Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
The adolescent brain is an open window on the environment, which is vulnerable to perturbations and the traumatic experiences occurring before or during this period have an increased saliency in affecting cognitive, emotional, and social levels. During adolescence, trauma-related effects causing significant impairment or suffering could be manifest in internalizing and externalizing behaviors.
- trauma
- post-traumatic stress disorder
- development
- extroverted symptoms
- introverted symptoms
- amygdala
- medial prefrontal cortex
- multiple and multimodal therapeutic treatments
1. Introduction
Trauma occurs more often than people think in youths. By age 16, two-thirds of children reported at least one traumatic event [1]. Among traumatic events, it is possible to include psychological, physical, or sexual abuse; community or school violence; witnessing or experiencing domestic violence; national disasters or terrorism; commercial sexual exploitation; sudden or violent loss of a loved one; refugee or war experiences; family-related military stressors; physical or sexual assault; neglect; serious accidents or life-threatening illness.
The developmental period is especially crucial when examining the effects of trauma at both neurobiological and behavioral levels. Coping with a history of chronic trauma or experiencing exposure to acute trauma during the development may have different, and sometimes even more significant, bio-psycho-social effects than trauma exposure occurring in adulthood [2]. In particular, changes occurring during adolescence are strictly associated with a prolonged period of brain and behavioral adaptations to prepare the individual for independence. Very briefly, adolescent humans, nonhuman primates, and rodents develop similar behaviors, including separation from parents, enhanced social interactions, increased risk-taking and sensation-seeking behaviors, modified food intake, and postponed sleep cycles [3]. In addition, the transition to adolescence gathers attention because some neuropsychiatric disorders, including schizophrenia, manifest at this period of life [4][5][6], and the transition is especially risky for children who are growing up in traumatic environments [7][8], partially due to the heightened trauma reactivity that characterizes the onset of puberty [9][10][11]. In fact, the variety of drastic (progressive as well as regressive) alterations in the brain renders the adolescent system highly vulnerable to the effects of trauma exposure. A history of trauma can be preadolescence-limited (i.e., early childhood and childhood) or adolescence-limited (i.e., early adolescence, adolescence, and late adolescence), with trauma-related behavioral and brain effects measured in adolescence or in adulthood (the specific ages for each developmental period are shown in Figure 1).
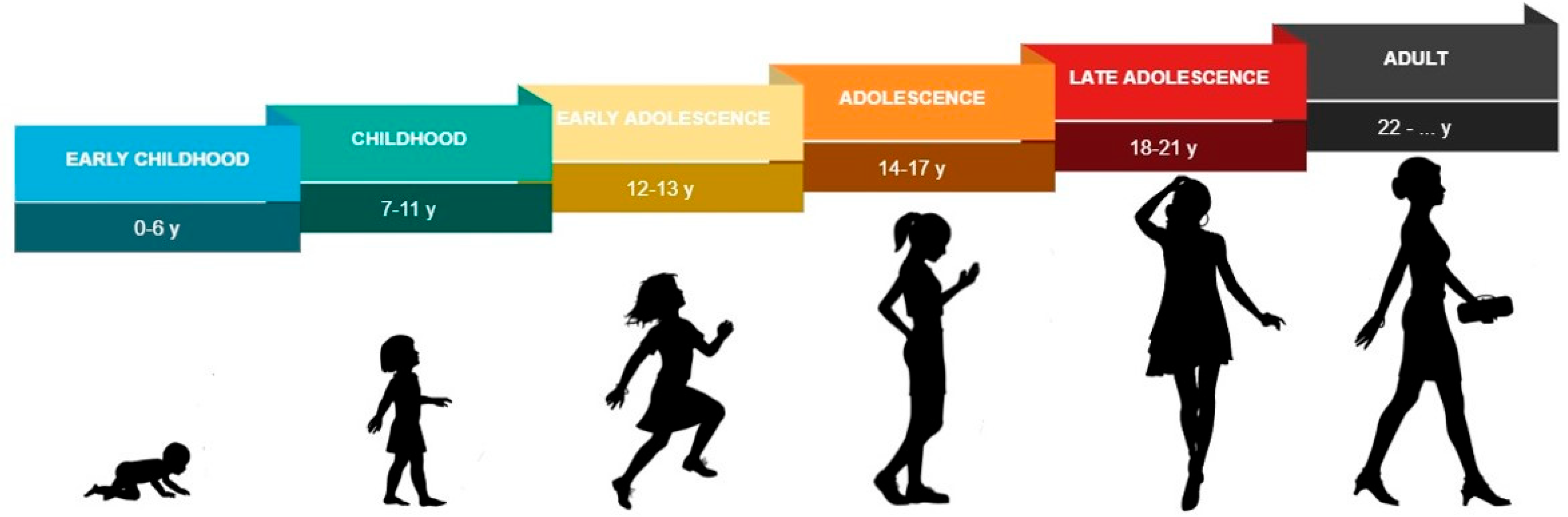
Figure 1. Specific ages for each developmental period (i.e., early childhood, childhood, early adolescence, adolescence, late adolescence, and adulthood) are reported.
