Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cell Biology
Malignant melanoma is an aggressive cancer of the skin and the leading cause of death from skin cancer. One major risk factor linked to melanoma development is exposure to UV radiation. Recent studies have demonstrated that alcohol consumption is positively linked with an increased risk of cancers, including melanoma.
- melanoma
- ethanol metabolism
- alcohol
- ethanol
- acetaldehyde
- alcohol dehydrogenase
- aldehyde dehydrogenase
1. Introduction
Cutaneous melanoma is an aggressive malignancy of the skin and a significant public health concern. Melanoma incidence continues to rise globally, placing a greater burden on industrialized countries [1,2,3,4,5]. In the United States, melanoma remains the fifth most common cancer, making up 6 and 5 percent of all new cancers in males and females, respectively [6,7]. Although melanoma mortality decreased from 2017 [8] to 2021 [9], the incidence continues to increase: approximately 99,780 new melanoma cases will be diagnosed in the United States in 2022 [6], almost doubling from 53,600 in 2002 [10]. The increased incidence of cutaneous melanoma has been hypothesized to be, in part, the result of improved screening and early detection. However, the incidence of advanced melanoma is also increasing, suggesting that risk factors for melanoma are on the rise [11,12,13].
Risk factors and conditions for the development of melanoma are categorized into three: (1) genetic risk factors, (2) phenotypic risk factors reflecting gene/environment interactions, and (3) social-environmental risk factors [14]. Genetic risk factors include family history, light skin/hair/eye color, DNA repair defects, and several melanoma risk genes, such as cyclin-dependent kinase (CDK) inhibitor 2A (CDKN2A), CDK4, BRCA1-associated protein-1 (BAP1), protection of telomeres 1 (POT1), and telomerase reverse transcriptase (TERT) [15,16]. Mutations in these tumor suppressor genes confer high susceptibility to melanoma. In contrast, some genetic factors, especially when interacting with phenotypic and environmental risk factors, have great significance in melanoma susceptibility. For example, melanocortin 1 receptor (MC1R) R (D84E, R142H, R151C, I155T, R160W, D294H) variants are associated with the fair skin and red hair color phenotype, which is prone to sunburn and has an increased risk of melanoma [15,16]. Phenotypic expressions of gene/environment interactions also include a personal history of skin cancer and numerous nevi [17,18,19,20,21,22]. While identifying these high-risk cohorts improves public health and clinical care management, genetic factors are unchangeable. Therefore, recognizing modifiable risk factors, such as social-environmental risk factors, is crucial from the clinical perspectives of patient outreach, education, and disease management.
The most notable social-environmental risk factors include ultraviolet (UV) exposure, tanning bed use, pregnancy, and chemical or carcinogen exposure [23,24,25,26]. Due to its strong genotoxic effects, melanoma development has been most commonly linked with UV radiation. Mutations caused by UV radiation account for >70% of the nucleotide mutations found in melanoma cases [27,28]. However, not all changes involved in melanoma incidence are UV-induced [29], and melanoma does not always occur in sun-exposed areas, a key difference from non-melanoma skin cancer [30,31]. Nearly one-third of melanoma cases are present in areas of the skin not usually exposed to UV light [31]. A small percentage of melanoma also occurs on mucosal surfaces, typically not exposed to the sun, and they tend to have a worse prognosis [32]. These findings suggest that UV exposure alone does not explain the sharply increased incidence of melanoma [7].
Pregnancy has been considered a trigger for melanoma since the 1950s [33,34]. A study of 1,309,501 maternities aged 15–44 years from 1994–2008 in New South Wales, Australia, found that the ratio of age-adjusted observed-to-expected rates for melanoma was 2.22 (95% CI = 2.05–2.41) [35,36]. While approximately one-third of melanoma cases in women are diagnosed during their childbearing age [37], these populations represent about 15% of melanoma cases. As melanoma incidence has increased similarly between males and females (1.90- and 1.81-fold increase from 2002 to 2022, respectively) [6,10], pregnancy alone does not explain the continued rise in melanoma cases. Other social-environmental risk factors such as older patients, organ transplant patients, and those with a history of immunosuppressive therapy are also conditions that have shown a significant correlation with aggressive melanoma, greater incidence of metastases, and lower survival rates [38]. These factors, however, are not modifiable.
