Disorders of sex development (DSDs), also known as differences in sex development, diverse sex development and variations in sex characteristics (VSC), are medical conditions involving the reproductive system. More specifically, these terms refer to "congenital conditions in which development of chromosomal, gonadal, or anatomical sex is atypical." The term has been controversial, and research has shown that affected people experience a negative impact, with the terminology impacting choice and utilization of health care providers. The World Health Organization and many medical journals still reference DSDs as intersex traits or conditions. The Council of Europe and Inter-American Commission on Human Rights have called for a review of medical classifications that unnecessarily medicalize intersex traits.
- sex development
- health
- sex characteristics
1. Overview
DSDs are medical conditions involving the way the reproductive system develops from infancy (and before birth) through young adulthood. There are several types of DSDs and their effect on the external and internal reproductive organs varies greatly.
A frequently-used social and medical adjective for people with DSDs is "intersex".[1] Parents with DSD children and clinicians involved in DSD treatment usually try to make clear distinctions between biological sex, social gender, and sexual orientation. This helps reduce confusion about the differences between being intersex, being transgender, and being gay/lesbian.
The most common DSD is congenital adrenal hyperplasia (CAH), which results in a person with female (XX) chromosomes having genitals that look somewhat masculine. In mild cases, CAH results in a slightly enlarged clitoris, while in more severe cases it can be difficult to decide on observation whether a baby is male or female (ambiguous genitalia). CAH is caused by a problem with the adrenal glands and is usually treated by taking a daily medication to replace or supplement the missing adrenal hormones. (When this adrenal problem occurs in people with male (XY) chromosomes, the result is over-masculinization and premature puberty).
Another common DSD is androgen insensitivity syndrome (AIS), also known as "testicular feminising syndrome" in which a person with male (XY) chromosomes does not respond to testosterone in the usual way. This results in a body that to some degree has a feminine appearance. In complete androgen insensitivity syndrome (CAIS) the result is a totally feminine appearance, including typical female breast development. Consequently, most young women with CAIS are unaware of their condition until the early teen years when they fail to menstruate. In the milder form, called partial androgen insensitivity syndrome (PAIS), the genitals can vary from mostly female to almost completely male. Some people with PAIS think of themselves as women or girls, others regard themselves as men or boys, and some consider themselves nonbinary.
One of the more uncommon DSDs is 5-alpha-reductase deficiency (5ARD). It is caused by a shortage early in life of an enzyme that converts testosterone into DHT. DHT is required for the development of external male genitalia. Therefore, in this condition, a person with male (XY) chromosomes has a body that appears female before puberty. After puberty begins, other testosterone-activating enzymes become available and the body soon takes on a masculine appearance, with the scrotum and penis usually reaching typical or nearly-typical size. If 5ARD is diagnosed at a young age, the child is often raised as a boy (a 1996 Brazilian study suggested that the majority of adults with this condition consider themselves men[2] but this has been questioned in some more recent research).
In addition to CAH, AIS and 5ARD there are several rarer types of DSDs, and in some cases, it is not possible to make a clear diagnosis of the underlying condition.
1.1. Genital Anatomy
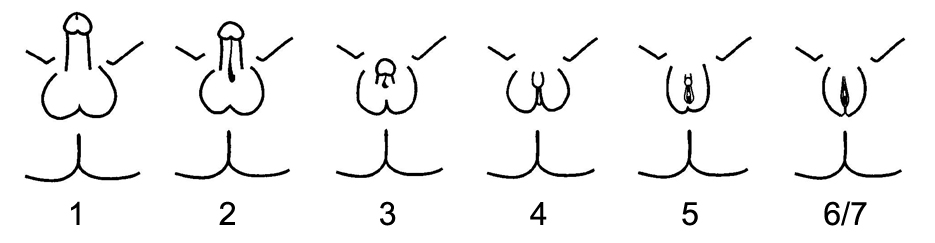
The penis (males) and clitoris (females) have a mutual origin, both arising from an embryonic structure called the primordial phallus. In typical males, the urethra is located at the tip of the penis, while in typical females the urethra is located below the base of the clitoris. It is also possible also to have a urethral opening located along the shaft; this condition is known as hypospadias.
