019.08.017.
8. Wu, P.; Zhang, B.; Ocansey, D.K.W.; Xu, W.; Qian, H. Extracellular vesicles: A bright star of nanomedicine. Biomaterials 2021, 269, 120467, https://doi.org/10.1016/j.biomaterials.2020.120467.
11. Thery, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles 2018, 7, 1535750, https://doi.org/10.1080/20013078.2018.1535750.
12. Kalluri, R.; LeBleu, V.S. The biology, function, and biomedical applications of exosomes. Science 2020, 367, 640-+, https://doi.org/10.1126/science.aau6977.
13. Baek, G.; Choi, H.; Kim, Y.; Lee, H.C.; Choi, C. Mesenchymal Stem Cell-Derived Extracellular Vesicles as Therapeutics and as a Drug Delivery Platform. Stem Cells Translational Medicine 2019, 8, 880-886, https://doi.org/10.1002/sctm.18-0226.
14. Evers, M.; van de Wakker, S.; de Groot, E.; de Jong, O.; Gitz-François, J.; Seinen, C.; Sluijter, J.; Schiffelers, R.; Vader, P. Functional siRNA Delivery by Extracellular Vesicle-Liposome Hybrid Nanoparticles. Advanced healthcare materials 2022, 11, e2101202, https://doi.org/10.1002/adhm.202101202.
15. Pirisinu, M.; Tin Chanh, P.; Zhang, D.X.; Tran Nguyen, H.; Lap Thi, N.; Le, M.T.N. Extracellular vesicles as natural therapeutic agents and innate drug delivery systems for cancer treatment: Recent advances, current obstacles, and challenges for clinical translation. Seminars in Cancer Biology 2022, 80, 340-355, https://doi.org/10.1016/j.semcancer.2020.08.007.
16. Massaro, C.; Sgueglia, G.; Frattolillo, V.; Baglio, S.; Altucci, L.; Dell'Aversana, C. Advances and Future Perspectives inExtracellular Vesicle-Based Nucleic Acid Delivery: Current Cancer Therapeutic Strategies. Pharmaceutics 2020, 12, https://doi.org/10.3390/pharmaceutics12100980.
17. van den Boorn, J.G.; Dassler, J.; Coch, C.; Schlee, M.; Hartmann, G. Exosomes as nucleic acid nanocarriers. Advanced Drug Delivery Reviews 2013, 65, 331-335, https://doi.org/10.1016/j.addr.2012.06.011.
18. Yang, B.; Chen, Y.; Shi, J. Exosome Biochemistry and Advanced Nanotechnology for Next-Generation Theranostic Platforms. Adv Mater 2019, 31, e1802896, https://doi.org/10.1002/adma.201802896.
19. Richter, M.; Vader, P.; Fuhrmann, G. Approaches to surface engineering of extracellular vesicles. Adv Drug Deliv Rev 2021, 173, 416-426, https://doi.org/10.1016/j.addr.2021.03.020.
20. Parada, N.; Romero-Trujillo, A.; Georges, N.; Alcayaga-Miranda, F. Camouflage strategies for therapeutic exosomes evasion from phagocytosis. J Adv Res 2021, 31, 61-74, https://doi.org/10.1016/j.jare.2021.01.001.
21. Jhan, Y.Y.; Prasca-Chamorro, D.; Zuniga, G.P.; Moore, D.M.; Kumar, S.A.; Gaharwar, A.K.; Bishop, C.J. Engineered extracellular vesicles with synthetic lipids via membrane fusion to establish efficient gene delivery. International Journal of Pharmaceutics 2020, 573, https://doi.org/10.1016/j.ijpharm.2019.118802.
22. Wang, J.; Chen, D.; Ho, E.A. Challenges in the development and establishment of exosome-based drug delivery systems. Journal of Controlled Release 2021, 329, 894-906, https://doi.org/10.1016/j.jconrel.2020.10.020.
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics14102236