Recent studies have shown links between melanoma incidence and other modifiable social-environmental factors such as obesity, tobacco use, and alcohol consumption. Obesity negatively impacts outcomes for surgically resected melanoma but leads to better outcomes when treated with immunotherapy [39,40]. However, the International Agency for Research on Cancer (IARC) found no evidence to correlate obesity and melanoma after reviewing more than 1000 epidemiological studies [41]. Linking tobacco use and increased risk of skin malignancies, especially melanoma, has been a topic of great investigation. However, the data remains unclear. While the IARC has declared smoking a cause of 18 cancers, cutaneous malignancies are not included in this data [42]. On the other hand, many studies have found a positive correlation between alcohol consumption and increased melanoma incidence.
2. Potential Roles of Ethanol on Melanoma Initiation and Progression
Absorption of orally administered alcohol beverages depends on ethanol concentration, blood flow, rate of ingestion and gastric emptying, beverage type, food intake, and the irritant properties of ethanol [84]. When ingested, ethanol is oxidized to toxic acetaldehyde (AcAH) by alcohol dehydrogenase (ADH) and then to acetic acid by mitochondrial aldehyde dehydrogenase 2 (ALDH2) (Figure 2, ethanol to a right direction) [84].
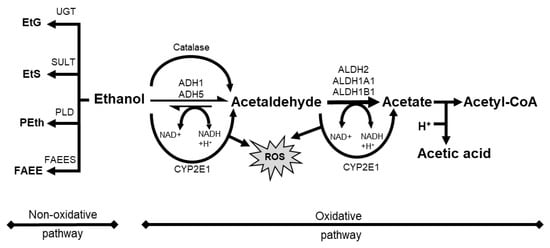
Figure 2. Schematic overview of alcohol metabolism with oxidative pathway and non-oxidative pathway. ADH, alcohol dehydrogenase; ALDH, aldehyde dehydrogenase; CYP2E1, cytochrome P 450 2E1; EtS, ethyl sulfate; FAEE, fatty acid ethyl ester; FAEES, fatty acid ethyl ester synthase; NAD, nicotinamide adenine dinucleotide; Peth, phosphatidyl ethanol; PLD, phospholipase D; ROS, reactive oxygen species; SULT, sulfotransferase; UGT, UDP-glucuronosyltransferase.
The putative benefits from alcohol intake come from various factors, including ethanol amount and ingredients [80]. For example, drinking small amounts of alcohol induces cardio-protective nitric oxide (NO) release in endothelial cells through ALDH2 activation [85]. Furthermore, non-ethanol active ingredients in alcoholic beverages (e.g., polyphenols) harbor anti-oxidant, anti-inflammatory, anti-carcinogenic, and other potential biological effects [86,87]. Rivera et al. [77] have found that white wine, but not red wine, was independently associated with an increased risk of cutaneous melanoma. A plausible explanation is that if the levels of AcAH in red and white wine are the same, the bioactive ingredients in red wine may offset its toxic effect.
However, the alcohol-mediated benefits disappear and are overridden by toxicity following heavy drinking and chronic consumption. In addition to the harmful intermediate metabolite AcAH, cytochrome p450 2E1 (CYP2E1) is induced and activated in response to high doses of ethanol, resulting in increased ROS (e.g., H2O2, hydroxide ion (OHˉ), and peroxide ion (O2ˉ)) [88]. IARC categorizes both ethanol and AcAH in alcoholic beverages as Group 1 carcinogens (carcinogenic to humans) [89]. Ethanol is associated with the tumor development of various cancers, such as liver and esophagus [76,90]. AcAH also induces GI tract tumors and lung cancer [91,92,93].
This chapter will review the roles of ethanol or AcAH in cellular biology and speculate on potential mechanisms connecting ethanol or AcAH to melanoma initiation and progression.