Open-minded parenting, appropriate and conservative medical intervention, and age-appropriate child involvement in the treatment plan contribute greatly to successful outcomes for the entire range of DSDs.[3]
2. Conditions
- 47,XXY females - There are case reports of 47,XXY females; in some cases SRY or androgen receptor abnormalities are detected.[4]
- 47,XXY males – see Klinefelter syndrome below
- 48, XXXX (also known as tetrasomy X, quadruple X, and XXXX syndrome) – A condition that describes a female with two extra X chromosomes. It is considered a variation of Triple X syndrome. Women with 48, XXXX may or may not have issues associated with the condition though most are developmentally delayed and only about 50% undergo puberty normally.
- 48, XXYY (also known as XXYY syndrome) – A condition that describes a male with one extra X chromosome and one extra Y chromosome. It occurs in 1 in 18,000 to 40,000 male births.[5] 48, XXYY may result in infertility, low testosterone, and neurodevelopmental disorders like ADHD or autism but some men have no issues.
- 49, XXXXX (also known as pentasomy X and XXXXX syndrome) – A condition that describes a female with three extra X chromosomes. It is considered a variant of Triple X syndrome. Women with 49, XXXXX usually suffer from numerous health issues such as patent ductus arteriosus, scoliosis, kidney hypoplasia, and abnormal lobulation of the lungs. Physical deformities include microcephaly, micrognathia, and webbing of the neck.
- 49, XXXXY – A condition that describes a male with three extra X chromosomes. It is rare, occurring in 1 in 85,000 to 100,000 males.[6][7] It is considered a variation of Klinefelter syndrome. Men with 49, XXXXY syndrome often suffer from mental retardation.
- 5α-reductase deficiency (also known as 5-ARD) - An autosomal recessive condition caused by a mutation of the 5-alpha reductase type 2 gene. It only affects people with Y chromosomes, namely genetic males. People with this condition are fertile, with the ability to father children, but may be raised as females due to ambiguous or feminized genitalia.
- 17β-Hydroxysteroid dehydrogenase deficiency – A condition characterized by impaired androgen and estrogen synthesis in males and females, respectively. Results in pseudohermaphroditism/undervirilization in males and in excessive virilization of adult females.
- Androgen insensitivity syndrome (also known as AIS) – A condition which affects a genetic male's virilization. A person with androgen insensitivity syndrome produces androgens and testosterone but their body does not recognize it, either partially or completely. Mild androgen insensitivity syndrome generally causes no developmental issues and people with this form are raised as males. Partial androgen insensitivity syndrome results in ambiguous genitalia and there is no consensus regarding whether to raise a child with this form as male or female. Complete androgen insensitivity syndrome causes a genetic male to have a vagina (often incompletely developed, nearly always blind-ending), breasts, and a clitoris and people with this form are raised as females.
- Aphallia – A rare occurrence where a male is born without a penis or where a female is born without a clitoris. As of 2005, only 75 cases of aphallia have been documented.[8] It should not be confused with intentional or accidental amputation of the genitalia.
- Aposthia - A congenital defect where a male is born without a foreskin.
- Aromatase deficiency – A disorder in which, in females, is characterized by androgen excess and estrogen deficiency, and can result in inappropriate virilization, though without pseudohermaphroditism (i.e., genitals are phenotypically appropriate) (with the exception of the possible incidence of clitoromegaly). Aromatase deficiency can also be caused by mutations in P450 oxidoreductase gene.[9]
- Aromatase excess syndrome (also known as familial hyperestrogenism) - A condition that causes excessive estrogen production, resulting in feminization without pseudohermaphroditism (i.e., male genitalia at birth and female secondary sexual characteristics at puberty) in males and hyperfeminization in females.
- Campomelic dysplasia – a condition caused by de novo autosomal dominant mutations in the SOX9 gene, causing bowing of the limbs, sex reversal in around two thirds of 46,XY males (but not in 46,XX females), and respiratory insufficiency. While in roughly 95% of cases, death occurs in the neonatal period due to respiratory distress, those that live past infancy typically survive to become adults.
