Iodine is one of the 30 essential elements for life, and its chemical speciation defines its biological activities. Both inorganic and organic chemical species have crucial roles in the biology of most living organisms. The most relevant inorganic species are iodate (IO3−) and iodide (I−), as the major sources of iodine for living beings, together with molecular iodine (I2) and hypoiodous acid (HIO) as the most reactive performing catalytic activities. Conversely, Thyroid Hormones (THs) are the master regulators of the metabolism of vertebrates and the representative organic species. Mainly inorganic species are exploited in the health science industry to produce disinfectants, supplements, medicines, and X-ray contrast media.
- iodine species
- iodide
- molecular iodine
- thyroid hormones
1. Introduction
2. History and Chemical Characteristics
3. Distribution of Iodine
4. Relevant Iodine Species
4.1. Main Inorganic Forms
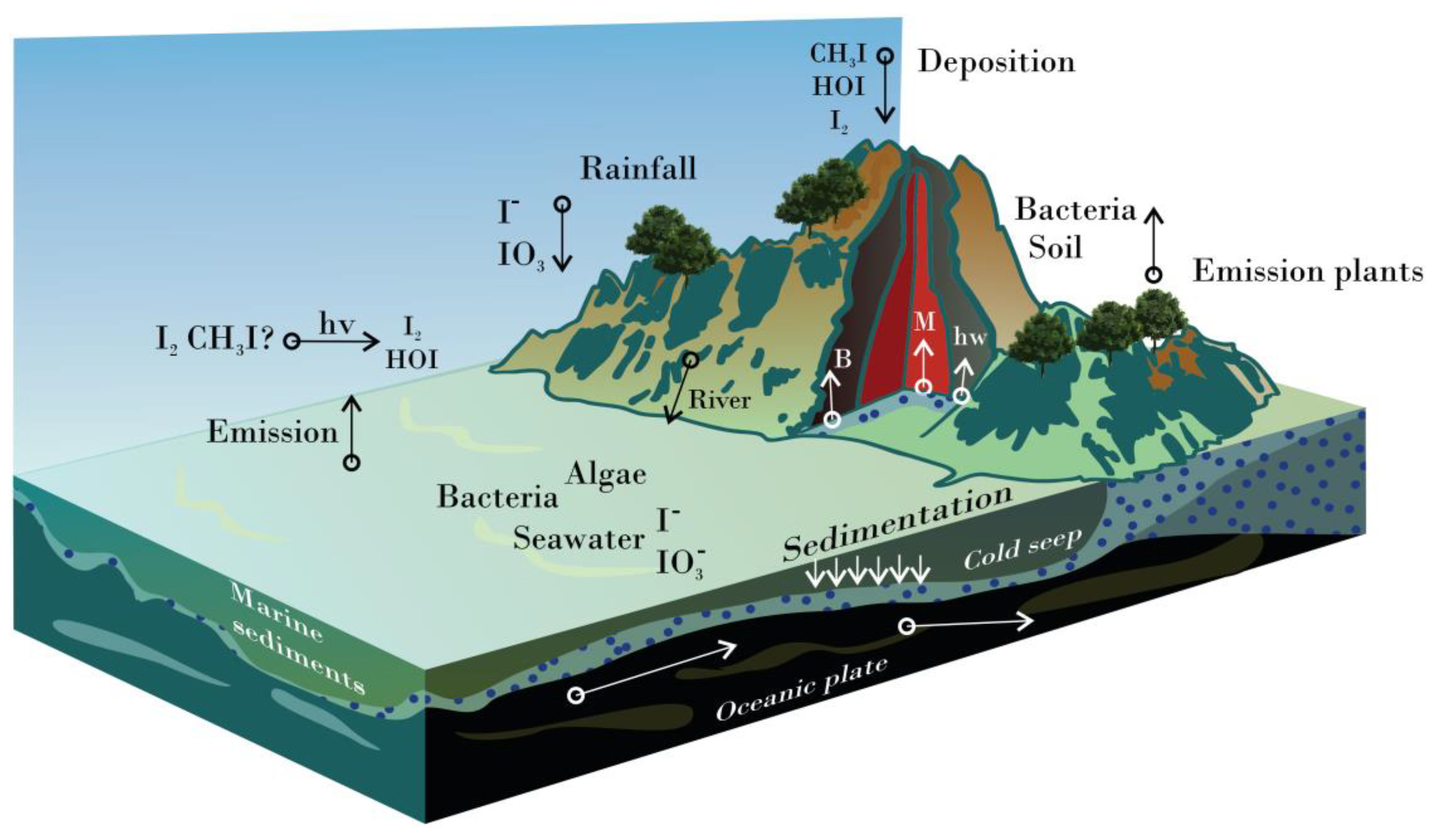
Dominant iodine species in solid-state are potassium iodate (KIO3) and potassium iodide (KI), whereas IO3- and I- ions lead to aqueous systems [19]. I2 and CH3I are the most abundant species in the atmosphere, produced by biotic and abiotic processes [20]. Atmospheric photochemistry promotes the speciation of gaseous iodine species (e.g., HI, IO-, HOI, IONO2 INO2, and IO2) [21][22]. Some of them (mainly I2 and HOI), together with other halogen compounds, are responsible for ozone (O3) depletion in the lower troposphere when interacting with hydrogen-oxygen species and nitrogen oxides [23].