2.1. Roles of Ethanol or AcAH in Cellular Biology
Ethanol and/or AcAH induce oxidative stress, DNA damage, and lipid peroxidation, which activate protein kinases and signaling pathways implicated in glycolysis, fatty acid oxidation, inflammation, differentiation, angiogenesis, and metastasis, thereby creating a favorable microenvironment for tumor initiation and progression [94].
Both ethanol and AcAH promote oxidative stress. After ethanol uptake, ADH-catalyzed reactions in the cytosol and ALDH2-mediated reactions in the mitochondria reduce an NAD+/NADH redox ratio [84], regenerating NAD+ from NADH via the mitochondrial electron transfer system with concomitant ROS production [94].
AcAH is a highly reactive metabolite and a mutagen. AcAH-mediated DNA damage includes adduct formation, double-strand breaks, point mutations, DNA-DNA cross-links, sister chromatid exchanges, and chromosomal aberrations [95]. AcAH binds proteins involved in DNA repair and methylation, altering their structure and functions and promoting carcinogenesis [96,97,98]. AcAH also reacts with deoxyguanosine residues, leading to DNA modifications and lesions [99], impairing replication, transcription, and metabolism, and increasing mutation rates and cell death [99].
Another mutagenic effect of ethanol and/or AcAH is mediated by CYP2E1 induction, resulting in increased ROS generation. ROS-induced lipid peroxidation products such as malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) are genotoxic, thus generating mutagenic DNA adducts [100]. In addition, following ethanol intake, hybrid adducts can be generated in the affected tissues, such as the hybrid MDA and AcAH-protein adducts, increasing the tumorigenic potential of individual adducts by reducing NAD+ to NADH [100,101].
2.2. Roles of Ethanol or AcAH in Tumor Biology
The abovementioned changes activate multiple signal transduction mechanisms, such as cAMP/PKA signaling [102,103,104], mitogen-activated protein kinase (MAPK) signaling [105], PI3K/Akt signaling [106,107], and Wnt/β-catenin signaling [108] (Figure 3). For example, ethanol stimulates cAMP-mediated PKA activation [104,109,110], and PKA activation has tumor-promoting or tumor-suppressive effects [111,112]. Ethanol also activates PKC [113]. Activated PKC induces RAS, RAF, or MEK 1/2 activation, leading to the activation of MAPK signaling to proliferate mammalian cells [114] and PI3K/Akt signaling to regulate cell survival and proliferation [115]. Furthermore, chronic alcohol consumption upregulates Wnt/β-catenin signaling, leading to tumor formation and progression in the liver cancer model [108] and tumor invasion in the colon cancer model [116]. Ethanol also induces JNK1-dependent upregulation of Brf1 expression and RNA Pol III gene transcription in breast cancer [117] and ethanol-induced liver cancer [118]. In addition, ethanol-induced genotoxic stress and oxidative stress can activate p53, which in turn activates sphingolipid-metabolizing enzymes, resulting in the accumulation of the ceramide metabolite sphingosine-1-phosphate (S1P), a promoter of the proliferation and inflammation in carcinogenesis [119]. These signaling pathways are key in initiating cellular responses implicated in tumorigenesis and progression, such as proliferation, differentiation, development, inflammation, survival, and cell death.
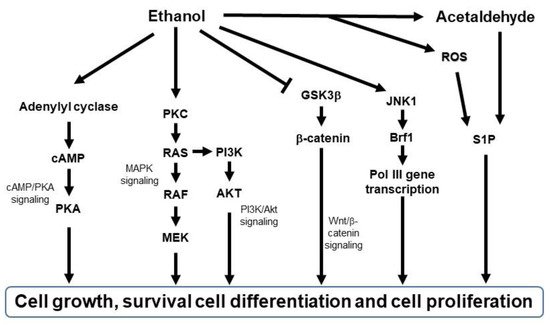
Figure 3. Schematic diagram of signaling pathways activated by ethanol. Brf1, TFIIB-related factor 1; AKT, protein kinase B; cAMP, cyclic adenosine monophosphate; GSK3β, glycogen synthase kinase 3 beta; JNK1, c-Jun N-terminal kinase; MAPK, mitogen-activated protein kinase; MEK, MAPK/Erk kinase; PI3K, phosphatidylinositol-3-kinase; PKA, protein kinase A; PKC, protein kinase C; RAF, rapidly accelerated fibrosarcoma; RAS, rat sarcoma virus; ROS, reactive oxygen species; S1P; sphingosine-1-phosphatase.
