Senescence Induction
Induction of senescence is influenced by various factors, such as DNA damage, telomere shortening, hypoxia, nutrient deficiency, cell stress, oncogene activation, mitochondrial dysfunctions [
3]. There is also a possibility of stimulating senescence through cellular metabolism, regulation of apoptosis, response to unfolded protein (UPR), and DNA damage response (DDR) [
13].
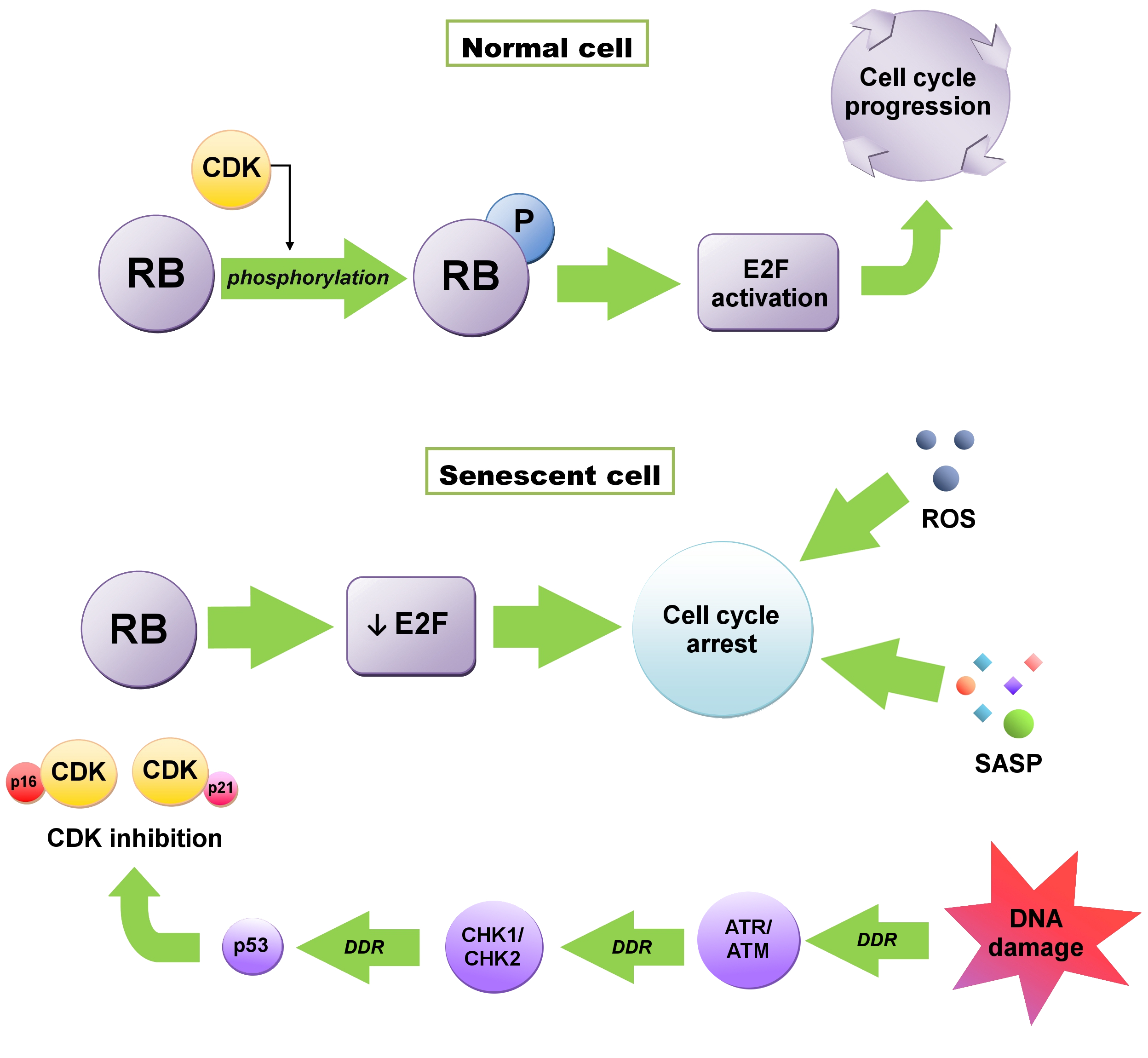
Initiation of senescence is associated with the cell cycle, when a cell from the G1 phase, instead of going into the synthesis (S) phase, goes into the G0 phase, resulting in cell division inhibition. Activation of this checkpoint usually depends on DNA damage and telomere shortening [
6]. Maintenance of this state, which is extremely important in anticancer therapy, is influenced by the cyclin-dependent kinase (CDK) inhibitors—P16
INK4A (CDKN2A) and P21
WAF1/CIP1 (CDKN1A) proteins—regulated by both the suppressor protein P53 and retinoblastoma proteins (RB) (
Figure 1) [
14,
15]. RB1 protein, as well as P107 (RBL1) and P130 (RBL2), are phosphorylated by CDKs. The phosphorylation weakens their ability to repress E2F transcription factors, crucial to cell cycle progression [
3]. In senescent cells, RB proteins are constantly activated due to the accumulation of the CDK4/6 inhibitor P16 and the CDK2 inhibitor P21. E2F transactivation is inhibited and consequently, cell cycle arrest occurs. This state is maintained by the SASP, heterochromatinization of E2F target genes and reactive oxygen species (ROS) and cannot be reversed by P53 or RB inactivation [
3,
16].
1. Replicative Senescence
According to the Hayflick theory, cells’ ability to replicate is limited [
17]. After reaching the limit, they become senescent cells—alive and metabolically active, but unable to divide. The main factor causing replicative senescence is the shortening of telomeres and the lack of telomerase responsible for their extension [
18,
19]. Telomeres are located at the ends of the chromosomes and are tandem repeats of TTAGGG nucleotides, stabilized by the Shelterin protein complex [
18,
19]. The majority of cells (except for stem and cancer cells) do not express telomerase responsible for maintaining telomere length [
3]. With each replication, the length of telomeres decreases [
