The Nurses' Health Study is a series of prospective studies that examine epidemiology and the long-term effects of nutrition, hormones, environment, and nurses' work-life on health and disease development. The studies have been among the largest investigations into risk factors for major chronic diseases ever conducted. The Nurses' Health Studies have led to many insights on health and well-being, including cancer prevention, cardiovascular disease, and type 2 diabetes. They have included clinicians, epidemiologists, and statisticians at the Channing Laboratory (of Brigham and Women's Hospital), Harvard Medical School, Harvard School of Public Health, and several Harvard-affiliated hospitals, including Brigham and Women's Hospital, Dana–Farber Cancer Institute, Children's Hospital Boston, and Beth Israel Deaconess Medical Center.
- epidemiology
- nurses#39
- health
1. Cohorts
| Study | Year | PI | Enrollees |
|---|---|---|---|
| Nurses' Health Study | 1976 | Frank Speizer | 121,700 |
| Nurses' Health Study II | 1989 | Walter Willett | 116,430 |
| Nurses' Health Study 3 | 2010 | Jorge Chavarro | target: 100,000 |
The Nurses' Health Study original cohort was established in 1976 by Dr. Frank Speizer.[2] Initially, the study investigated contraceptive use, smoking, cancer, and cardiovascular disease.[3] The 1976 baseline group included married female registered nurses between the ages of 30 and 55.[3] Approximately 121,700 participants in 11 of the most populous U.S. states (California , Connecticut, Florida, Maryland, Massachusetts , Michigan, New Jersey, New York, Ohio, Pennsylvania, and Texas ) responded. The survey was then distributed biennially thereafter.[3] Over the years, the principal investigator of the Nurses' Health Study have been Frank Speizer, Graham Colditz, Sue Hankinson, and Meir Stampfer.[4]
Over time, the study expanded. Most notably, a dietary questionnaire was added in 1980 due to investigators recognizing the impact of diet and nutrition on the development of chronic disease. Blood, urine, saliva, and other physical samples were received and tested beginning in 1982.[2] Experimenters followed up reports of morbidity using the National Death Index.[2] Where possible and permitted, cancer diagnoses were reviewed.[2] Although reports of other diseases were not followed up, self-reporting has been confirmed by medical records and doctors unaware of the answers to the study's questions.[2]
The Nurses' Health Study II was established in 1989 by Dr. Walter Willett, who has been its principal investigator since inception. The focus of the study was women's health, especially the long term adverse effects of oral contraceptives.[3] The sample population contained females within the age range of 25-42, employed as nurses, from 14 U.S. States.[2] Data collected included the brand of pill and length of use.[2] Over time, the study expanded to include information on basic practices and measurements of health, such as exercise practices and food intake.[2]
Between the years of 1996 and 1999, approximately 30,000 nurses volunteered to provide blood and urine samples to the study.[5] Of these women, 18,500 were pre-menopausal, providing samples at specific points in the menstrual cycle.[5] These data allowed researchers to study how hormone levels influence the risk of disease. A second set of samples was collected from 16,500 of the same group of women in 2010-2012, by which time most of them were postmenopausal.[5] Over 25,000 children of women in the Nurses' Health Study II cohort were enrolled in their own follow-up study called the Growing Up Today Study, or GUTS, which has followed the subjects through their early life so as to obtain a second generation of data.[6]
The Nurses' Health Study 3 was developed in 2010 by Drs. Jorge Chavarro, Walter Willett, Janet Rich-Edwards, and Stacey Missmer.[3] The study includes investigators from the Channing Division of Network Medicine at Brigham and Women's Hospital, Harvard Medical School, and Harvard T.H. Chan School of Public Health.[7] The original population contained females 19-49 in age and expanded to include Canadian subjects.[2] Unlike the predecessor studies, the NH3 includes participants of both male and female genders in 2015.[2] Jorge Chavarro has been the principal investigator of Nurses' Health Study 3 since its 2010 inception.[2]
2. Findings
The studies revealed many correlations, that is statistical relationships, whether causal or not, between environmental factors and risk for health conditions.