Lastly, ethanol and its metabolites damage various types of progenitor/stem cells, such as embryonic stem cells and tumor-initiating cells, impairing cell differentiation and genomic stability, leading to cellular aging and carcinogenesis [120,121].
2.3. Roles of Ethanol or AcAH in Skin Biology
Most research on alcohol consumption is centered around its effects on the liver and gastrointestinal tract but rarely on the skin [122,123]. Nonetheless, acute and chronic alcohol consumption induces various skin changes. Alcohol flush reaction is a typical acute response in which the rapid elevation of AcAH in the blood after drinking alcoholic beverages leads to erythema on the face, neck, and even the entire body [124], and this reaction occurs not only in ALDH2-deficient Asians but also in Caucasians and Native Americans [125,126]. Chronic alcohol consumption induces many skin changes such as jaundice, hyperpigmentation, and telangiectasis, which are often considered clinical manifestations of hepatic and vascular consequences [127,128].
However, it is crucial to consider ethanol’s direct effects on skin cells. For a long time, it has been known that ingested ethanol is secreted by the eccrine glands of human skin [129,130], with an almost equal concentration to blood concentration [131]. Ethanol can directly influence skin structure by disrupting skin cell membranes that form an effective barrier [132]. Furthermore, many skin microbiotas such as Cutibacterium acnes, Staphylococcus aureus, and Staphylococcus epidermidis possess ADH to convert ethanol to AcAH [133]. Therefore, it is likely that ethanol and AcAH exposure in the skin affects skin cell biology. The fact that chronic alcohol consumption causes esophageal melanosis in alcoholics [134,135,136] and skin hyperpigmentation in the epidermis of the paw and tail in mice [137,138,139] suggests that chronic alcohol ingestion promotes melanocyte changes.
In addition to oxidative metabolism, a smaller fraction of ethanol undergoes a non-oxidative route of metabolism (Figure 2, ethanol to a left direction). It results in the enzymatic conjugation of ethanol to endogenous metabolites, yielding ethyl glucuronide (EtG), ethyl sulfate (EtS), phosphatidylethanol (PEth), and fatty acid ethyl esters (FAEE) [140]. While only a minor fraction of total ethanol undergoes these metabolic pathways, the resulting metabolites such as EtG remain in the blood, urine, and hair for a long time (up to several months in hair). Therefore, these biometabolites are suitable biomarkers for recent alcohol use and abuse in clinical and forensic settings [141,142]. EtG and EtS are involved in toll-like receptor signaling, oxidative stress, and lower energy metabolism [143]. In contrast, PEth and FAEE interfere with cellular signaling pathways and disrupt organelle function [140]. Therefore, these biometabolites can also contribute to direct ethanol toxicity in organs with a limited oxidative capacity [140].
Furthermore, chronic alcohol consumption impairs skin immunology directly and/or indirectly by altering skin Langerhans cells [144,145], migrating dendritic cells [146], and multiple skin T cells [146].
Due to our use of alcohol-containing products and alcoholic beverages, these direct and indirect effects of ethanol and AcAH on our skin may not be easily eliminated. Together with the impact of skin microorganisms and potentially synergistic influences from sun exposure, these diverse effects on our skin may likely contribute to activating and transforming skin cells.
2.4. Does Ethanol or AcAH Affect Melanoma Initiation?
While mutagenic effects of ethanol and/or AcAH have been demonstrated in other cancers, their contribution to melanoma remains largely elusive.
