Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
NUT carcinoma is a rare, highly lethal cancer characterized with the rearrangement of the nuclear protein in testis (NUT) gene on chromosome 15q14, which primarily occurs in the midline organs. Primary pulmonary NUT carcinoma (NC) lacks characteristic clinical manifestations, which leads to the high rate of misdiagnose and nonstandard treatment.
- NUT carcinoma (NC)
- primary pulmonary NC
- chemoradiotherapy
1. Introduction
Nuclear protein of the testis (NUT) is a protein translated by the NUTM1 gene (NUT family member 1, located on the long arm of chromosome 15) whose expression should be restricted to the testis and ovary. Nuclear protein of the testis carcinoma (NC), also known as NUT midline carcinoma (NMC), is a rare and highly aggressive malignant epithelial tumor that typically affects midline organs, including the nasal cavity, palate and mediastinum. The pathogenesis of NC is currently unclear, which is often thought to be related to the NUT-mediated genome-wide histone modification that alters the expression of oncogenes or tumor suppressor genes. Molecular genetic studies have demonstrated recurrent fusions involving the NUT gene on chromosome 15q14 [1]. Related cases have reported fusions involve BRD4 on chromosome 19p13.1. Frequently, BRD3 and NSD3 have also been reported. The prognosis of NC is often extremely poor. A report showed [2] that the disease progresses rapidly to death in most cases, with a median overall survival (OS) of only 6.7 months and a 2-year progression-free survival (PFS) of 9%.
The World Health Organization (WHO, Geneva, Switzerland) included primary pulmonary NC in the classification of other undifferentiated cancers of lung malignancies in 2015. However, less than 100 cases of primary pulmonary NC have been reported worldwide. Due to the rarity, the occurrence of the primary pulmonary NC is often ignored by clinicians, and its clinical understanding is not yet profound. The relevant clinical characteristics, imaging and pathological features of primary pulmonary NC, as well as the treatment methods and prognosis for a total of 55 patients, were summarized from 35 articles in order to deepen the understanding and hopefully help in the clinical identification and treatment of the disease.
2. Pathological Characteristics
Among all the literatures, 47 cases were described in detail regarding their histological features of the primary or metastatic lesions at the surgical specimens or fine needle aspiration (FNA) samples. In summary, sheets of undifferentiated or poorly differentiated (93.75% 30/32) cells with squamous differentiation (n = 15) and abrupt keratinization (n = 13) were typically observed (32 cases mentioned the degree of cell differentiation). The cytological morphological features included small-to-intermediate-sized (n = 7) elliptical cancer cells, with irregular nuclei in a nested arrangement, and overlapped nuclei (n = 2) could be seen in a minority of the cases. Occasionally, naked nuclei (n = 3) were seen around clusters and debris. Numerous tumor cells (n = 25) possessed prominent nucleoli (n = 25), scanty cytoplasm (n = 7) and a high nuclear-to-cytoplasmic (N/C) ratio (n = 4). The cells were predominantly scattered in a necrotic background (n = 15), with a nest-like distribution (n = 11) in which a distinct neutrophil infiltration (n = 8) was present. Apoptosis and identifiable mitotic figures (n = 12) could be found in some tumor cells.
Immunohistochemistry (IHC) showed that all specimens were positive for NUT, except for eight cases not mentioned. Most (49) cases specifically described the results of IHC staining: 30 positive for P63 (61.2% 30/49), 16 positive for P40 (32.7% 16/49), 6 positive for TTF-1 (12.2% 6/49) and 5 positive for CD56 (10.2% 5/49). In addition, other epithelial markers (CK5/6, CK7, AE1/AE3, CAM5.2, EMA, etc.) (69.4% 34/49) and neuroendocrine markers (Syn, NSE, CgA, etc.) (20.4% 10/49), as well as other markers such as P53, CD99, LCA, CD138, Vimentin, BCL-2 and HHF-35, can also be discovered as positive. Nineteen cases were positive for Ki-67 (range 25–80%), of which eighteen cases were reported above 30% (94.7% 18/19), demonstrating a generally high but variable proliferation index, as measured by Ki-67 (Figure 1).