6]. Eventually, the free end of the chromosome is exposed, which is perceived as a double-strand DNA break (DSB). DSBs activate the DDR [
4].
2. Stress–Induced Senescence
As mentioned before, senescence is associated with DDR. DNA damage caused by the above-described telomere shortening, induction of an oncogene, as well as damage due to the oxidative stress, external factors, and chemotherapeutic agents result in a cellular response [
6]. A strong inducer of DDR is also the sugar-phosphate DNA backbone damage—caused by, among others, ionizing radiation (IR) or topoisomerase inhibitors—which may cause DSBs [
20]. In case of constant DNA damage signaling, DSB contributes to the enhanced secretion of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and onset of inflammation [
21]. Diminished selective autophagy of GATA binding protein 4 (GATA4)—transcriptional factor—also contributes to the induction of DDR-dependent senescence and inflammation. During senescence—due to the action of ataxia telangiectasia mutated kinase (ATM) and ataxia telangiectasia and Rad3-related kinase (ATR)—activation of P16
INK4A and P53 pathways occurs. As a result, p62-dependent autophagic GATA4 degradation is inhibited. Activation of nuclear factor kappa B (NF-κB) occurs, which leads to the SASP initiation [
22]. This process seems to be independent of P16
INK4A and P53 [
20]. Furthermore, telomere related factors such as protection of telomeres 1 (POT1) and telomeric repeat-binding factor 2 (TRF2) may impair the activity of DDR via inhibiting ATM and ATR kinases involved in the cell response to DNA damage [
23,
24]. Eradication of TRF2 or POT1 from telomeric DNA leads to DDR [
25].
Figure 1. Retinoblastoma (RB)-dependent cell cycle arrest. In normal cells RB is phosphorylated by cyclin-dependent kinases (CDKs). Enhancement of E2F transcription factor activity occurs, which is required for cell cycle progression. In senescent cells, CDKs are inhibited by P16 or P21, which can be activated as a result of DNA damage response (DDR) through ataxia telangiectasia and Rad3-related kinase (ATR)/ataxia telangiectasia mutated kinase (ATM) → checkpoint kinase 1 /checkpoint kinase 2 (CKH1/CHK2) → P53 pathway. E2F repression occurs, which leads to the cell cycle arrest maintained by the senescence-associated secretory phenotype (SASP) and reactive oxygen species (ROS).