I2 + H2O ↔ HIO + I− + H+. (1)
HIO ↔ OI− + H+. (2)
I2 + I− ↔ I3−. (3)
HIO + H+ ↔ H2OI+. (4)
I3− + I2 ↔ I5-. (5)
2I3− ↔ I62−. (6)
OI− + I- +H2O ↔ HIO2- + OH-. (7)
HIO2- ↔ I2O- + H+. (8)
3HIO ↔ IO3- + 2I- + H+. (9)
4.2. Representative Organic Species
Thyroid hormones (THs) are the protagonists of organic iodine species because of their hormonal role in vertebrate animals. THs comprise i) 3-iodotyrosine or monoiodotyrosine (MIT or T1) and 3,5-diiodotyrosine (DIT) as precursors; ii) 3’,5,3-triiodothyronine (T3) and thyroxine (T4), typically considered as the active hormones; and iii) 3’,5’,3 triiodothyronine or reverse T3 (rT3), 3’,5’ diiodotyrosine (3’,5’-DIT), and 3’- monoiodotyrosine (3’-MIT), the T4 derivatives [28][29]. Other THs derivatives include thyronamines (TAMs) and thyroacetic acids like 3,3',5-triiodothyroacetic acid (Triac), and 3,3′,5,5′-tetraiodothyroacetic acid (Tetrac) produced by deiodination and decarboxylation [29].
Thyroid Peroxidase (TPO) is the enzyme responsible for synthesizing THs using thyroglobulin (TG) as a substrate. TG is the main iodinated compound in the thyroid gland [30][31][32]. The sequence for TH production is TPO incorporates one iodine atom into Tyr residues at position 3 of the ring to produce MIT (reaction 10) and then at position 5 to form DIT (reaction 11). Subsequently, T3 is constructed by an oxidative coupling reaction between one DIT and one MIT (reaction 12), still incorporated into the TG. At the same time, T4 is formed by coupling two adjacent DITs (reaction 13). At the end of the process, only 37 of the ~70 Tyr residues in the TG are known iodination targets [30][31]. Most MITs and DITs produced are kept in the thyroid cells and are eventually degraded by iodotyrosine deiodinases (IYD) enzymes into MIT and Tyr (T0), respectively (reactions 14 and 15) [33]. Meanwhile, T3 and T4 are transported into the bloodstream, mostly bound to plasma proteins. Just a fraction of T3 (21.8%) is synthesized and released in the same fashion as T4; most of it is generated by the deiodination of T4 out of the thyroid by two kinds of iodothyronine deiodinases (ID) (Reaction (16)) [34][35]. A different iodothyronine deiodinase transforms T4 into rT3 (Reaction (17)), an inactive TH produced to maintain hormone homeostasis [36].
Tyr residue + I− + H2O2 + H+ + TPO → MIT + 2H2O + TPO. (10)
MIT + I− + H2O2 + H+ + TPO → DIT + 2H2O + TPO. (11)
MIT + DIT + H2O2 + H+ + TPO → T3 + 2H2O + TG (dehydroalanine). (12)
2DIT + I− + H2O2 + H+ + TPO → T4 + 2H2O + TG (dehydroalanine). (13)
DIT + NADPH + IYD → MIT + NADP+ + I− + IYD. (14)
MIT + NADPH + IYD → Tyr + NADP+ + I− + IYD. (15)
T4 + NADPH + ID→ T3 + NADP+ + I− + ID. (16)
T4 + NADPH + ID→ rT3 + NADP+ + I− + ID. (17)
TPO is also responsible for the iodination of lipids (iodolipids) as α-IHDA and 6-IL. Noticeably, 6-IL was recently related to antioxidant, anti-inflammatory, and anticarcinogenic activities [37][38]. Other peroxidase enzymes like Lactoperoxidase (LPO) are responsible for the synthesis of iodolactones (e.g., δ-lactone of 6-iodo-4-hydroxy-eicosa-8,11,14-trienoic acid, and ε-lactone of 5-iodo-4-hydroxy-7-docosapentaenoic acid) using docosahexaenoic acid (DHA) as a substrate [39].
5. Iodine in the Industry
6. Applications in the Health Sciences
6.1. Disinfection, Asepsis, and Wound Care
6.2. Supplementation
6.3. Contrast Agents
6.4. Applications in Nuclear Medicine
| Isotope | Abundance | Atomic Mass | Half-Life | Decay Mode (%) | keV | Production | Application |
|---|---|---|---|---|---|---|---|
| 123I | Synthetic | 122.9056 | 13.2232 h | β+ (100%) | 159 | Cyclotron | Diagnosis (SPECT) and therapy |
| 124I | Synthetic | 123.9062 | 4.176 d | β+ (100%) | 603 | Cyclotron | Research and diagnosis (PET) |
| 125I | Synthetic | 124.9046 | 59.392 d | ε (100%) | 27.5 | Nuclear reactor and cyclotron | Therapy and radioimmunoassay |
| 127I | Natural (1) | 126.9045 | Stable | Natural | Diagnosis (X-rays and CT) and therapy | ||
| 131I | Synthetic | 130.9061 | 8.0249 d | β− (100) | 364.5 | Nuclear reactor | Diagnosis, therapy, and RIA |
6.5. Prophylaxis
| Age Group | I2 (mg) |
KI (mg) |
KIO3 (mg) | Fraction of a Tablet (100 mg) |
|---|---|---|---|---|
| Adults and adolescents, including lactating women (>12 years) | 100 | 130 | 170 | 1 |
| Children (3–12 years) | 50 | 65 | 85 | 1/2 |
| Infants (1 month–3 years) | 25 | 32 | 42 | 1/4 |
| Neonates (birth–1 month) | 12.5 | 16 | 21 | 1/8 |
This entry is adapted from the peer-reviewed paper 10.3390/futurepharmacol2040026
References
- Venturi, S.; Donati, F.M.; Venturi, A.; Venturi, M. Environmental Iodine Deficiency: A Challenge to the Evolution of Terrestrial Life? Thyroid 2000, 10, 727–729.