- Clitoromegaly – A clitoris that is considered larger than average. While clitoromegaly may be a symptom of an intersex condition, it may also be considered a normal variation in clitoris size. Clitoromegaly causes no health issues. Surgical reduction of the clitoris or its complete removal may be performed to normalize the appearance of the genitalia. While female genital mutilation is outlawed in many countries, reduction or the removal of the clitoris in cases of clitoromegaly are generally exempt, despite the fact that it is a nontherapeutic and sexually damaging surgery. Clitoromegaly may also be caused by females using testosterone or anabolic steroids for purposes related to female to male gender transition or bodybuilding.
- Combined 17α-hydroxylase/17,20-lyase deficiency – A condition in which presents as a combination of the symptoms of congenital adrenal hyperplasia and isolated 17,20-lyase deficiency. See those two conditions for more information.
- Complete androgen insensitivity syndrome (also known as CAIS) – A condition which completely affects a genetic male's ability to recognize androgens. It is considered a form of androgen insensitivity syndrome and is the most severe form. People with complete androgen insensitivity are raised as females and usually do not discover they are genetic males until they experience amenorrhoea in their late teens or they need medical intervention due to a hernia caused by their undescended testes. Complete androgen insensitivity syndrome results in a genetic male having a vagina, clitoris, and breasts which are capable of breastfeeding. However, they will not have ovaries or a uterus. Because they do not have ovaries or sufficiently developed testicles, people with complete androgen insensitivity syndrome are infertile.
- Congenital adrenal hyperplasia (also known as CAH) – A condition that causes excessive androgen production, which causes excessive virilization. It is most problematic in genetic females, where severe virilization can result in her having vaginal agenesis (absence of vagina) and a functional penis which is capable of penetrative intercourse. Females with this condition are usually fertile, with the ability to become pregnant and give birth. The salt-wasting variety of this condition is fatal in infants if left untreated.
- De la Chapelle syndrome (also known as XX male syndrome) – a condition where a genetically female 46,XX individual is phenotypically male, usually caused by atypical chromosomal crossover of the Y chromosome's SRY gene. XX males are shorter and weigh less than XY males, may have genital ambiguities, usually have small testes, and are universally sterile.[10]
- Denys–Drash syndrome and the related Frasier syndrome - similar rare conditions arising from de novo autosomal dominant mutations in the WT1 gene, causing symptoms ranging from undervirilization to complete sex reversal with persistant Müllerian ducts in affected 46,XY males (but not in 46,XX females). The disorders are invariably fatal before the age of 15, causing kidney failure due to nephrotic syndrome.
- Diphallia (also known as penile duplication, diphallic terata, and diphallasparatus) – A condition where a male is born with two penises. It's extremely rare, with only 100 cases being recorded since 1609 and an occurrence rate of 1 in 5,500,000 in the United States. The penises may be side by side or one on top of the other, being of equal size or with one penis being distinctively larger than the other, and both penises may be suitable for urination and intercourse. Men with diphallia may be sterile.
- Estrogen insensitivity syndrome (EIS) – The estrogen counterpart to androgen insensitivity syndrome. Extremely rare, with only one verified case having been reported; a biological male presented with tall stature, a heightened risk of osteoporosis, and sterility.
- Gonadal Dysgenesis – is any congenital developmental disorder of the reproductive system characterized by a progressive loss of primordial germ cells on the developing gonads of an embryo.
- Isolated 17,20-lyase deficiency – A condition that is characterized by either partial or complete inability to produce androgens and estrogens.[11] Results in partial or complete feminization and undervirilization in males and in a delayed, reduced, or absent puberty in both sexes, in turn causing sexual infantilism and infertility, among other symptoms.