Regardless of the inducer, the DDR mechanism is based on the activation of the kinase cascade (first ATR and ATM kinases, then checkpoint kinase 1 (CHK1) and kinase 2 (CHK2)). ATM responds to the DNA DSB and activates the DNA repair mechanism via H2A histone family member X (H2AX) phosphorylation—a crucial step of the production of DNA repair factors (Nijmegen breakage syndrome 1 protein (NBS1), mediator of DNA damage checkpoint 1 (MDC1)/nuclear factor with BRCT domains protein 1 (NFBD1), P53 binding protein 1 (53BP1) and checkpoint proteins. Phosphorylated H2AX (γH2AX) also controls CHK1 and CHK2 phosphorylation, which transmits the signal to P53/P51 proteins [
4,
26]. Eventually, the P53 protein is phosphorylated, and its activation leads to cell cycle arrest [
25,
27]. It has been proven that inhibition of DDR, and more specifically ATR, ATM, CHK1, CHK2 kinases, leaves an open door for senescent cells to re-enter the cell cycle [
25,
28].
As a result of DDR activation, the cell may enter a state of apoptosis or senescence. The path it takes depends on the degree of DNA damage and the possibility of its repair. Initiating cellular senescence through DDR activation is a crucial process in chemotherapy and radiotherapy [
6]. In cancer, tumor suppressor genes such as
P53 and
BRCA are mutated, which is perceived as DNA damage. Damaged DNA accumulates and finally leads to DDR. As a result, tumor cells may enter state of apoptosis or senescence through P53/cyclin E/CDK2/RB pathway [
6].
2.1. Oncogene–Induced Senescence
Senescence may also be induced by oncogenes; this is considered to be a tumor suppressor mechanism and the first barrier preventing intensified cell proliferation [
3]. During oncogene-induced senescence (OIS), cell cycle inhibition is usually mediated by the tumor suppressors—ADP ribosylation factors (ARF) and P16
INK4A, encoded by
CDKN2A locus [
2]. Certain oncogenes, such as
BRAF, may induce senescence through the activity of mitochondrial pyruvate kinase [
6]. Oncogene expression induces hyperproliferation. Consumption of DNA replication resources increases and finally the stalled replication forks occur, leading to DDR followed by senescence [
28,
29]. Inhibited expression of cancer suppressors triggers cell proliferation arrest, as exemplified by PICS (phosphatase and tensin homolog deleted on chromosome ten (PTEN) loss-induced cellular senescence), which has recently also been proven to be associated with hyperproliferation and the DDR mechanism [
30].
2.2. Oxidative Stress
Due to the replicative stress, the accumulation of ROS occurs. ROS induce cellular senescence by affecting various SASP components including regulation of P53/P21 and P16
INK4A/pRB pathways, enhancement of interleukin 1α (IL-1α) and matrix metalloproteinases (MMPs) synthesis, inhibition of sirtuins, decreasing activity of sarco/endoplasmic reticulum Ca
2+-ATPase or mammalian target of rapamycin (mTOR) pathway regulation [
31]. Furthermore, during OIS, ROS are able to imitate the signalling factors that are associated with promitogenic oncogene functions. Furthermore, the oncogene-induced ROS, arising from nicotinamide adenine dinucleotide phosphate (NADPH) oxidases, can lead to senescence by enhancing the initial hyperproliferative phase caused by the accumulation of DNA damage and altered DNA replication [
32].
2.3. Metabolic Stress
Metabolic stress is also a senescence inducer. Due to the stress factors—such as acidosis and hypoxia—UPR is triggered. UPR leads to senescence by arresting the cell cycle. Due to the high glucose demand and abnormal circulation, metabolic stress commonly occurs in cancers and the UPR [
33].