During adolescence, affective, cognitive, and behavioral symptoms related to trauma causing significant impairment or suffering could be classified within the internalizing and externalizing domains [12][13][14]. Internalizing problems are those having mood or emotion as their primary feature and include symptoms such as anxiety, depression, anhedonia, and withdrawal, while externalizing problems are those such as aggression, delinquency, oppositional defiant disorder, and conduct disorder [15][16]. Thus, it is important to recognize the signs of trauma and its short- and long-term consequences and, faced with the complexity of trauma-related consequences, psychoanalysts who work with adolescents are urged to co-construct a relationship with traumatized adolescents to favor the plastic potential of the brain and the Self, enlarging the therapeutic level to counteract the internalizing or externalizing behaviors.
2. Diagnostic Aspects and Neurobiological Correlates in Traumatized Adolescents: A Scenario on Externalizing/Internalizing Behaviors
One of the adaptive values of long adolescence is a prolonged period of synaptogenesis, neuroplasticity, and neuronal connectivity, all processes that sustain behavioral changes, mainly in the social domain, needed for the passage to adulthood [17][18]. The adolescent brain is vulnerable to environmental perturbations and traumatic experiences occurring before or during this period have an increased saliency in affecting cognitive, emotional, and social levels. Given these bio-psycho-social changes occurring in this part of life, diagnosing trauma-related disorders in adolescence is quite complex. In this life period, besides a categorical approach, a dimensional approach should be used in the diagnostic process as a tool to capture the elements of continuity in physiological and psychopathological trajectories of development [19]. According to the fifth edition of the Diagnostic and Statistical Manual (DSM-5) of mental disorders, trauma-related disorders during adolescence imply exposure to overwhelming, aversive, threatening, or fearful experiences [20]. Affective, cognitive, and behavioral symptoms related to trauma causing significant impairment or suffering can be accompanied by dissociative symptomatology (depersonalization and derealization on the positive pole, as well as dissociative amnesia on the negative pole). As mentioned above, trauma-related symptoms in adolescence can be classified within the externalizing and internalizing domains, along with a dimension ranging from hyper- to hypoarousal, and may also lead to a Reactive Attachment Disorder or an Uninhibited Social Engagement Disorder [12][13][14]. As regards externalizing behaviors, extroverted symptoms mainly occur such as: hypervigilance, impulsivity, hyperactivity, disinhibition, aggression, mood enhancement, intrusive thoughts, disorganized cognitive processing on the paranoid side, substance abuse, difficulty in attention and concentration, hyperactivity, and hyperexcitability, accompanied by depersonalization and derealization. Conversely, introverted symptoms mainly occur in the presence of internalizing behaviors, such as: freezing, social withdrawal, mood deflection, cognitive inhibition, depressive ideation, numbing, reduced psychomotor skills, avoidance behaviors, and feelings of impotence, accompanied by dissociative amnesia.
The externalizing/internalizing conducts are grounded in a neurobiological basis, which undergo crucial changes during adolescence, especially in the presence of trauma. In fact, brain structure, function and connectivity, neurotransmitter levels, stress response, homeostasis maintenance, immune system, genetics/epigenetics, and gut microbiome undergo marked changes due to trauma exposure [21][22][23]. To improve understanding of how the effects of traumatic experiences on the brain involve changes at nearly every level of analysis, there is a need to comprehend the adolescent physiological conditions. During adolescence, brain remodeling is characterized by changes in associative and limbic circuits (such as the medial prefrontal cortex, amygdala, and hippocampus) subserving high-order processes (e.g., executive function, mentalizing, emotion regulation, and social cognition), along with dramatic changes in endocrine, immune, and biochemical systems [18][24]. The initiation of puberty represents a period of dynamic synaptogenesis and dendritic/synaptic pruning, with experience-dependent remodeling of brain circuits underlying complex behaviors [25][26]. Specifically, during this time there is substantial pruning of excitatory synapses in the cortex and in particular in the prefrontal cortex, supporting the hypothesis that overproduction and subsequent pruning of synapses is a computationally advantageous approach to building a competent brain [27]. A correct balance of activity of the GABA and glutamate systems is vital for optimal neurodevelopment and general central nervous system function, and the dysregulation of this balance has been implicated in a number of neurological conditions that range from mild to severe, including schizophrenia and epilepsy, and has been shown to increase the incidence of anxiety disorders [28][29].