Smoking: correlated to a higher likelihood of cardiovascular disease (CVD),[8] colorectal[9] and pancreatic[10] cancer, psoriasis,[11] multiple sclerosis,[12] type 2 diabetes,[13] and eye disease.[14]
Trans Fats: correlation between cardiovascular disease (CVD) and consumption of trans fatty acids.[15] Initially met with skepticism,[16] it ultimately led to trans fat being added to U.S. food labels in 2003 [17] and partially hydrogenated oils being labeled as not generally recognized as safe (GRAS) by the FDA.[18]
Obesity: correlated to a higher likelihood of cardiovascular disease (CVD),[19] breast cancer,[20] pancreatic cancer,[21] psoriasis,[22] multiple sclerosis,[23] gallstones,[24] type 2 diabetes,[25] and eye disease.[26]
Postmenopausal Hormone Therapy: correlated to a lower likelihood of cardiovascular disease (CVD).[27] Combination hormones (progesteron and estrogen) were associated with higher risk of breast cancer.[28][29]
Oral Contraceptives: correlated to a lower likelihood of ovarian cancer.[30] No statistically significant effects of oral contraceptives were observed in regard to risk of breast cancer.[31] Present or past use did not correlate significantly with CVD.[32]
Exercise: correlated to higher likelihood of breast cancer survival.[33] Physical activity was correlated to a decreased likelihood of cardiovascular disease (CVD)[34] and type 2 diabetes.[35]
Many relationships and factors were examined over the course of the study, examples including diet, coffee consumption, and sleep.[36] Many publications diverse findings were produced as a result.
3. History
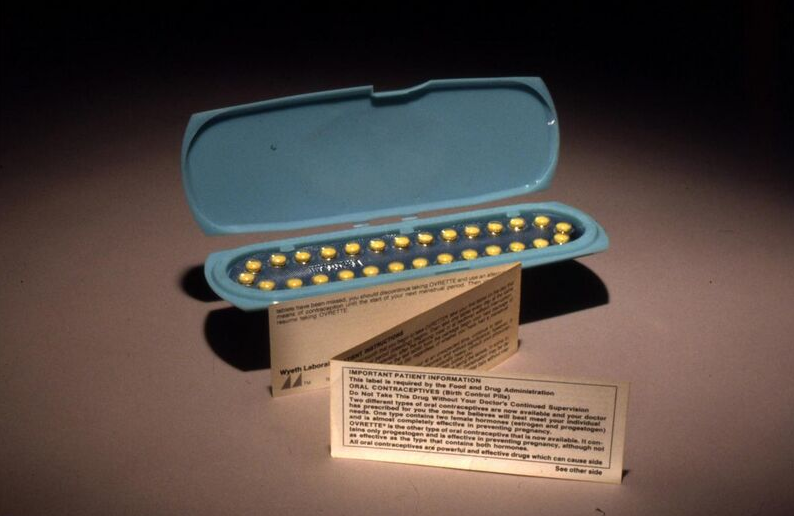
Beginning in the 1960s, oral contraceptives were used by the public in the U.S. and U.K.[2] As soon as 1966, however, there were reports of women falling ill with cardiovascular disease in association with these contraceptives.[2] Doctors Frank Speizer and Martin Vessey hoped to better understand the effects of long-term use of oral contraceptives on the health of women.[2] After receiving funding from the National Cancer Institute in 1974, the study was directed towards the wives of doctors. When it was discovered that such responses were not ideal due to lack of medical knowledge of the participants, the study shifted its focus to nurses.[2] The studies did not remain focused on oral contraceptives, but expanded to investigate factors such as smoking, diet, and exercise. These conditions demonstrated relationships with states of health, such as risk of developing chronic disease.[2] Because the women continued submitting their responses as time passed, the Nurses' Health Study was the first cohort study of such magnitude to follow a population over time.[2] The study has continued into 2018, and as of 2016 were funded almost entirely (90%) by the federal government.[2]
4. Impact
Data received from the study has expanded the understanding of women's health. Public messages from the United States Surgeon General, World Health Organization, and World Cancer Research Fund have resulted from the findings of the Nurses' Health Study.[38] Policies such as the 2008 Physical Activity Guidelines for Americans and the Dietary Guidelines of the Food and Drug Administration regarding trans-fat related to the findings of these studies.[38] Studies to date have led to the publication of hundreds of peer-reviewed papers.[39] Influential figures in the Nurses' Health Study have published advice for women based on their findings. For example, the book Healthy Women and Healthy Lives was written by Hankson, Colditz, Manson, and Speizer to reflect results of the study. This work makes explicit suggestions for a healthy lifestyle based on the study.[40]
5. Public Reaction