- Gottardi, W. Iodine as Disinfectant. In Iodine Chemistry and Applications; Kaiho, T., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 9781118466, pp. 375–410.
- Crockford, S.J. Evolutionary Roots of Iodine and Thyroid Hormones in Cellcell Signaling. Integr. Comp. Biol. 2009, 49, 155–166.
- Venkatesh Mannar, M.G.; Dunn, J.T.; World Health Organization. Salt Iodization for the Elimination of Iodine Deficiency; International Council for Control of Iodine Deficiency Disorders: Brussels; Belgium, 1995.
- Diosady, L.L.; Alberti, J.O.; Mannar, M.G.V.; FitzGerald, S. Stability of Iodine in Iodized Salt Used for Correction of Iodine-Deficiency Disorders. II. Food Nutr. Bull. 1998, 19, 240–250.
- Aceves, C.; Mendieta, I.; Anguiano, B.; Delgado-González, E. Molecular Iodine Has Extrathyroidal Effects as an Antioxidant, Differentiator, and Immunomodulator. Int. J. Mol. Sci. 2021, 22, 1228.
- World Health Organization. Protection of the Human Environment. Guidelines for Iodine Prophylaxis Following Nuclear Accidents; Update 1999; World Health Organization: Geneva, Switzerland, 1999; pp. 1–45.
- Küpper, F.C.; Feiters, M.C.; Olofsson, B.; Kaiho, T.; Yanagida, S.; Zimmermann, M.B.; Carpenter, L.J.; Luther, G.W.; Lu, Z.; Jonsson, M.; et al. Commemorating Two Centuries of Iodine Research: An Interdisciplinary Overview of Current Research. Angew. Chemie Int. Ed. 2011, 50, 11598–11620.
- National Center for Biotechnology Information PubChem Element Summary for AtomicNumber 53, Iodine. Available online: https://pubchem.ncbi.nlm.nih.gov/element/Iodine (accessed on 24 April 2022).
- Meija, J.; Coplen, T.B.; Berglund, M.; Brand, W.A.; De Bièvre, P.; Gröning, M.; Holden, N.E.; Irrgeher, J.; Loss, R.D.; Walczyk, T.; et al. Isotopic Compositions of the Elements 2013 (IUPAC Technical Report). Pure Appl. Chem. 2016, 88, 293–306.
- Edwards, R.R. Iodine-129: Its Occurrence in Nature and Its Utility as a Tracer. Science 1962, 137, 851–853.
- Kaiho, T. Inorganic Iodides. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 9781118466, pp. 55–73.
- Muramatsu, Y.; Yoshida, S.; Fehn, U.; Amachi, S.; Ohmomo, Y. Studies with Natural and Anthropogenic Iodine Isotopes: Iodine Distribution and Cycling in the Global Environment. J. Environ. Radioact. 2004, 74, 221–232.
- Moreda-Piñeiro, A.; Romarís-Hortas, V.; Bermejo-Barrera, P. A Review on Iodine Speciation for Environmental, Biological and Nutrition Fields. J. Anal. At. Spectrom. 2011, 26, 2107.
- Amachi, S. Microbial Contribution to Global Iodine Cycling: Volatilization, Accumulation, Reduction, Oxidation, and Sorption of Iodine. Microbes Environ. 2008, 23, 269–276.
- Kocher, D.C. A Dynamic Model of the Global Iodine Cycle and Estimation of Dose to the World Population from Releases of Iodine-129 to the Environment. Environ. Int. 1981, 5, 15–31.
- Elmore, D.; Gove, H.E.; Ferraro, R.; Kilius, L.R.; Lee, H.W.; Chang, K.H.; Beukens, R.P.; Litherland, A.E.; Russo, C.J.; Purser, K.H.; et al. Determination of 129I Using Tandem Accelerator Mass Spectrometry. Nature 1980, 286, 138–140.
- Brown, C.F.; Geiszler, K.N.; Lindberg, M.J. Analysis of 129I in Groundwater Samples: Direct and Quantitative Results below the Drinking Water Standard. Appl. Geochemistry 2007, 22, 648–655.
- Crivello, J.V. Diaryliodonium Salt Photoacid Generators. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 457–478.
- Carpenter, L.J. Atmospheric Chemistry of Iodine. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 591–601.
- Cox, R.A.; Bloss, W.J.; Jones, R.L.; Rowley, D.M. OIO and the Atmospheric Cycle of Iodine. Geophys. Res. Lett. 1999, 26, 1857–1860.
- Chameides, W.L.; Davis, D.D. Iodine: Its Possible Role in Tropospheric Photochemistry. J. Geophys. Res. Ocean. 1980, 85, 7383–7398.
- Raso, A.R.W.; Custard, K.D.; May, N.W.; Tanner, D.; Newburn, M.K.; Walker, L.; Moore, R.J.; Huey, L.G.; Alexander, L.; Shepson, P.B.; et al. Active Molecular Iodine Photochemistry in the Arctic. Proc. Natl. Acad. Sci. USA 2017, 114, 10053–10058.
- Yuita, K. Dynamics of Iodine, Bromine, and Chlorine in Soil: II. Chemical Forms of Iodine in Soil Solutions. Soil Sci. Plant Nutr. 1992, 38, 281–287.