- Klinefelter syndrome (also known as 47, XXY and XXY syndrome) – A condition that describes a male born with at least one extra X chromosome. Though the most common variation is 47, XXY, a man may also be 48, XXXY or 49, XXXXY. It is a common occurrence, affecting 1 in 500 to 1,000 men.[12] While some men may have no issues related to the syndrome, some may experience gynecomastia, micropenis, cognitive difficulties, hypogonadism, reduced fertility/infertility, and/or little or no facial hair. Testosterone therapy may be pursued by men who desire a more masculine appearance and those with gynecomastia may opt to undergo a reduction mammoplasty. Men who wish to father children may be able to do so with the help of IVF.[13]
- Leydig cell hypoplasia - A condition solely affecting biological males which is characterized by partial or complete inactivation of the luteinizing hormone receptor, resulting in stymied androgen production. Patients may present at birth with a fully female phenotype, ambiguous genitalia, or only mild genital defects such as micropenis and hypospadias. Upon puberty, sexual development is either impaired or fully absent.
- Micropenis (also known as microphallus) – A penis that measures 3 inches (7.62 centimeters) or less in length when erect. It is a common condition, occurring in 1 in 200 men.[14] Micropenis may be the result of undervirilization during fetal development or may be caused by an underlying intersex condition, such as mild androgen insensitivity syndrome, partial androgen insensitivity syndrome, or Klinefelter syndrome. It may also be considered a natural variation of penis size. While the majority of men have no issues with having a micropenis, some may opt to use a penile implant or undergo penile enlargement to increase the size of their penis.
- Lipoid congenital adrenal hyperplasia – An endocrine disorder that arises from defects in the earliest stages of steroid hormone synthesis: the transport of cholesterol into the mitochondria and the conversion of cholesterol to pregnenolone—the first step in the synthesis of all steroid hormones.
- Mild androgen insensitivity syndrome (also known as MAIS) – A condition which mildly affects a genetic male's ability to recognize androgens. It is considered a form of androgen insensitivity syndrome and is considered the least severe form. While men generally do not need any specialized medical care related to this form, mild androgen insensitivity syndrome may result in gynecomastia and hypospadias. Neither gynecomastia nor hypospadias require surgical intervention or adversely affect a man's health though some men may opt to undergo surgery to remove their breasts and/or repair their hypospadias. Men with mild androgen insensitivity syndrome may have reduced fertility.
- Mixed gonadal dysgenesis – is a condition of unusual and asymmetrical gonadal development leading to an unassigned sex differentiation. A number of differences have been reported in the karyotype, most commonly a mosaicism 45,X/ 46, XY.
- Ovotesticular disorder (also called true hermaphroditism) – A condition where an individual has both testicular and ovary tissue.
- Partial androgen insensitivity syndrome (also known as PAIS) – A condition which partially affects a genetic male's ability to recognize androgens. It is considered a form of androgen insensitivity syndrome and while it is not as severe as complete androgen insensitivity syndrome, it is more severe than mild androgen insensitivity syndrome. Partial androgen insensitivity syndrome causes major problems with gender assignment because it causes ambiguous genitalia such as a micropenis or clitoromegaly in addition to breast development. People with partial androgen insensitivity syndrome who are assigned as males may undergo testosterone therapy to virilize their body while those who are assigned as females may undergo a surgical reduction of the clitoris and/ or estrogen therapy.
- Penoscrotal transposition
- Persistent Müllerian duct syndrome A condition where Fallopian tubes, uterus, or the upper part of the vagina are present in an otherwise normal male.
- Pseudovaginal perineoscrotal hypospadias (also known as PPSH) – A form of ambiguous genitalia which results in a phallic structure that is smaller than a penis but larger than a clitoris, a chordee, hypospadias, and a shallow vagina.
- Swyer Syndrome (Also known as Pure Gonadal Dysgenesis or XY gonadal dysgenesis) is a type of hypogonadism in a person whose karyotype is 46,XY. The person is externally female with streak gonads, and left untreated, will not experience puberty. Such gonads are typically surgically removed (as they have a significant risk of developing tumors) and a typical medical treatment would include hormone replacement therapy with female hormones.
- Triple X syndrome – A condition that describes a female born with an extra X chromosome, making her karotype 47, XXX. It is a common occurrence, affecting 1 in 1,000 females.[15] It generally causes no health issues or abnormal development.