This study was referenced in popular news by many sources. The term "Nurses' Health Study" has been stated in over three hundred articles of the New York Times and The Washington Post alone.[41] These articles discussed the findings of the study, such as one titled Women, Alcohol and the Search for Certainty.[42] Published as early as 1988, this Washington Post article discussed the effect of the Nurses' Health Study on the relationship between women and alcohol, citing the former as a factor which affects a woman's risk for CVD and strokes.[42] News outlets have also described the more general implications of the study, such as a piece titled It's Never Too Late to Be Healthy, Studies Show.[43] The 2004 article discusses the research of the study and resulting understanding of general health in older populations.[43] The impact of the study itself was also in the public eye. In the New York Times article In Nurses' Lives, a Treasure Trove of Health Data, nurses themselves were cited as changing daily habits and considering their choices as a result of their participation.[44] In this way, the findings and magnitude of the Nurses Health Study reached the public throughout its history.
6. Limitations and Controversy
The Nurses' Health Study 1 contained populations representing nurses of the time, but did not reflect great diversity. The participants had a slightly higher income than the average of the time and a majority were white (97%).[2] In 2012, however, minority participants were increasingly sought after.[38] Leaders of the experiment made this a priority by sending extra information on the study to possible subjects living in areas of high diversity.[2] In 2015 males were accepted into the study.[38] This was caused by an increase in the number of males in the nursing profession.[38]
The Nurses' Health Study faced controversy based on its recommendations. The study published in 1985 that taking estrogen as a part of Hormone Replacement Therapy would lead to large decreases in risk of heart disease (a third of the risk of those who did not take supplements).[45] However, the Framingham Heart Study found the opposite result.[46] This controversy caused a 10-year follow up by the Nurses' Health Study which again concluded that risks of CVD were lower in samples currently taking hormones.[46] However, further studies such as the Heart and Estrogen-progestin Replacement Study found that estrogen tablets actually increase risk for heart disease. This was a double-blind trial following an experimental group of women who were given replacement therapy pills and a control group following the same procedure with placebos.[47] Findings from the study displayed a direct relationship between therapy and risk for heart disease, as opposed to the previously stated benefits.[48] This finding largely opposed the published Nurses' Health Study conclusion.
The content is sourced from: https://handwiki.org/wiki/Medicine:Nurses%27_Health_Study
References
- Feldscher, Karen. "Nurses' Health Study 3 ramps up its recruiting efforts". Harvard T.H. Chan School of Public Health. https://www.hsph.harvard.edu/news/features/nurses-health-study-3-ramps-up-its-recruiting-efforts/. Retrieved February 2, 2020.
- Bao, Ying; Bertoia, Monica; Lenart, Elizabeth; Stampfer, Meir; Willett, Walter; Speizer, Frank; Chavarro, Jorge (September 2016). "Origin, Methods, and Evolution of the Three Nurses' Health Studies". American Journal of Public Health 106 (9): 1573–1581. doi:10.2105/AJPH.2016.303338. PMID 27459450. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4981810
- "History | Nurses' Health Study" (in en). http://www.nurseshealthstudy.org/about-nhs/history.
- "Principal investigators | Nurses' Health Study". http://www.nurseshealthstudy.org/about/principal-investigators.
- "History | Nurses' Health Study" (in en). http://www.nurseshealthstudy.org/about-nhs/history.