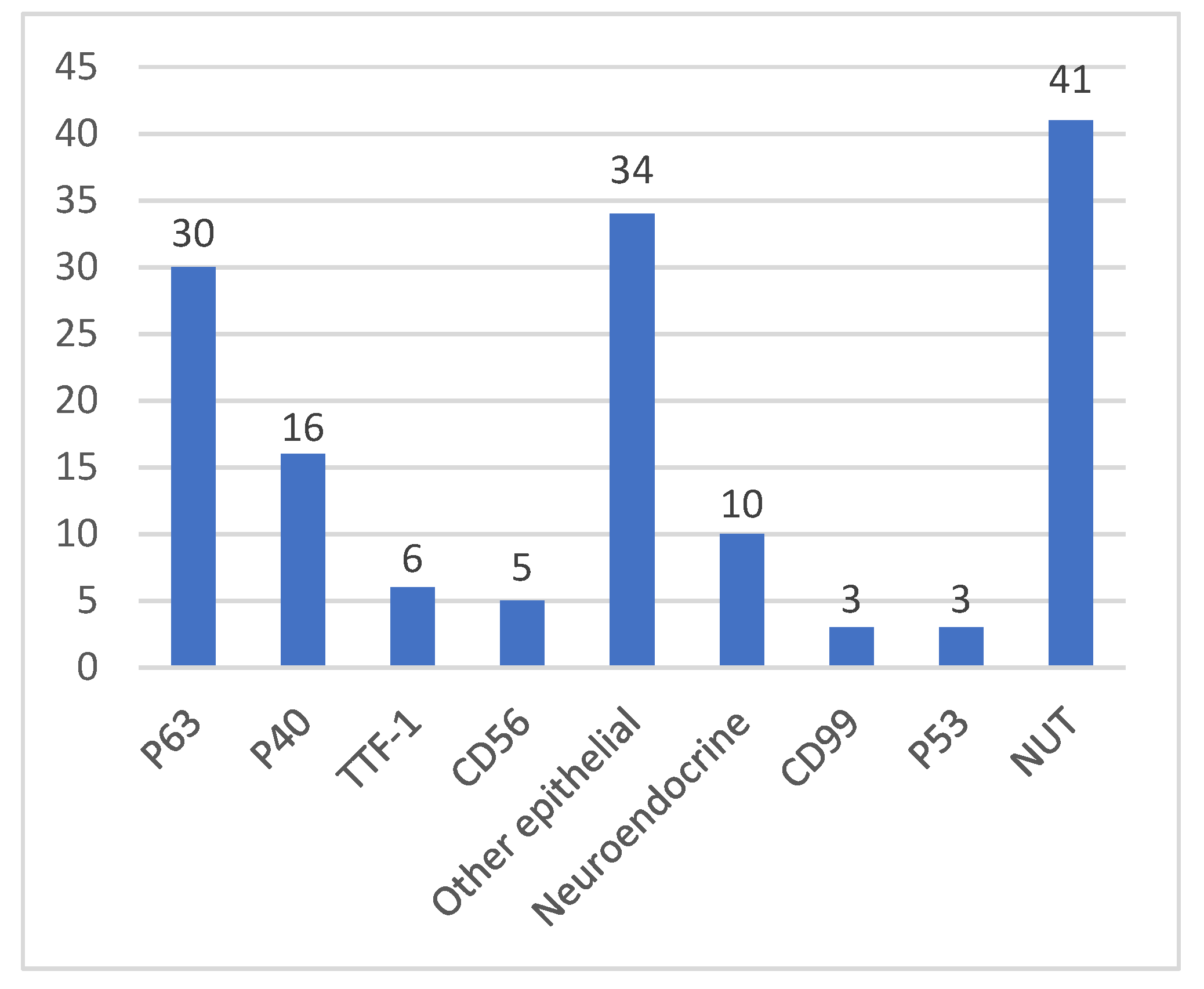
Figure 1. The mainly positive signals of IHC.
In 36 cases, modern molecular biotechnology was used to detect the gene fusion, including fluorescence in situ hybridization (FISH) (n = 19), next-generation sequencing (NGS) (n = 8), reverse transcriptase-polymerase chain reaction (RT-PCR) (n = 3), comprehensive genomic profiling (CGP) (n = 3) and other diagnosis approaches (n = 5). The majority of these cases manifested a tumor with chromosomal translocation, which forms the BRD4-NUT fusion oncogene (n = 16), BRD3-NUT (n = 4), NSD3-NUT (n = 3), NUT-variant (n = 1), CHRM5-NUTM1 (n = 1) and other NUTM1 rearrangements (n = 5). DDR2, CSF1R, DAXX, RUNX1 somatic mutations, ATXN3 ZNF429 mutations and EGFR exon19 deletion were also identified by NGS. Due to the rarity of NC, these methods are not routinely used in all cancer patients, resulting in the misdiagnosis or delayed identification of this disease.
3. Treatments and Outcomes
Forty cases documented the OS since diagnosis. The median OS in patients with primary pulmonary NC was 4.4 months (range 1 day–26.7 months), and the mean OS was 6.21 months.