- Li, J.; Wang, Y.; Guo, W.; Xie, X.; Zhang, L. Factors Controlling Spatial Variation of Iodine Species in Groundwater of the Datong Basin, Northern China. Procedia Earth Planet. Sci. 2013, 7, 483–486.
- Gottardi, W. Iodine and Disinfection: Theoretical Study on Mode of Action, Efficiency, Stability, and Analytical Aspects in the Aqueous System. Arch. Pharm. 1999, 332, 151–157.
- Gottardi, W. Potentiometrische Bestimmung Der Gleichgewichtskonzentrationen an Freiem Und Komplex Gebundenem Iod in W~iflrigen Liisungen von Polyvinylpyrrolidon-Iod (PVP-Iod) Polyvinylpyrrolidon-Iod (PVP-Iod). Fresenius’ Zeitschrift für Anal. Chemie 1983, 314, 582–585.
- Hulbert, A.J. Thyroid Hormones and Their Effects: A New Perspective. Biol. Rev. 2000, 75, 519–631.
- Köhrle, J. Thyroid Hormones and Derivatives: Endogenous Thyroid Hormones and Their Targets. In Thyroid Hormone Nuclear Receptor; Springer: Berlin, Germany, 2018; Volume 1897, pp. 85–104.
- Citterio, C.E.; Targovnik, H.M.; Arvan, P. The Role of Thyroglobulin in Thyroid Hormonogenesis. Nat. Rev. Endocrinol. 2019, 15, 323–338.
- Dedieu, A.; Gaillard, J.-C.; Pourcher, T.; Darrouzet, E.; Armengaud, J. Revisiting Iodination Sites in Thyroglobulin with an Organ-Oriented Shotgun Strategy. J. Biol. Chem. 2011, 286, 259–269.
- Fong, P. Thyroid Iodide Efflux: A Team Effort? J. Physiol. 2011, 589, 5929–5939.
- Vermot, A.; Petit-Härtlein, I.; Smith, S.M.E.; Fieschi, F. NADPH Oxidases (NOX): An Overview from Discovery, Molecular Mechanisms to Physiology and Pathology. Antioxidants 2021, 10, 890.
- Milanesi, A.; Brent, G.A. Iodine and Thyroid Hormone Synthesis, Metabolism, and Action. In Molecular, Genetic, and Nutritional Aspects of Major and Trace Minerals; Elsevier: Amsterdam, The Netherlands, 2017; Volume 1896, pp. 143–150.
- Nicoloff, J.T.; Low, J.C.; Dussault, J.H.; Fisher, D.A. Simultaneous Measurement of Thyroxine and Triiodothyronine Peripheral Turnover Kinetics in Man. J. Clin. Invest. 1972, 51, 473–483.
- Gomes-Lima, C.; Burman, K.D. Reverse T 3 or Perverse T 3? Still Puzzling after 40 Years. Cleve. Clin. J. Med. 2018, 85, 450–455.
- Pereira, A.; Braekman, J.C.; Dumont, J.E.; Boeynaems, J.M. Identification of a Major Iodolipid from the Horse Thyroid Gland as 2-Iodohexadecanal. J. Biol. Chem. 1990, 265, 17018–17025.
- Aceves, C.; Anguiano, B.; Delgado, G. Is Iodine a Gatekeeper of the Integrity of the Mammary Gland? J. Mammary Gland Biol. Neoplasia 2005, 10, 189–196.
- Dembitsky, V.M. Biogenic Iodine and Iodine-Containing Metabolites. Nat. Prod. Commun. 2006, 1, 1934578X0600100.
- Wang, X.; Yan, F.; Wang, Q. Molecular Iodine: Catalysis in Heterocyclic Synthesis. Synth. Commun. 2021, 51, 1763–1781.
- Bürgi, H.; Schaffner, T.; Seiler, J.P. The Toxicology of Iodate: A Review of the Literature. Thyroid 2001, 11, 449–456.
- Tekale, S.U.; Kauthale, S.S.; Dake, S.A.; Sarda, S.R.; Pawar, R.P. Molecular Iodine: An Efficient and Versatile Reagent for Organic Synthesis. Curr. Org. Chem. 2012, 16, 1485–1501.
- Dohi, T.; Kita, Y. Oxidizing Agents. In Iodine Chemistry and Applications; Kaiho, T., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 277–301.
- World Health Organization. WHO Model List of Essential Medicines—22nd List; World Health Organization: Geneva, Switzerland, 2021; p. 66.
- Lugol, J.G.A. Mémoire Sur l’Emploi de l’Iode Dans Les Maladies Scrofuleuses. Glasgow Med. J. 1832, 5, 83–92.
- Cooper, R.A. Iodine Revisited. Int. Wound J. 2007, 4, 124–137.
- Fernández, L. Global Market Value of Iodine 2017 & 2024. Available online: https://www.statista.com/statistics/1001959/market-value-iodine-worldwide/ (accessed on 2 March 2022).
- Garside, M. Iodine Global Reserves by Countries 2020. Available online: https://www.statista.com/statistics/264946/global-iodine-reserves-by-countries/ (accessed on 2 March 2022).
- Garside, M. Major Countries in Iodine Production 2010–2020. Available online: https://www.statista.com/statistics/264945/major-countries-in-iodine-production/ (accessed on 2 March 2022).
- Rayyes, A.; Hamid, A. Technical Meeting of Project Counterparts on Cyclotron Production of I-123. In Proceedings of the Cyclotron production of Iodine-123, Sao Paulo, Brazil, 8–10 August 2001; International Atomic Energy Agency: Vienna, Brazil, 2002; pp. 81–89.