- Chavarro, Jorge; Rich-Edwards, Janet; Gaskins, Audrey; Farland, Leslie; Terry, Kathryn; Zhang, Cuilin; Missmer, Stacy (September 2016). "Contributions of the Nurses' Health Studies to Reproductive Health Research". American Journal of Public Health 106 (9): 1669–1676. doi:10.2105/AJPH.2016.303350. PMID 27459445. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4981818
- "Nurses' Health Studies" (in en-US). The Nurses' Health Study. 2016-08-16. https://www.hsph.harvard.edu/nutritionsource/nurses-health-study/.
- Willett, W. C.; Green, A.; Stampfer, M. J.; Speizer, F. E.; Colditz, G. A.; Rosner, B.; Monson, R. R.; Stason, W. et al. (1987-11-19). "Relative and absolute excess risks of coronary heart disease among women who smoke cigarettes". The New England Journal of Medicine 317 (21): 1303–1309. doi:10.1056/NEJM198711193172102. ISSN 0028-4793. PMID 3683458. https://dx.doi.org/10.1056%2FNEJM198711193172102
- Wei, Esther K.; Giovannucci, Edward; Wu, Kana; Rosner, Bernard; Fuchs, Charles S.; Willett, Walter C.; Colditz, Graham A. (2004-01-20). "Comparison of risk factors for colon and rectal cancer". International Journal of Cancer 108 (3): 433–442. doi:10.1002/ijc.11540. ISSN 0020-7136. PMID 14648711. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2903217
- Fuchs, C. S.; Colditz, G. A.; Stampfer, M. J.; Giovannucci, E. L.; Hunter, D. J.; Rimm, E. B.; Willett, W. C.; Speizer, F. E. (1996-10-28). "A prospective study of cigarette smoking and the risk of pancreatic cancer". Archives of Internal Medicine 156 (19): 2255–2260. doi:10.1001/archinte.1996.00440180119015. ISSN 0003-9926. PMID 8885826. https://dx.doi.org/10.1001%2Farchinte.1996.00440180119015
- Setty, Arathi R.; Curhan, Gary; Choi, Hyon K. (2007-11-01). "Smoking and the Risk of Psoriasis in Women: Nurses' Health Study II" (in en). The American Journal of Medicine 120 (11): 953–959. doi:10.1016/j.amjmed.2007.06.020. ISSN 0002-9343. PMID 17976422. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2696351
- Hernan, M. A. (2001-07-01). "Cigarette Smoking and Incidence of Multiple Sclerosis" (in en). American Journal of Epidemiology 154 (1): 69–74. doi:10.1093/aje/154.1.69. ISSN 0002-9262. PMID 11427406. https://dx.doi.org/10.1093%2Faje%2F154.1.69
- Rimm, E. B.; Manson, J. E.; Stampfer, M. J.; Colditz, G. A.; Willett, W. C.; Rosner, B.; Hennekens, C. H.; Speizer, F. E. (1993). "Cigarette smoking and the risk of diabetes in women". American Journal of Public Health 83 (2): 211–214. doi:10.2105/AJPH.83.2.211. ISSN 0090-0036. PMID 8427325. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1694562
- Hankinson, S. E.; Willett, W. C.; Colditz, G. A.; Seddon, J. M.; Rosner, B.; Speizer, F. E.; Stampfer, M. J. (1992-08-26). "A prospective study of cigarette smoking and risk of cataract surgery in women". JAMA 268 (8): 994–998. doi:10.1001/jama.1992.03490080068026. ISSN 0098-7484. PMID 1501325. https://dx.doi.org/10.1001%2Fjama.1992.03490080068026
- Willett, W. C.; Stampfer, M. J.; Manson, J. E.; Colditz, G. A.; Speizer, F. E.; Rosner, B. A.; Sampson, L. A.; Hennekens (1993-03-06). "Intake of trans fatty acids and risk of coronary heart disease among women". Lancet 341 (8845): 581–585. doi:10.1016/0140-6736(93)90350-p. PMID 8094827. https://dx.doi.org/10.1016%2F0140-6736%2893%2990350-p
- "NURSES' HEALTH STUDY NEWSLETTER" (in en). https://www.nurseshealthstudy.org/sites/default/files/pdfs/2012newsletter.pdf. ,
- "Small Entity Compliance Guide on Labeling Trans" (in en). 20 August 2003. https://www.federalregister.gov/documents/2003/08/20/03-21228/small-entity-compliance-guide-on-labeling-trans.