- Turner syndrome (also known as Ullrich-Turner syndrome and gonadal dysgenesis) – A condition that describes a female born with only one X chromosome or with an abnormal X chromosome, making her karotype 45, XO. It occurs in 1 in 2,000 to 5,000 females. Turner syndrome causes numerous health and development problems, including but not limited to short stature, lymphedema, infertility, webbed neck, coarctation of the aorta, ADHD, amenorrhoea, and obesity.
- Uterus didelphys (also known as double uterus) – A condition where a female is born with two uteri. It is often accompanied by two vaginas. It is generally not considered a health issue and women with uterus didelphys usually have normal sex lives and pregnancies.[16]
- Müllerian agenesis (also known as MRKH or Vaginal Agenesis) – A condition that causes the uterus and other reproductive organs in a 46,XX female to be small or absent, as well as the vaginal canal itself. It affects 1 out of 4,500 to 5,000 females and can also come with skeletal or endocrine system issues at conception.
3. Controversy
The term DSD (and particularly its association with medical disorders) has been controversial. The argument over terminology reflects a deeper disagreement over the extent to which intersex conditions require medical intervention, the appropriateness of certain interventions, and whether physicians and parents should make irreversible treatment decisions on behalf of young children if the condition is not life-threatening.
- Use of the term disorder of sex development (DSD) is controversial among many activists and community organizations due to the label "disorders".[17][18][19][20] Many governments and international institutions use the term 'intersex' in preference to 'DSD', or have called for the review of medical classifications.[21][22] In May 2019, more than 50 intersex-led organizations signed a multilingual joint statement condemning the introduction of "disorders of sex development" language into the International Classification of Diseases, stating that this causes "harm" and facilitates human rights violations, calling on the World Health Organization to publish clear policy to ensure that intersex medical interventions are "fully compatible with human rights norms".[23][24][25][26][27]
- Lee et al. in a 2006 Consensus statement on management of intersex disorders proposed a system of nomenclature based on "disorders of sex development" for clinical use, suggesting that "terms such as intersex, pseudohermaphroditism, hermaphroditism, sex reversal, and gender based diagnostic labels are particularly controversial," may be perceived as pejorative, and are confusing to practitioners and parents alike.[28] However, research by the Lurie Children's Hospital, Chicago, and the AIS-DSD Support Group published in 2017 found that affected persons, and care givers, object to the term, and that this may impact choice, access, and utilization of health care providers.[29] Australian sociological research on people born with atypical sex characteristics, published in 2016, found that 3% of respondents choose the term "disorders of sex development" or "DSD" to define their sex characteristics, while 21% use the term when accessing medical services. In contrast, 60% used the term "intersex" in some form to self-describe their sex characteristics.[30]
- A committee of the Senate of Australia found that labelling intersex as "pejorative" appeared to be a post-hoc rationalisation in the 2006 Consensus statement. It recommended a review of clinical use of the term.[31]
- Alternative terms have been offered: Milton Diamond has suggested the use of "variation"[32][33] or of "difference",[34] Elizabeth Reis has suggested "divergence";[35] Liao and Simmonds suggest "diverse sex development".[36] The latter suggestions would retain the initial D in DSD.
- The 2006 Consensus statement on management of intersex disorders stated that evidence for early surgery for cosmetic reasons is lacking, outcomes include "decreased sexual sensitivity" and long term outcome data is absent.[28] A 2016 Global Disorders of Sex Development Update since 2006 states that there is "still no consensual attitude regarding indications, timing, procedure and evaluation of outcome of DSD surgery" and "no evidence regarding the impact of surgically treated or non-treated DSDs during childhood for the individual, the parents, society or the risk of stigmatization".[37]
- In 2013, Juan E. Méndez, the United Nations Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment, condemned "irreversible sex assignment, involuntary sterilization, involuntary genital normalizing surgery, performed without their informed consent, or that of their parents, “in an attempt to fix their sex”" stating that "members of sexual minorities are disproportionately subjected to torture and other forms of ill-treatment because they fail to conform to socially constructed gender expectations".[38]
- In May 2014, the World Health Organization issued a joint statement on Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement with the OHCHR, UN Women, UNAIDS, UNDP, UNFPA and UNICEF. Referencing the involuntary surgical "sex-normalising or other procedures" on "intersex persons", the report recommends a range of guiding principles for medical treatment, including ensuring patient autonomy in decision-making, ensuring non-discrimination, accountability and access to remedies.[39]
- During 2015, the Council of Europe,[21] and Inter-American Commission on Human Rights[22] called for a review of medical classifications that unnecessarily medicalize intersex traits[21][22][40] an end to medical interventions without consent, and improved disclosure. The Council of Europe's Human Rights Commissioner recommended: National and international medical classifications which pathologise variations in sex characteristics should be reviewed with a view to eliminating obstacles to the effective enjoyment, by intersex persons, of human rights, including the right to the highest attainable standard of health.