- Chattopadhyay, S.; Saha Das, S. Recovery of 131I from Alkaline Solution of N-Irradiated Tellurium Target Using a Tiny Dowex-1 Column. Appl. Radiat. Isot. 2010, 68, 1967–1969.
- Statista Research Department Global Demand for Iodine by Application 2016. Available online: https://www.statista.com/statistics/862097/global-iodine-demand-share-by-application/ (accessed on 2 March 2022).
- Sharma, A.; Stan, M.N. Thyrotoxicosis: Diagnosis and Management. Mayo Clin. Proc. 2019, 94, 1048–1064.
- Horn-Ross, P.L.; Morris, J.S.; Lee, M.; West, D.W.; Whittemore, A.S.; McDougall, I.R.; Nowels, K.; Stewart, S.L.; Spate, V.L.; Shiau, A.C.; et al. Iodine and Thyroid Cancer Risk among Women in a Multiethnic Population: The Bay Area Thyroid Cancer Study. Cancer Epidemiol Biomarkers Prev. 2001, 10, 979–985.
- Zimmermann, M.B.; Galetti, V. Iodine Intake as a Risk Factor for Thyroid Cancer: A Comprehensive Review of Animal and Human Studies. Thyroid Res. 2015, 8, 8.
- Rackur, H. New Aspects of Mechanism of Action of Povidone-Iodine. J. Hosp. Infect. 1985, 6, 13–23.
- Bafort, F.; Parisi, O.; Perraudin, J.-P.; Jijakli, M.H. Mode of Action of Lactoperoxidase as Related to Its Antimicrobial Activity: A Review. Enzyme Res. 2014, 2014, 517164.
- Ren, B.; Zhu, Y. A New Perspective on Thyroid Hormones: Crosstalk with Reproductive Hormones in Females. Int. J. Mol. Sci. 2022, 23, 2708.
- Gottardi, W. Potentiometrische Bestimmung Der Gleichgewichtskonzentrationen an Freiem Und Komplex Gebundenem Iod in W~iflrigen Liisungen von Polyvinylpyrrolidon-Iod (PVP-Iod) Polyvinylpyrrolidon-Iod (PVP-Iod). Fresenius’ Zeitschrift für Anal. Chemie 1983, 314, 582–585.
- Reddy, J.M.; Knox, K.; Robin, M.B. Crystal Structure of HI 3 ·2C 6 H 5 CONH 2: A Model of the Starch—Iodine Complex. J. Chem. Phys. 1964, 40, 1082–1089.
- Gottardi, W. Iodine and Disinfection: Theoretical Study on Mode of Action, Efficiency, Stability, and Analytical Aspects in the Aqueous System. Arch. Pharm. 1999, 332, 151–157.
- Makhayeva, D.N.; Irmukhametova, G.S.; Khutoryanskiy, V.V. Polymeric Iodophors: Preparation, Properties, and Biomedical Applications. Rev. J. Chem. 2020, 10, 40–57.
- French, E.A.; Mukai, M.; Zurakowski, M.; Rauch, B.; Gioia, G.; Hillebrandt, J.R.; Henderson, M.; Schukken, Y.H.; Hemling, T.C. Iodide Residues in Milk Vary between Iodine-Based Teat Disinfectants. J. Food Sci. 2016, 81, T1864–T1870.
- Sukawa, H.; Yoda, Y.; Sugimoto, H.; Yoshida, S.; Yamamoto, T.; Kuroda, S.; Sanechika, K.; Nishinuma, M. Absorption of Iodine by Polymers and Electrochemical Response of Polymer Film in Aqueous Solution of Iodine. Polym. J. 1989, 21, 403–408.
- Schreier, H.; Erdos, G.; Reimer, K.; König, B.; König, W.; Fleischer, W. Molecular Effects of Povidone-Iodine on Relevant Microorganisms: An Electron-Microscopic and Biochemical Study. Dermatology 1997, 195, 111–116.
- Berkelman, R.L.; Holland, B.W.; Anderson, R.L. Increased Bactericidal Activity of Dilute Preparations of Povidone-Iodine Solutions. J. Clin. Microbiol. 1982, 15, 635–639.
- Rösner, H.; Möller, W.; Groebner, S.; Torremante, P. Antiproliferative/Cytotoxic Effects of Molecular Iodine, Povidone-Iodine and Lugol’s Solution in Different Human Carcinoma Cell Lines. Oncol. Lett. 2016, 12, 2159–2162.
- Piérard, G.E.; Piérard-Franchimont, C.; Arrese, J.E. Povidone-Iodine Wash Solutions in the Prevention of Superficial Fungal Infections; Predictive Evaluation Using the Corneofungimetry Bioassay. Eur. J. Clin. Pharmacol. 1997, 53, 101–104.
- Yu, H.; Tak-Yin, M. The Efficacy of Povidone-Iodine Pessaries in a Short, Low-Dose Treatment Regime on Candidal, Trichomonal and Non-Specific Vaginitis. Postgrad. Med. J. 1993, 69 (Suppl. S3), S58–S61.
- Gatti, S.; Cevini, C.; Bruno, A.; Penso, G.; Rama, P.; Scaglia, M. In Vitro Effectiveness of Povidone-Iodine on Acanthamoeba Isolates from Human Cornea. Antimicrob. Agents Chemother. 1998, 42, 2232–2234.
- Kawana, R.; Kitamura, T.; Nakagomi, O.; Matsumoto, I.; Arita, M.; Yoshihara, N.; Yanagi, K.; Yamada, A.; Morita, O.; Yoshida, Y.; et al. Inactivation of Human Viruses by Povidone-Iodine in Comparison with Other Antiseptics. Dermatology 1997, 195, 29–35.