- "Final Determination Regarding Partially Hydrogenated Oils (Removing Trans Fat)" (in en). FDA. 20 February 2020. https://www.fda.gov/food/food-additives-petitions/final-determination-regarding-partially-hydrogenated-oils-removing-trans-fat. Retrieved 2020-11-15.
- Eckel, N; Li, Y; Kuxhaus, O; Stefan, N; Hu, FB; Schulze, MB (2018). "Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses' Health Study): 30 year follow-up from a prospective cohort study.". Lancet Diabetes Endocrinol 6 (9): 714–724. doi:10.1016/S2213-8587(18)30137-2. PMID 29859908. https://dx.doi.org/10.1016%2FS2213-8587%2818%2930137-2
- Hirko, KA; Chai, B; Spiegelman, D; Campos, H; Farvid, MS; Hankinson, SE; Willett, WC; Eliassen, AH (2018). "Erythrocyte membrane fatty acids and breast cancer risk: a prospective analysis in the nurses' health study II". International Journal of Cancer 142 (6): 1116–1129. doi:10.1002/ijc.31133. PMID 29071721. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5773390
- Michaud, Dominique S. (2001-08-22). "Physical Activity, Obesity, Height, and the Risk of Pancreatic Cancer" (in en). JAMA 286 (8): 921–9. doi:10.1001/jama.286.8.921. ISSN 0098-7484. PMID 11509056. https://dx.doi.org/10.1001%2Fjama.286.8.921
- Setty, Arathi R.; Curhan, Gary; Choi, Hyon K. (2007). "Obesity, waist circumference, weight change, and the risk of psoriasis in women: Nurses' Health Study II". Archives of Internal Medicine 167 (15): 1670–1675. doi:10.1001/archinte.167.15.1670. ISSN 0003-9926. PMID 17698691. https://dx.doi.org/10.1001%2Farchinte.167.15.1670
- Munger, Kassandra L.; Chitnis, Tanuja; Ascherio, Alberto (2009-11-10). "Body size and risk of MS in two cohorts of US women" (in en). Neurology 73 (19): 1543–1550. doi:10.1212/WNL.0b013e3181c0d6e0. ISSN 0028-3878. PMID 19901245. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2777074
- Field, Alison E.; Coakley, Eugenie H.; Must, Aviva; Spadano, Jennifer L.; Laird, Nan; Dietz, William H.; Rimm, Eric; Colditz, Graham A. (2001-07-09). "Impact of Overweight on the Risk of Developing Common Chronic Diseases During a 10-Year Period" (in en). Archives of Internal Medicine 161 (13): 1581–6. doi:10.1001/archinte.161.13.1581. ISSN 0003-9926. PMID 11434789. https://dx.doi.org/10.1001%2Farchinte.161.13.1581
- Carey, Vincent; Walters, Ellen; Colditz, Graham; Solomon, Caren; Willet, Walter; Rosner, Bernard; Speizer, Frank E.; Manson, JoAnn (1997). "Body Fat Distribution and Risk of Non-Insulin-dependent Diabetes Mellitus in Women: The Nurses' Health Study". American Journal of Epidemiology 145 (7): 614–9. doi:10.1093/oxfordjournals.aje.a009158. PMID 9098178. https://dx.doi.org/10.1093%2Foxfordjournals.aje.a009158
- Weintraub, JM; Willett, WC; Rosner, B; Colditz, GA; Seddon, JM; Hankinson, SE (December 2002). "A prospective study of the relationship between body mass index and cataract extraction among US women and men" (in En). International Journal of Obesity 26 (12): 1588–1595. doi:10.1038/sj.ijo.0802158. ISSN 0307-0565. PMID 12461675. https://dx.doi.org/10.1038%2Fsj.ijo.0802158
- Stampfer, M. J.; Willett, W. C.; Colditz, G. A.; Rosner, B.; Speizer, F. E.; Hennekens, C. H. (1985-10-24). "A prospective study of postmenopausal estrogen therapy and coronary heart disease". The New England Journal of Medicine 313 (17): 1044–1049. doi:10.1056/NEJM198510243131703. ISSN 0028-4793. PMID 4047106. https://dx.doi.org/10.1056%2FNEJM198510243131703
- Colditz, G. A.; Hankinson, S. E.; Hunter, D. J.; Willett, W. C.; Manson, J. E.; Stampfer, M. J.; Hennekens, C.; Rosner, B. et al. (1995-06-15). "The use of estrogens and progestins and the risk of breast cancer in postmenopausal women". The New England Journal of Medicine 332 (24): 1589–1593. doi:10.1056/NEJM199506153322401. ISSN 0028-4793. PMID 7753136. https://dx.doi.org/10.1056%2FNEJM199506153322401
- "Selected publications | Nurses' Health Study" (in en). http://www.nurseshealthstudy.org/selected-publications.