- The European Union Agency for Fundamental Rights[40] and UN Treaty Bodies have called for informed consent by individuals subjected to medical treatment, improved disclosure, and access to redress.[41][42]
The content is sourced from: https://handwiki.org/wiki/Medicine:Disorders_of_sex_development
References
- UN Committee against Torture; UN Committee on the Rights of the Child; UN Committee on the Rights of People with Disabilities; UN Subcommittee on Prevention of Torture and other Cruel, Inhuman or Degrading Treatment or Punishment; Juan Méndez, Special Rapporteur on torture and other cruel inhuman or degrading treatment or punishment; Dainius Pῡras Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health; Dubravka Šimonoviæ, Special Rapporteur on violence against women its causes and consequences; Marta Santos Pais, Special Representative of the UN Secretary-General on Violence against Children et al. (October 24, 2016), "Intersex Awareness Day – Wednesday 26 October. End violence and harmful medical practices on intersex children and adults, UN and regional experts urge", Office of the High Commissioner for Human Rights, http://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=20739&LangID=E
- "Male pseudohermaphroditism due to steroid 5-alpha-reductase deficiency". The American Journal of Medicine 62 (2): 170–91. February 1977. doi:10.1016/0002-9343(77)90313-8. PMID 835597. https://dx.doi.org/10.1016%2F0002-9343%2877%2990313-8
- Pediatric gender assignment: a critical reappraisal; [proceedings from a conference ... in Dallas in the spring of 1999. New York, NY: Kluwer Academic/Plenum Publishers. 2002. ISBN 978-0-306-46759-2.
- Röttger, S., K. Schiebel, G. Singer, S. Ebner, W. Schempp, and G. Scherer. Röttger, S., K. Schiebel, G. Singer, S. Ebner, W. Schempp, and G. Scherer. "An SRY-negative 47,XXY mother and daughter." Cytogenetics and Cell Genetics 91.1–4 (2000): 204–07. National Center for Biotechnology Information. U.S. National Library of Medicine, 2001. Web. 12 Aug. 2013. https://www.ncbi.nlm.nih.gov/pubmed/11173857
- "A new look at XXYY syndrome: medical and psychological features". American Journal of Medical Genetics. Part A 146A (12): 1509–22. June 2008. doi:10.1002/ajmg.a.32366. PMID 18481271. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3056496
- What is XXXXY syndrome? Retrieved March 26, 2008. http://www.xxxxysyndrome.com/what_is___.htm
- "Klinefelter syndrome and other sex chromosomal aneuploidies". Orphanet Journal of Rare Diseases 1: 42. October 2006. doi:10.1186/1750-1172-1-42. PMID 17062147. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1634840
- "Male gender assignment in aphallia: a case report and review of the literature". International Urology and Nephrology 37 (2): 317–9. 2005. doi:10.1007/s11255-004-7974-0. PMID 16142564. https://dx.doi.org/10.1007%2Fs11255-004-7974-0
- "Molecular Basis of CYP19A1 Deficiency in a 46,XX Patient With R550W Mutation in POR: Expanding the PORD Phenotype". The Journal of Clinical Endocrinology and Metabolism 105 (4). April 2020. doi:10.1210/clinem/dgaa076. PMID 32060549. https://dx.doi.org/10.1210%2Fclinem%2Fdgaa076