- Asanaka, M. In Vitro Study on Inactivation of Various Viruses Including Human Immunodeficiency Virus (HIV) by PVP-I. Proc. First Asian/Pacific Congr. Antisepsis. 1988. Available online: https://cir.nii.ac.jp/crid/1570009750369814784?lang=en (accessed on 15 March 2022).
- Sriwilaijaroen, N.; Wilairat, P.; Hiramatsu, H.; Takahashi, T.; Suzuki, T.; Ito, M.; Ito, Y.; Tashiro, M.; Suzuki, Y. Mechanisms of the Action of Povidone-Iodine against Human and Avian Influenza A Viruses: Its Effects on Hemagglutination and Sialidase Activities. Virol. J. 2009, 6, 124.
- Anderson, D.E.; Sivalingam, V.; Kang, A.E.Z.; Ananthanarayanan, A.; Arumugam, H.; Jenkins, T.M.; Hadjiat, Y.; Eggers, M. Povidone-Iodine Demonstrates Rapid In Vitro Virucidal Activity Against SARS-CoV-2, The Virus Causing COVID-19 Disease. Infect. Dis. Ther. 2020, 9, 669–675.
- Liang, B.; Yuan, X.; Wei, G.; Wang, W.; Zhang, M.; Peng, H.; Javer, A.; Mendenhall, M.; Julander, J.; Huang, S.; et al. In-Vivo Toxicity Studies and In-Vitro Inactivation of SARS-CoV-2 by Povidone-Iodine In-Situ Gel Forming Formulations. bioRxiv 2020. bioRxiv:2020.05.18.103184.
- Garcia-Sanchez, A.; Peña-Cardelles, J.F.; Ruiz, S.; Robles, F.; Ordonez-Fernandez, E.; Salgado-Peralvo, A.O.; Balloch, J.; Simon, J.C. Efficacy of Pre-Procedural Mouthwashes against SARS-CoV-2: A Systematic Review of Randomized Controlled Trials. J. Clin. Med. 2022, 11, 1692.
- Hoekstra, M.J.; Westgate, S.J.; Mueller, S. Povidone-Iodine Ointment Demonstrates in Vitro Efficacy against Biofilm Formation. Int. Wound J. 2017, 14, 172–179.
- Muppalaneni, S.; Omidian, H. Polyvinyl Alcohol in Medicine and Pharmacy: A Perspective. J. Dev. Drugs 2013, 2, 1–5.
- Miao, Z.; Sun, Y.; Tao, Z.; Chen, Y.; Ma, Y.; Zhu, D.; Huang, X.; Zha, Z. Thermochromic Polyvinyl Alcohol-Iodine Hydrogels with Safe Threshold Temperature for Infectious Wound Healing. Adv. Healthc. Mater. 2021, 10, 2100722.
- Montaser, A.S.; Rehan, M.; El-Naggar, M.E. PH-Thermosensitive Hydrogel Based on Polyvinyl Alcohol/Sodium Alginate/N-Isopropyl Acrylamide Composite for Treating Re-Infected Wounds. Int. J. Biol. Macromol. 2019, 124, 1016–1024.
- Tang, Y.; Xu, Y.; Li, F.; Jmaiff, L.; Hrudey, S.E.; Li, X.-F. Nontargeted Identification of Peptides and Disinfection Byproducts in Water. J. Environ. Sci. 2016, 42, 259–266.
- Gao, Y.; Qiu, J.; Ji, Y.; Wawryk, N.J.P.; An, T.; Li, X.-F. Formation Mechanism of Iodinated Aromatic Disinfection Byproducts: Acid Catalysis with H2OI+. Environ. Sci. Technol. 2022, 56, 1791–1800.
- Prütz, W.A.; Kissner, R.; Koppenol, W.H.; Rüegger, H. On the Irreversible Destruction of Reduced Nicotinamide Nucleotides by Hypohalous Acids. Arch. Biochem. Biophys. 2000, 380, 181–191.
- World Health Organization/United Nations Children’s Fund (UNICEF)/International Council for Control of Iodine Deficiency Disorders. Review of Findings from 7-Country Study in Africa on Levels of Salt Idodization in Relation to Iodine Deficiency Disorders, Including Iodine-Induced Hyperthyroidism; WHO, UNICEF, ICCIDD: Geneva, Switzerland, 1996.
- Sharma, A.; Stan, M.N. Thyrotoxicosis: Diagnosis and Management. Mayo Clin. Proc. 2019, 94, 1048–1064.
- Aceves, C.; Mendieta, I.; Anguiano, B.; Delgado-González, E. Molecular Iodine Has Extrathyroidal Effects as an Antioxidant, Differentiator, and Immunomodulator. Int. J. Mol. Sci. 2021, 22, 1228.
- Nagataki, S. The Average of Dietary Iodine Intake Due to the Ingestion of Seaweeds Is 1.2 Mg/Day in Japan. Thyroid 2008, 18, 667–668.
- Farebrother, J.; Zimmermann, M.B.; Andersson, M. Excess Iodine Intake: Sources, Assessment, and Effects on Thyroid Function. Ann. N. Y. Acad. Sci. 2019, 1446, 44–65.
- Backer, H.; Hollowell, J. Use of Iodine for Water Disinfection: Iodine Toxicity and Maximum Recommended Dose. Environ. Health Perspect. 2000, 108, 679–684.