- Collaborative Group on Epidemiological Studies of Ovarian Cancer; Beral, V.; Doll, R.; Hermon, C.; Peto, R.; Reeves, G. (2008-01-26). "Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls". Lancet 371 (9609): 303–314. doi:10.1016/S0140-6736(08)60167-1. ISSN 1474-547X. PMID 18294997. https://cris.maastrichtuniversity.nl/portal/en/publications/ovarian-cancer-and-oral-contraceptives-collaborative-reanalysis-of-data-from-45-epidemiological-studies-including-23257-women-with-ovarian-cancer-and-87303-controls(44267649-a4c1-406e-a328-4cfdb6d80b24).html.
- Lipnick, R. J.; Buring, J. E.; Hennekens, C. H.; Rosner, B.; Willett, W.; Bain, C.; Stampfer, M. J.; Colditz, G. A. et al. (1986-01-03). "Oral contraceptives and breast cancer. A prospective cohort study". JAMA 255 (1): 58–61. doi:10.1001/jama.1986.03370010064026. ISSN 0098-7484. PMID 3940306. https://dx.doi.org/10.1001%2Fjama.1986.03370010064026
- Stampfer, Meir J.; Willett, Walter C.; Colditz, Graham A.; Speizer, Frank E.; Hennekens, Charles H. (July 1990). "Past use of oral contraceptives and cardiovascular disease: A meta-analysis in the context of the Nurses' Health Study" (in en). American Journal of Obstetrics and Gynecology 163 (1): 285–291. doi:10.1016/0002-9378(90)90569-S. ISSN 0002-9378. PMID 2142573. https://www.ajog.org/article/0002-9378(90)90569-S/fulltext.
- Irwin, Melinda L.; Smith, Ashley Wilder; McTiernan, Anne; Ballard-Barbash, Rachel; Cronin, Kathy; Gilliland, Frank D.; Baumgartner, Richard N.; Baumgartner, Kathy B. et al. (2008-08-20). "Influence of Pre- and Postdiagnosis Physical Activity on Mortality in Breast Cancer Survivors: The Health, Eating, Activity, and Lifestyle Study". Journal of Clinical Oncology 26 (24): 3958–3964. doi:10.1200/JCO.2007.15.9822. ISSN 0732-183X. PMID 18711185. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2654316
- Manson, JoAnn E.; Hu, Frank B.; Rich-Edwards, Janet W.; Colditz, Graham A.; Stampfer, Meir J.; Willett, Walter C.; Speizer, Frank E.; Hennekens, Charles H. (1999-08-26). "A Prospective Study of Walking as Compared with Vigorous Exercise in the Prevention of Coronary Heart Disease in Women" (in EN). New England Journal of Medicine 341 (9): 650–658. doi:10.1056/nejm199908263410904. ISSN 0028-4793. PMID 10460816. http://espace.library.uq.edu.au/view/UQ:144950/UQ144950_OA.pdf.