In the context of trauma, the amygdala, the medial prefrontal cortex, and the hippocampus have been extensively investigated with respect to fear learning and extinction, threat reactivity, and emotion regulation [30][31][32], and they have been identified as critical loci of dysfunction following trauma [33][34]. Notably, acute exposure to threatening adversity promotes the secretion of hormones (e.g., cortisol) and pro-inflammatory cytokines, which drive changes in the structural plasticity of the amygdala and hippocampus to enhance fear learning in the occurrence of similar events [35]. Chronic exposure to traumatic events acts through these same hormonal and immune mediators to create glutamatergic excitotoxicity and atrophy in the amygdala and hippocampus linked to impaired memory and other behavioral and cognitive symptoms, commonly found in internalizing behaviors, such as depression [36]. Furthermore, deficits in the synthesis of GABAergic neurosteroids—produced from progesterone in the brain, adrenal gland, ovaries, and testes [37], clearly more active during puberty—have been implicated in the pathophysiology and recovery from trauma-related disorders [38]. For individuals raised in environments where multiple sources of threat are present and/or long-term survival is uncertain, the “developmental reprioritization” is often marked by an accelerated maturation, characterized by the early emergence of adult-like phenotypes [39][40]. Specifically, traumatized children showed adult-like neural phenotype in the functional connectivity between the amygdala and medial prefrontal cortex during threat processing [41][42][43][44], in parallel with experimental reports indicating that early adversity leads to accelerated myelination of axons in the amygdala [45].
Overall, across various types of traumatic experiences, an altered structure, function, and connectivity of the amygdala, medial prefrontal cortex, and hippocampus correspond to an increased fear reactivity, attentional biases towards threat, and difficulty with affective regulation [46][47][48], contributing to a risk of externalizing/internalizing behaviors.
This entry is adapted from the peer-reviewed paper 10.3390/adolescents2040032
References
- Copeland, W.E.; Keeler, G.; Angold, A.; Costello, E.J. Traumatic Events and Posttraumatic Stress in Childhood. Arch. Gen. Psychiatry 2007, 64, 577–584.
- Birn, R.M.; Patriat, R.; Phillips, M.L.; Germain, A.; Herringa, R.J. Childhood Maltreatment and Combat Posttraumatic Stress Differentially Predict Fear-Related Fronto-Subcortical Connectivity. Depress. Anxiety 2014, 31, 880–892.
- Spear, L.P. The Adolescent Brain and Age-Related Behavioral Manifestations. Neurosci. Biobehav. Rev. 2000, 24, 417–463.
- Kessler, R.C.; Adler, L.A.; Barkley, R.; Biederman, J.; Conners, C.K.; Faraone, S.V.; Greenhill, L.L.; Jaeger, S.; Secnik, K.; Spencer, T.; et al. Patterns and Predictors of ADHD Persistence into Adulthood: Results from the National Comorbidity Survey Replication. Biol. Psychiatry 2005, 57, 1442–1451.
- Paus, T.; Keshavan, M.; Giedd, J.N. Why Do Many Psychiatric Disorders Emerge during Adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957.
- Merikangas, K.R.; He, J.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989.
- LeMoult, J.; Humphreys, K.L.; Tracy, A.; Hoffmeister, J.-A.; Ip, E.; Gotlib, I.H. Meta-Analysis: Exposure to Early Life Stress and Risk for Depression in Childhood and Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 842–855.
- Rudolph, K.D.; Flynn, M. Childhood Adversity and Youth Depression: Influence of Gender and Pubertal Status. Dev. Psychopathol. 2007, 19, 497–521.
- Dahl, R.E.; Gunnar, M.R. Heightened Stress Responsiveness and Emotional Reactivity during Pubertal Maturation: Implications for Psychopathology. Dev. Psychopathol. 2009, 21, 1–6.