- World Health Organization. Vitamin and Mineral Requirements in Human Nutrition, 2nd ed; World Health Organization: Geneva, Switzerland, 2005.
- World Health Organization. Urinary Iodine Concentrations for Determining Iodine Status in Populations; World Health Organization: Geneva, Switzerland, 2013.
- Zimmermann, M.B.; Jooste, P.L.; Pandav, C.S. Iodine-Deficiency Disorders. Lancet 2008, 372, 1251–1262.
- Ristic-Medic, D.; Piskackova, Z.; Hooper, L.; Ruprich, J.; Casgrain, A.; Ashton, K.; Pavlovic, M.; Glibetic, M. Methods of Assessment of Iodine Status in Humans: A Systematic Review. Am. J. Clin. Nutr. 2009, 89, 2052S–2069S.
- Zicker, S.; Schoenherr, B. Focus on Nutrition: The Role of Iodine in Nutrition and Metabolism. Compend. Contin. Educ. Vet. 2012, 34, E1-4.
- Milagres, R.C.; de Souza, E.C.G.; Peluzio, M.; Franceschini, S.; Duarte, M.S.L. Food Iodine Content Table Compiled from International Databases. Rev. Nutr. 2020, 33, 1–12.
- Rohner, F.; Zimmermann, M.; Jooste, P.; Pandav, C.; Caldwell, K.; Raghavan, R.; Raiten, D.J. Biomarkers of Nutrition for Development—Iodine Review. J. Nutr. 2014, 144, 1322S–1342S.
- World Health Organization Guideline. In Fortification of Food-Grade Salt with Iodine for the Prevention and Control of Iodine Deficiency Disorders; World Health Organization: Geneva, Switzerland, 2014.
- UNICEF Worldwide, 89 per Cent of People Consume Iodized Salt. Available online: https://data.unicef.org/topic/nutrition/iodine/ (accessed on 15 March 2022).
- Chavasit, V.; Malaivongse, P.; Judprasong, K. Study on Stability of Iodine in Iodated Salt by Use of Different Cooking Model Conditions. J. Food Compos. Anal. 2002, 15, 265–276.
- Stansbury, J.; Saunders, P.; Winston, D. Promoting Healthy Thyroid Function with Iodine, Bladderwrack, Guggul and Iris. J. Restor. Med. 2012, 1, 83–90.
- Zimmermann, M.; Delange, F. Iodine Supplementation of Pregnant Women in Europe: A Review and Recommendations. Eur. J. Clin. Nutr. 2004, 58, 979–984.
- Leung, A.M.; Pearce, E.N.; Braverman, L.E. Iodine Content of Prenatal Multivitamins in the United States. N. Engl. J. Med. 2009, 360, 939–940.
- Hennessey, J.V. The Emergence of Levothyroxine as a Treatment for Hypothyroidism. Endocr. 2016 551 2016, 55, 6–18.
- Knezevic, J.; Starchl, C.; Tmava Berisha, A.; Amrein, K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function? Nutrients 2020, 12, 1769.
- Agrawal, V.; Ghaznavi, S.A.; Paschke, R. Environmental Goitrogens. In Encyclopedia of Endocrine Diseases; Elsevier: Amsterdam, The Netherlands, 2018; pp. 506–511.
- López-Moreno, M.; Garcés-Rimón, M.; Miguel, M. Antinutrients: Lectins, Goitrogens, Phytates and Oxalates, Friends or Foe? J. Funct. Foods 2022, 89.
- Gaitan, E. 9 Goitrogens. Baillieres. Clin. Endocrinol. Metab. 1988, 2, 683–702.
- Speck, U. X-ray Contrast Media: Overview, Use and Pharmaceutical Aspects; Springer: Berlin/Heidelberg, Germany, 2018.
- Bourin, M.; Jolliet, P.; Ballereau, F. An Overview of the Clinical Pharmacokinetics of X-ray Contrast Media. Clin. Pharmacokinet. 1997, 32, 180–193.
- Crivello, J.V. Diaryliodonium Salt Photoacid Generators. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 457–478.
- Krause, W. Iodinated X-ray Contrast Agents. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 9781118466, pp. 353–374.
- Zhibin, Y. FDA Approved Radiopharmaceuticals. Foreign Med. Sci. Sect. Radiat. Med. Nucl. Med. 2000, 24, 161–163.
- Bartolozzi, C.; Lencioni, R.; Caramella, D.; Palla, A.; Bassi, A.M.; Di Candio, G. Small Hepatocellular Carcinoma. Acta Radiol. 1996, 37, 69–74.
- Wallers, K.J.; McDermott, P.; James, W.B. Intravenous Cholangiography by Bolus Injection of Meglumine Iotroxamate and Meglumine Iodoxamate: A Comparative Trial of Two New Contrast Media. Clin. Radiol. 1981, 32, 457–459.
- Miszczuk, M.A.; Chapiro, J.; Geschwind, J.-F.H.; Thakur, V.; Nezami, N.; Laage-Gaupp, F.; Kulon, M.; van Breugel, J.M.M.; Fereydooni, A.; Lin, M.; et al. Lipiodol as an Imaging Biomarker of Tumor Response After Conventional Transarterial Chemoembolization: Prospective Clinical Validation in Patients with Primary and Secondary Liver Cancer. Transl. Oncol. 2020, 13, 100742.
- Karmaker, N.; Maraz, K.M.; Islam, F.; Haque, M.M.; Razzak, M.; Mollah, M.Z.I.; Faruque, M.R.I.; Ruhul, A. Khan Fundamental Characteristics and Application of Radiation. GSC Adv. Res. Rev. 2021, 7, 064–072.