Alcohol consumption lowers carotenoid levels in the plasma [147]. Carotenoids such as beta-carotene or lycopene can act as anti-oxidants to scavenge singlet molecular oxygen and peroxyl radicals generated during photo-oxidation and reduce solar light simulator-induced erythema [148]. AcAH is also a highly reactive chemical that serves as a photosensitizer [149]. Therefore, Darvin et al. hypothesized that alcohol consumption increased photosensitivity in human skin and recruited six male Caucasian volunteers [150]. They reported a decrease in the skin carotenoid concentration and minimal erythema dose (MED) after consuming 1 mL of ethanol/kg of body weight (corresponding to ~150 mL of vodka). However, these decreases were not observed after a combined intake of alcohol and ~1 liter of orange juice, rich in carotenoids. Low carotenoid levels increase erythema following UV exposure [148,151,152], and carotenoid consumption in the diet has been associated with decreased melanoma risk [59]. Therefore, these data suggest that alcohol consumption is associated with increased melanoma risk by lowering carotenoid levels and increasing UV sensitivity, indicating the synergistic effects of ethanol with UV exposure.
To elucidate the synergistic effects of ethanol and UV exposure on skin cells, Brand et al. used mouse models and human skin explants [153]. They demonstrated that combined ethanol consumption and UV exposure increased immune dysfunction and skin damage by decreasing DNA repair capacity and inhibiting protective mechanisms such as melanin production and anti-oxidants against UV exposure.
However, the mechanisms of melanoma development induced by UV light and ethanol are unclear. As mentioned in Section 3.1, excessive ethanol induces a complicated cellular response, from oxidative stress and persistent inflammation to mitochondrial DNA damage and signaling pathway activation [154,155], all implicated in tumor development. Among these pathways, MAPK signaling is one of the major pathways activated by mutations and is critical for melanoma initiation [156].
Strickland et al. reported that treating C3H/HeNCr mice with UV light and topical ethanol application (25% in water) thrice weekly for about 30 weeks induced primary cutaneous melanoma in 20 to 30% of the mice [157]. The frequency of melanoma induction was similar to that of squamous cell carcinoma. Topical ethanol application alone did not induce melanoma, and UV alone rarely induced melanoma. Interestingly, these melanoma tumors possessed Nras mutations at codons 13 and 19 in both tumors [158], which occurred at pyrimidine dimer sites, exhibiting a C to T transition on the non-transcribed strand at codon 13 and transcribed strand at codon 19, implicating UV-associated changes [159]. BRAF and NRAS are two major genes often mutated in human melanoma and are associated with melanoma initiation and progression [160]. Active NRAS mutations induce both MAPK and PI3K/Akt signaling [161]. Furthermore, these two mouse tumors and the cell lines had either a deletion in exon 2 of the Ink4a/Arf gene or an interstitial deletion of the long arm of chromosome 4 (where the Ink4a/Arf gene resides), similar to genetic changes of human melanoma for CDKN2A, encoding p16INK4a and p19ARF [162].
While UV is more frequently associated with the development of non-melanoma skin cancer than melanoma, it is unclear how the combination of ethanol and UV induced a relatively equal number of melanoma tumors compared to squamous cell carcinoma [157]. As ethanol stimulates cAMP-mediated PKA activation [104,109,110], this signaling may rewire β-catenin to activate the transcription of CREB target genes, including microphthalmia-associated transcriptional factor (MITF) [163], a master regulator of melanocyte biology [164,165]. Alterations in the MITF gene and pathway are associated with a higher risk of melanoma initiation [166,167]. MITF is regulated by several other transcription factors, including SOX10, CREB, Pax3, Tyro3, and TCF/LEF. The activation of the BRAF V600E/ERK pathway can also enhance the expression of MITF by directly phosphorylating MITF at Ser73 or activating CREB through MSK [164,168,169,170]. The PI3K/Akt signaling pathway regulates MITF through inactivating GSK-3β or cooperating with RAS/RAF/MEK/ERK signaling. In addition, MITF is a target of the p38/MAPK signaling but can be inhibited by the JNK/MAPK pathway, suggesting that the regulation of MITF is accomplished by various MAPK signaling pathways [171,172].
Considering these data collectively, it is likely that such signaling pathways are critical components of ethanol-induced carcinogenesis in some cancers, including melanoma.