- Vorona, Elena; Zitzmann, Michael; Gromoll, Jörg; Schüring, Andreas N.; Nieschlag, Eberhard (2007-09-01). "Clinical, Endocrinological, and Epigenetic Features of the 46,XX Male Syndrome, Compared with 47,XXY Klinefelter Patients". The Journal of Clinical Endocrinology & Metabolism 92 (9): 3458–3465. doi:10.1210/jc.2007-0447. ISSN 0021-972X. PMID 17579198. https://dx.doi.org/10.1210%2Fjc.2007-0447
- "The syndrome of 17,20 lyase deficiency". The Journal of Clinical Endocrinology and Metabolism 97 (1): 59–67. January 2012. doi:10.1210/jc.2011-2161. PMID 22072737. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3251937
- The Focus Foundation. X & Y Variations. thefocusfoundation.org http://www.thefocusfoundation.org/FF/XYvariations.php
- "Should non-mosaic Klinefelter syndrome men be labelled as infertile in 2009?". Human Reproduction 25 (3): 588–97. March 2010. doi:10.1093/humrep/dep431. PMID 20085911. https://dx.doi.org/10.1093%2Fhumrep%2Fdep431
- Op can boost size of micro-penis, BBC News, Published December 6, 2004 http://news.bbc.co.uk/2/hi/health/4071657.stm
- National Library of Medicine (2007). "Genetics Home Reference: Triple X syndrome". http://ghr.nlm.nih.gov/condition=triplexsyndrome.
- Double uterus Mayo Clinic, Published September 11, 2010 http://www.mayoclinic.com/health/double-uterus/DS00821
- "An Interview with Dr. Tiger Howard Devore PhD". We Who Feel Differently. February 7, 2011. http://wewhofeeldifferently.info/interview.php?interview=108.
- interACT (May 2016). "interACT Statement on Intersex Terminology". Interact Advocates for Intersex Youth. http://interactadvocates.org/interact-statement-on-intersex-terminology/.
- Briffa, Tony (8 May 2014). "Disorders of Sex Development". Organisation Intersex International Australia. http://oii.org.au/26808/tony-briffa-on-dsd/.
- "Why Not "Disorders of Sex Development"?". UK Intersex Association. http://www.ukia.co.uk/ukia/dsd.html.
- Council of Europe; Commissioner for Human Rights (April 2015), Human rights and intersex people, Issue Paper, https://wcd.coe.int/ViewDoc.jsp?Ref=CommDH/IssuePaper(2015)1&Language=lanEnglish&Ver=original
- Comisión Interamericana de Derechos Humanos (November 12, 2015) (in Spanish), Violencia contra Personas Lesbianas, Gays, Bisexuales, Trans e Intersex en América, http://www.oas.org/es/cidh/informes/pdfs/ViolenciaPersonasLGBTI.pdf
- Intersex Human Rights Australia (2019-05-23). "Joint statement on the International Classification of Diseases 11". https://ihra.org.au/35299/joint-statement-icd-11/.
- Crittenton, Anya (2019-05-24). "World Health Organization condemned for classifying intersex as 'disorder'". Gay Star News. https://www.gaystarnews.com/article/world-health-organization-condemned-classifying-intersex-disorder/.
- Leighton-Dore, Samuel (2019-05-28). "World Health Organisation drops transgender from list of mental health disorders". SBS. https://www.sbs.com.au/topics/sexuality/agenda/article/2019/05/28/world-health-organisation-drops-transgender-list-mental-health-0.
- Barr, Sabrina (2019-05-28). "Transgender no longer classified as 'mental disorder' by WHO". The Independent. https://www.independent.co.uk/life-style/transgender-world-health-organisation-mental-disorder-who-gender-icd11-update-a8932786.html.
- Wills, Ella (2019-05-29). "Campaigners hail changes to WHO classification of trans health issues". Evening Standard. https://www.standard.co.uk/news/world/human-rights-campaigners-hail-major-change-by-who-as-transgender-no-longer-recognised-as-mental-a4154421.html.