- Shirakami, Y. Radioactive Iodine. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 9781118466, pp. 603–624.
- Zerdoud, S.; Giraudet, A.-L.; Leboulleux, S.; Leenhardt, L.; Bardet, S.; Clerc, J.; Toubert, M.-E.; Al Ghuzlan, A.; Lamy, P.-J.; Bournaud, C.; et al. Radioactive Iodine Therapy, Molecular Imaging and Serum Biomarkers for Differentiated Thyroid Cancer: 2017 Guidelines of the French Societies of Nuclear Medicine, Endocrinology, Pathology, Biology, Endocrine Surgery and Head and Neck Surgery. Ann. Endocrinol. 2017, 78, 162–175.
- Braghirolli, A.M.S.; Waissmann, W.; Da Silva, J.B.; Dos Santos, G.R. Production of Iodine-124 and Its Applications in Nuclear Medicine. Appl. Radiat. Isot. 2014, 90, 138–148.
- Piel, M.; Rösch, F. Radiopharmaceutical Chemistry; Springer: Berlin/Heidelberg, Germany, 2012; Volume 71.
- Crișan, G.; Moldovean-Cioroianu, N.S.; Timaru, D.-G.; Andrieș, G.; Căinap, C.; Chiș, V. Radiopharmaceuticals for PET and SPECT Imaging: A Literature Review over the Last Decade. Int. J. Mol. Sci. 2022, 23, 5023.
- Kondev, F.G.; Wang, M.; Huang, W.J.; Naimi, S.; Audi, G. The NUBASE2020 Evaluation of Nuclear Physics Properties. Chinese Phys. C 2021, 45, 030001.
- Rasmussen, T.; de Nijs, R.; Olsen, L.K.; Kamper, A.L.; Bang, L.E.; Frimodt-Møller, M.; Kelbæk, H.; Sørensen, S.S.; Kjær, A.; Feldt-Rasmussen, B.; et al. Renal 123I-MIBG Uptake before and after Live-Donor Kidney Transplantation. Diagnostics 2020, 10, 802.
- Qaim, S.M.; Scholten, B.; Neumaier, B. New Developments in the Production of Theranostic Pairs of Radionuclides. J. Radioanal. Nucl. Chem. 2018, 318, 1493–1509.
- Barca, C.; Griessinger, C.; Faust, A.; Depke, D.; Essler, M.; Windhorst, A.; Devoogdt, N.; Brindle, K.; Schäfers, M.; Zinnhardt, B.; et al. Expanding Theranostic Radiopharmaceuticals for Tumor Diagnosis and Therapy. Pharmaceuticals 2021, 15, 13.
- Spitzweg, C.; Dietz, A.; O’Connor, M.; Bergert, E.; Tindall, D.; Young, C.; Morris, J. In Vivo Sodium Iodide Symporter Gene Therapy of Prostate Cancer. Gene Ther. 2001, 8, 1524–1531.
- Boland, A.; Ricard, M.; Opolon, P.; Bidart, J.M.; Yeh, P.; Filetti, S.; Schlumberger, M.; Perricaudet, M. Adenovirus-Mediated Transfer of the Thyroid Sodium/Iodide Symporter Gene into Tumors for a Targeted Radiotherapy. Cancer Res. 2000, 60, 3484–3492.
- Chen, E.; Wang, J.; Zhang, H.; Zhang, Y.; Jia, C.; Min, X.; Liang, Y. Analysis of the Efficacy and Safety of Iodine-125 Seeds Implantation in the Treatment of Patients with Inoperable Early-Stage Non-Small Cell Lung Cancer. J. Contemp. Brachytherapy 2021, 13, 347–357.
- Pavlicek, W.; Walton, H.A.; Karstaedt, P.J.; Gray, R.J. Radiation Safety with Use of I-125 Seeds for Localization of Nonpalpable Breast Lesions. Acad. Radiol. 2006, 13, 909–915.
- Mansouri, M.; Shahbazi-Gahrouei, D. A Review on Theranostic Applications of Iodine Nanoparticles: Recent Findings and Perspectives. Nanomedicine J. 2021, 8, 234–240.
- Zimmermann, M.B. Iodine Deficiency Disorders and Their Correction Using Iodized Salt and/or Iodine Supplements. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; Volume 9781118466, pp. 421–431.
- Yoshida, S.; Ojino, M.; Ozaki, T.; Hatanaka, T.; Nomura, K.; Ishii, M.; Koriyama, K.; Akashi, M. Guidelines for Iodine Prophylaxis as a Protective Measure: Information for Physicians. Japan Med. Assoc. J. JMAJ 2014, 57, 113–123.
- Küpper, F.C.; Kroneck, P.M.H. Iodine Bioinorganic Chemistry. In Iodine Chemistry and Applications; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2014; pp. 555–589.
- Dreger, S.; Pfinder, M.; Christianson, L.; Lhachimi, S.K.; Zeeb, H. The Effects of Iodine Blocking Following Nuclear Accidents on Thyroid Cancer, Hypothyroidism, and Benign Thyroid Nodules: Design of a Systematic Review. Syst. Rev. 2015, 4, 126.
- Markou, K.; Georgopoulos, N.; Kyriazopoulou, V.; Vagenakis, A.G. Iodine-Induced Hypothyroidism. Thyroid 2001, 11, 501–510.
- World Health Organization. Protection of the Human Environment. Guidelines for Iodine Prophylaxis Following Nuclear Accidents; Update 1999; World Health Organization: Geneva, Switzerland, 1999; pp. 1–45.