- Doom, J.R.; Gunnar, M.R. Stress Physiology and Developmental Psychopathology: Past, Present, and Future. Dev. Psychopathol. 2013, 25, 1359–1373.
- Busso, D.S.; McLaughlin, K.A.; Sheridan, M.A. Dimensions of Adversity, Physiological Reactivity, and Externalizing Psychopathology in Adolescence: Deprivation and Threat. Psychosom. Med. 2017, 79, 162–171.
- Hofstra, M.B.; Van der Ende, J.; Verhulst, F.C. Pathways of Self-Reported Problem Behaviors from Adolescence into Adulthood. Am. J. Psychiatry 2002, 159, 401–407.
- King, S.M.; Iacono, W.G.; McGue, M. Childhood Externalizing and Internalizing Psychopathology in the Prediction of Early Substance Use. Addict. Abingdon Engl. 2004, 99, 1548–1559.
- Reef, J.; Diamantopoulou, S.; van Meurs, I.; Verhulst, F.; van der Ende, J. Predicting Adult Emotional and Behavioral Problems from Externalizing Problem Trajectories in a 24-Year Longitudinal Study. Eur. Child Adolesc. Psychiatry 2010, 19, 577–585.
- Achenbach, T.M.; Howell, C.T.; Quay, H.C.; Conners, C.K. National Survey of Problems and Competencies among Four- to Sixteen-Year-Olds: Parents’ Reports for Normative and Clinical Samples. Monogr. Soc. Res. Child Dev. 1991, 56, 1–131.
- Kovacs, M.; Devlin, B. Internalizing Disorders in Childhood. J. Child Psychol. Psychiatry 1998, 39, 47–63.
- Houston, S.M.; Herting, M.M.; Sowell, E.R. The Neurobiology of Childhood Structural Brain Development: Conception through Adulthood. Curr. Top. Behav. Neurosci. 2014, 16, 3–17.
- Ho, T.C.; King, L.S. Mechanisms of Neuroplasticity Linking Early Adversity to Depression: Developmental Considerations. Transl. Psychiatry 2021, 11, 517.
- Lingiardi, V.; Gazzillo, F. La Personalità e i Suoi Disturbi; Raffaello Cortina Editore: Milan, Italy, 2014.
- APA. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013; p. xliv, 947; ISBN 978-0-89042-554-1.
- De Bellis, M.D.; Zisk, A. The Biological Effects of Childhood Trauma. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 185–222.
- Agorastos, A.; Pervanidou, P.; Chrousos, G.P.; Baker, D.G. Developmental Trajectories of Early Life Stress and Trauma: A Narrative Review on Neurobiological Aspects Beyond Stress System Dysregulation. Front. Psychiatry 2019, 10, 118.
- Kolacz, J.; Kovacic, K.K.; Porges, S.W. Traumatic Stress and the Autonomic Brain-Gut Connection in Development: Polyvagal Theory as an Integrative Framework for Psychosocial and Gastrointestinal Pathology. Dev. Psychobiol. 2019, 61, 796–809.
- Dandash, O.; Cherbuin, N.; Schwartz, O.; Allen, N.B.; Whittle, S. The Long-Term Associations between Parental Behaviors, Cognitive Function and Brain Activation in Adolescence. Sci. Rep. 2021, 11, 11120.
- Blakemore, S.-J. Development of the Social Brain during Adolescence. Q. J. Exp. Psychol. 2006 2008, 61, 40–49.
- Pfeifer, J.H.; Allen, N.B. Puberty Initiates Cascading Relationships between Neurodevelopmental, Social, and Internalizing Processes across Adolescence. Biol. Psychiatry 2021, 89, 99–108.
- Averbeck, B.B. Pruning Recurrent Neural Networks Replicates Adolescent Changes in Working Memory and Reinforcement Learning. Proc. Natl. Acad. Sci. USA 2022, 119, e2121331119.
- Meldrum, B.S. Glutamate as a Neurotransmitter in the Brain: Review of Physiology and Pathology. J. Nutr. 2000, 130, 1007S–1015S.
- Deidda, G.; Bozarth, I.F.; Cancedda, L. Modulation of GABAergic Transmission in Development and Neurodevelopmental Disorders: Investigating Physiology and Pathology to Gain Therapeutic Perspectives. Front. Cell. Neurosci. 2014, 8, 119.
- Laricchiuta, D.; Saba, L.; De Bartolo, P.; Caioli, S.; Zona, C.; Petrosini, L. Maintenance of Aversive Memories Shown by Fear Extinction-Impaired Phenotypes Is Associated with Increased Activity in the Amygdaloid-Prefrontal Circuit. Sci. Rep. 2016, 6, 21205.