2.5. Does Ethanol or AcAH Affect Melanoma Progression?
Several studies have reported the biological effects of chronic alcohol consumption on melanoma progression and metastasis. Tan et al. found that ethanol-treated B16F10 melanoma tumors exhibited enhanced angiogenesis through increased vascular endothelial growth factor (VEGF) expression, contributing to tumor progression [173]. On the other hand, Meadow’s research team from Washington State University studied alcohol’s impact on tumor metastasis in C57BL/6 mice using B16BL6 melanoma, a derivative of B16F10 with a more invasive and metastatic phenotype [174,175,176,177]. Melanoma cells were injected subcutaneously to assess spontaneous metastasis and intravenously to assess experimental metastasis. While pretreating tumor cells in vitro or in vivo with ethanol enhanced experimental metastasis [174], pretreating mice with ethanol (10–20% (w/v) ethanol for >4 weeks) inhibited spontaneous and experimental metastases [174,177]. These data suggest that ethanol directly potentiates the metastatic capacity of melanoma cells. They also indicate that the host environment at the tumor injection determines the ethanol’s effect on tumor metastasis. Interestingly, survival times were significantly shorter in mice pretreated with ethanol, despite having fewer metastases [174], implicating the detrimental effects of ethanol in tumor-bearing mice.
Several mechanisms could be involved in alcohol-mediated melanoma progression and metastasis. For example, ethanol disturbs mitochondrial dynamics [178] by increasing mitochondrial fission and reducing their fusion [179], and altered mitochondrial dynamics can promote tumor migration and progression in human melanoma [180]. ROS from mitochondria upregulates hypoxia-inducible factor-1α, inducing matrix metalloproteinases and VEGF [181], important for tumor invasion. Furthermore, DNA and ATP leaked from damaged mitochondria activate inflammasomes [181,182], reshaping the tumor microenvironment and immune infiltration to support tumor progression and drug resistance, as shown in our previous reports [183,184,185].
Another consequence of chronic and acute alcohol consumption is interference with immune cell numbers and function, which may facilitate melanoma progression and metastasis [163,186]. B16BL6 melanoma-bearing mice exposed to chronic ethanol showed fewer mature B cells, CD8+ T cells, and NK cells in circulation due to ethanol-induced downregulation of S1P/S1P receptor 1 signaling resulting in decreased egress of lymphocytes from the spleen [187]. Chronic ethanol administration also impairs the trafficking of NK cells to lymph nodes, resulting in a decreased number and percentage of NK cells in the draining nodes [188]. CD8+ T cells and NK cells are important in inhibiting tumor progression. Moreover, chronic ethanol exposure in mice impairs antigen-specific response to melanoma cells by inhibiting the proliferation of memory T cells, reducing IFN-γ producing CD8+ T cells, and increasing myeloid-derived suppressor cells [189].
Ethanol can also upregulate the expression of nerve growth factor receptor (NGFR/CD271) through NF-κB signaling in human melanoma cells [190]. NGFR expression in melanoma cells is associated with increased metastasis and long-term growth [191,192]. NGFR signaling also plays a critical role in acquired melanoma resistance to BRAF/MEK inhibitors [193,194,195,196]. VEGF expression, which contributed to angiogenesis in the melanoma mice model, is also reported to induce immune resistance by affecting myeloid-derived suppressor cells, dendritic cells, T regulatory cells, and cytotoxic T cells [173,197]. In addition, NGFR expression induced by ethanol is linked to immunosuppressive functions and anti-PD-1 immunotherapy resistance in melanoma [198,199,200].
Together, the accumulated data suggest a link between chronic alcohol consumption and melanoma progression. Further studies are required to ascertain these findings, especially in human melanoma patients, and elucidate the underlying mechanisms and biology. In addition to the factors mentioned above, the role of other potential factors such as genetic instability, metabolic rewiring, and skin microbiota need to be determined for a comprehensive understanding of alcohol-associated melanoma progression.
This entry is adapted from the peer-reviewed paper 10.3390/cancers14205010
This entry is offline, you can click here to edit this entry!