Fifty cases described the complete treatment course. Five patients were untreated with just a mean OS of 1.3 months. Eleven patients had surgical resection of the primary lesion (22% 11/50), of which seven patients operating alone had a mean OS of 3.54 months. For the other four patients who received neoadjuvant therapy and postoperative adjuvant chemoradiotherapy, three of them were still alive at the time of reporting, and one of them had an 8-month OS. Patients receiving neoadjuvant therapy or postoperative adjuvant chemoradiotherapy demonstrated an obvious improvement in OS, whereas surgery alone could only have a limited benefit.
Chemotherapy (platinum-based regimen constituted the majority) was chosen by 33 of the unoperated patients (66% 33/50), with a mean OS of 7.32 months, longer than the mean OS of untreated and surgically only patients. Of these, 16 patients were treated with chemotherapy alone, of whom two were alive at the time of reporting, and one did not record the survival time, leaving a mean OS of 5.58 months. Eight patients opted for chemoradiotherapy (applied concurrent chemoradiotherapy or sequential chemoradiotherapy as the first-line therapy), with a mean OS of 13.2 months for the six patients who recorded the survival time, and four of them reported an OS more than 12 months (12.9, 16, 18 and 26.7 months, respectively). On the basis of chemotherapy alone, immunotherapy was administered to three cases: the OS of one case was unclear, and the remaining two cases reported OS of 3 and 8 months, respectively. Seven cases applied immunotherapy in the posterior lines. As most immunotherapies were coupled with other treatments, their efficacy could not be determined with certainty. Six patients were treated with bromodomain and extra-terminal motif inhibitors (BETi) or histone deacetylase inhibitors (HDACi) for the posterior-line treatment, with a mean OS of 7.45 months. There was no significant therapeutic benefit found in this therapeutic option, which may due to the misdiagnosis of most patients and the advanced disease at the time of the confirmed diagnosis. Patients with primary pulmonary NC have a clinical response to chemotherapy, especially combined with radiotherapy, suggesting that the tumor is sensitive to radiotherapy. The effect of a combination with immunotherapy is uncertain. The details are in Table 1.
Table 1. Treatments and outcomes.
| Treatment | Recorded/Total (n) | Mean OS (Months) |
|---|---|---|
| Untreated | 5/5 | 1.3 |
| Surgery only | 11/11 | 3.54 |
| Surgery combined with adjuvant therapy | 1/4 | (8) * |
| Chemotherapy only | 13/16 | 5.58 |
| Chemoradiotherapy | 6/8 | 13.2 |
| Chemotherapy combined with immunotherapy | 2/3 | 5.5 |
* Only one case in this group with an OS of 8 months.
The TP regimen (Taxanes + Platinum) was chosen as the most common chemotherapy (30.3% 10/33), followed by the EP regimen (Etoposide + Platinum) (18.2% 6/33), DP (Docetaxel + Platinum), AP (Pemetrexed + Platinum), etc. For the second-line and third-line treatments, the regimen included platinum-containing chemotherapy; single-agent chemotherapy; dual or single-agent immunotherapy (Pembrolizumab, Nivolumab, Bevacizumab, Atezolizumab, etc.) and targeted therapy (Gefitinib, Apatinib or Anlotinib); palliative radiotherapy was also chosen, but the effect was moderate. Only 4 of the 50 patients were treated to the fourth line; all of them had received chemotherapy, radiotherapy, immunotherapy and targeted therapy, and all four had an OS of longer than 12 months.
Some (n = 23) cases were misdiagnosed initially and were diagnosed with further examination. Thirteen cases were misdiagnosed as non-small cell lung cancer (NSCLC) (13/23) at the early diagnose, most of which were misdiagnosed as lung squamous cell carcinoma (SCC). Moreover, some have been incorrectly diagnosed with small cell lung cancer (SCLC), neuroendocrine tumor, blood disease, sarcoma and other diseases.
This entry is adapted from the peer-reviewed paper 10.3390/curroncol29100536
References
- French, C.A.; Ramirez, C.L.; Kolmakova, J.; Hickman, T.T.; Cameron, M.J.; Thyne, M.E.; Kutok, J.L.; Toretsky, J.A.; Tadavarthy, A.K.; Kees, U.R.; et al. BRD-NUT oncoproteins: A family of closely related nuclear proteins that block epithelial differentiation and maintain the growth of carcinoma cells. Oncogene 2008, 27, 2237–2242.
- Bauer, D.E.; Mitchell, C.M.; Strait, K.M.; Lathan, C.S.; Stelow, E.B.; Lüer, S.C.; Muhammed, S.; Evans, A.G.; Sholl, L.M.; Rosai, J.; et al. Clinicopathologic features and long-term outcomes of NUT midline carcinoma. Clin. Cancer Res. 2012, 18, 5773–5779.
This entry is offline, you can click here to edit this entry!