- Manson, J. E.; Rimm, E. B.; Stampfer, M. J.; Colditz, G. A.; Willett, W. C.; Krolewski, A. S.; Rosner, B.; Hennekens, C. H. et al. (1991-09-28). "Physical activity and incidence of non-insulin-dependent diabetes mellitus in women". Lancet 338 (8770): 774–778. doi:10.1016/0140-6736(91)90664-B. ISSN 0140-6736. PMID 1681160. https://dx.doi.org/10.1016%2F0140-6736%2891%2990664-B
- COLDITZ, GRAHAM A.; MANSON, JOANN E.; HANKINSON, SUSAN E. (1997). "The Nurses' Health Study: 20-Year Contribution to the Understanding of Health Among Women" (in en). Journal of Women's Health 6 (1): 49–62. doi:10.1089/jwh.1997.6.49. ISSN 1059-7115. PMID 9065374. https://dx.doi.org/10.1089%2Fjwh.1997.6.49
- "File:Patient Package Insert for Oral Contraceptives (FDA 079) (8249451687).jpg" (in en), Wikipedia, https://en.wikipedia.org/wiki/File:Patient_Package_Insert_for_Oral_Contraceptives_(FDA_079)_(8249451687).jpg, retrieved 2018-11-16
- Colditz, Graham; Philpott, Sydney; Hankinson, Susan E. (September 2016). "The Impact of the Nurses' Health Study on Population Health: Prevention, Translation, and Control". American Journal of Public Health 106(9) (September 216): 1540–1545. doi:10.2105/AJPH.2016.303343. PMID 27459441. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4981811
- List of NHS publications indexed by year https://sites.google.com/a/channing.harvard.edu/nhs-publications/Home/nhs---nhs-ii
- Hankinson, Susan; Colditz, Graham; Manson, JoAnn; Speizer, Frank (2001). Healthy Women, Healthy Lives. New York, NY: Simon & Schuster. ISBN 978-0-684-85519-6. https://archive.org/details/healthywomenheal00susa.
- "Factiva". https://global.factiva.com/ha/default.aspx#./!?&_suid=1541792552103011958772908435156.
- Rovner, Sandy (9 August 1988). "Women, Alcohol and the Search for Certainty". The Washington Post. https://global.factiva.com/ha/default.aspx#./!?&_suid=154066874374808529448361321608.
- Stein, Rob (22 September 2004). "It's Never Too Late to Be Healthy, Studies Show". The Washington Post. https://global.factiva.com/ha/default.aspx#./!?&_suid=154066909332208621992634542217.
- Yoon, Carol Kaesuk. "In Nurses' Lives, a Treasure Trove of Health Data" (in en). https://www.nytimes.com/1998/09/15/science/in-nurses-lives-a-treasure-trove-of-health-data.html.
- Taubes, Gary (17 September 2007). "Do We Really Know What Makes Us Healthy?". The New York Times. https://global.factiva.com/ha/default.aspx#./!?&_suid=154066605058807449088086257397.
- Stampfer, Meir J.; Colditz, Graham A.; Willett, Walter C.; Manson, JoAnn E.; Rosner, Bernard; Speizer, Frank E.; Hennekens, Charles H. (1991-09-12). "Postmenopausal Estrogen Therapy and Cardiovascular Disease" (in EN). New England Journal of Medicine 325 (11): 756–762. doi:10.1056/nejm199109123251102. ISSN 0028-4793. PMID 1870648. https://dx.doi.org/10.1056%2Fnejm199109123251102
- Grady, Deborah; Applegate, William; Bush, Trudy; Furberg, Curt; Riggs, Betty; Hulley, Stephen (August 1998). "Heart and Estrogen/progestin Replacement Study (HERS): Design, Methods, and Baseline Characteristics". Controlled Clinical Trials 19 (4): 314–335. doi:10.1016/S0197-2456(98)00010-5. PMID 9683309. https://dx.doi.org/10.1016%2FS0197-2456%2898%2900010-5
- Blakely, John A. (2000-10-23). "The Heart and Estrogen/Progestin Replacement Study Revisited" (in en). Archives of Internal Medicine 160 (19): 2897–900. doi:10.1001/archinte.160.19.2897. ISSN 0003-9926. PMID 11041895. https://dx.doi.org/10.1001%2Farchinte.160.19.2897