- "Consensus statement on management of intersex disorders. International Consensus Conference on Intersex". Pediatrics 118 (2): e488-500. August 2006. doi:10.1542/peds.2006-0738. PMID 16882788. PMC 2082839. http://pediatrics.aappublications.org/cgi/reprint/118/2/e488.
- "Attitudes towards "disorders of sex development" nomenclature among affected individuals". Journal of Pediatric Urology 13 (6): 608.e1–608.e8. December 2017. doi:10.1016/j.jpurol.2017.03.035. PMID 28545802. https://dx.doi.org/10.1016%2Fj.jpurol.2017.03.035
- Jones, Tiffany; Hart, Bonnie; Carpenter, Morgan; Ansara, Gavi; Leonard, William; Lucke, Jayne (2016). Intersex: Stories and Statistics from Australia. Cambridge, UK: Open Book Publishers. ISBN 978-1-78374-208-0. http://oii.org.au/wp-content/uploads/key/Intersex-Stories-Statistics-Australia.pdf. Retrieved 2 February 2016.
- "Involuntary or coerced sterilisation of intersex people in Australia". Senate Community Affairs Committee. October 2013. http://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/Involuntary_Sterilisation/Sec_Report/index.
- Beh, Hazel; Diamond, Milton (2006). "Variations of Sex Development Instead of Disorders of Sex Development". Archives of Disease in Childhood (26 July 2006). http://www.hawaii.edu/PCSS/biblio/articles/2005to2009/2006-variations.html.
- "Managing variation in sex development". Journal of Pediatric Endocrinology & Metabolism 20 (4): 552–3. April 2007. PMID 17550222. http://www.hawaii.edu/PCSS/biblio/articles/2005to2009/2007-managing-variation.html.
- "Changes in the management of children with intersex conditions". Nature Clinical Practice. Endocrinology & Metabolism 4 (1): 4–5. January 2008. doi:10.1038/ncpendmet0694. PMID 17984980. http://www.hawaii.edu/PCSS/biblio/articles/2005to2009/2008-changes-in-management.html.
- "Divergence or disorder?: the politics of naming intersex". Perspectives in Biology and Medicine 50 (4): 535–43. 2007. doi:10.1353/pbm.2007.0054. PMID 17951887. https://www.researchgate.net/publication/5893631.
- Liao, Lih-Mei; Simmonds, Margaret (2013). "A values-driven and evidence-based health care psychology for diverse sex development". Psychology & Sexuality 5 (1): 83–101. doi:10.1080/19419899.2013.831217. ISSN 1941-9899. http://discovery.ucl.ac.uk/1461157/1/19419899%252E2013%252E831217.pdf.
- "Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care". Hormone Research in Paediatrics 85 (3): 158–80. January 28, 2016. doi:10.1159/000442975. PMID 26820577. https://dx.doi.org/10.1159%2F000442975
- Méndez, Juan (February 2013). "Report of the Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment, A.HRC.22.53". http://www.ohchr.org/Documents/HRBodies/HRCouncil/Regularsession/Session22/A.HRC.22.53_English.pdf.
- "Eliminating forced, coercive and otherwise involuntary sterilization, An interagency statement". World Health Organization. May 2014. http://www.who.int/reproductivehealth/publications/gender_rights/eliminating-forced-sterilization/en/.
- European Union Agency for Fundamental Rights (April 2015), The fundamental rights situation of intersex people, http://fra.europa.eu/sites/default/files/fra-2015-focus-04-intersex.pdf
- United Nations; Committee on the Rights of Persons with Diabilities (April 17, 2015), Concluding observations on the initial report of Germany (advance unedited version), Geneva: United Nations, http://tbinternet.ohchr.org/_layouts/treatybodyexternal/Download.aspx?symbolno=CRPD%2FC%2FDEU%2FCO%2F1&Lang=en
- United Nations; Committee on the Rights of Child (February 26, 2015), Concluding observations on the combined second to fourth periodic reports of Switzerland, Geneva: United Nations, http://tbinternet.ohchr.org/_layouts/treatybodyexternal/Download.aspx?symbolno=CRC%2fC%2fCHE%2fCO%2f2-4&Lang=en