- Laricchiuta, D.; Sciamanna, G.; Gimenez, J.; Termine, A.; Fabrizio, C.; Caioli, S.; Balsamo, F.; Panuccio, A.; De Bardi, M.; Saba, L.; et al. Optogenetic Stimulation of Prelimbic Pyramidal Neurons Maintains Fear Memories and Modulates Amygdala Pyramidal Neuron Transcriptome. Int. J. Mol. Sci. 2021, 22, 810.
- Borgomaneri, S.; Battaglia, S.; Sciamanna, G.; Tortora, F.; Laricchiuta, D. Memories Are Not Written in Stone: Re-Writing Fear Memories by Means of Non-Invasive Brain Stimulation and Optogenetic Manipulations. Neurosci. Biobehav. Rev. 2021, 127, 334–352.
- Tottenham, N.; Sheridan, M.A. A Review of Adversity, the Amygdala and the Hippocampus: A Consideration of Developmental Timing. Front. Hum. Neurosci. 2009, 3, 68.
- Tottenham, N. Human Amygdala Development in the Absence of Species-Expected Caregiving. Dev. Psychobiol. 2012, 54, 598–611.
- McEwen, B.S.; Stellar, E. Stress and the Individual. Mechanisms Leading to Disease. Arch. Intern. Med. 1993, 153, 2093–2101.
- Lupien, S.J.; Maheu, F.; Tu, M.; Fiocco, A.; Schramek, T.E. The Effects of Stress and Stress Hormones on Human Cognition: Implications for the Field of Brain and Cognition. Brain Cogn. 2007, 65, 209–237.
- Belelli, D.; Herd, M.B.; Mitchell, E.A.; Peden, D.R.; Vardy, A.W.; Gentet, L.; Lambert, J.J. Neuroactive Steroids and Inhibitory Neurotransmission: Mechanisms of Action and Physiological Relevance. Neuroscience 2006, 138, 821–829.
- Rasmusson, A.M.; Pineles, S.L.; Brown, K.D.; Pinna, G. A Role for Deficits in GABAergic Neurosteroids and Their Metabolites with NMDA Receptor Antagonist Activity in the Pathophysiology of Posttraumatic Stress Disorder. J. Neuroendocrinol. 2022, 34, e13062.
- Callaghan, B.L.; Tottenham, N. The Stress Acceleration Hypothesis: Effects of Early-Life Adversity on Emotion Circuits and Behavior. Curr. Opin. Behav. Sci. 2016, 7, 76–81.
- Belsky, J. Early-Life Adversity Accelerates Child and Adolescent Development. Curr. Dir. Psychol. Sci. 2019, 28, 241–246.
- Gee, D.G.; Gabard-Durnam, L.J.; Flannery, J.; Goff, B.; Humphreys, K.L.; Telzer, E.H.; Hare, T.A.; Bookheimer, S.Y.; Tottenham, N. Early Developmental Emergence of Human Amygdala-Prefrontal Connectivity after Maternal Deprivation. Proc. Natl. Acad. Sci. USA 2013, 110, 15638–15643.
- Gee, D.G.; Humphreys, K.L.; Flannery, J.; Goff, B.; Telzer, E.H.; Shapiro, M.; Hare, T.A.; Bookheimer, S.Y.; Tottenham, N. A Developmental Shift from Positive to Negative Connectivity in Human Amygdala-Prefrontal Circuitry. J. Neurosci. Off. J. Soc. Neurosci. 2013, 33, 4584–4593.
- Keding, T.J.; Herringa, R.J. Paradoxical Prefrontal–Amygdala Recruitment to Angry and Happy Expressions in Pediatric Posttraumatic Stress Disorder. Neuropsychopharmacology 2016, 41, 2903–2912.
- Wu, M.; Kujawa, A.; Lu, L.H.; Fitzgerald, D.A.; Klumpp, H.; Fitzgerald, K.D.; Monk, C.S.; Phan, K.L. Age-Related Changes in Amygdala-Frontal Connectivity during Emotional Face Processing from Childhood into Young Adulthood. Hum. Brain Mapp. 2016, 37, 1684–1695.
- Ono, M.; Kikusui, T.; Sasaki, N.; Ichikawa, M.; Mori, Y.; Murakami-Murofushi, K. Early Weaning Induces Anxiety and Precocious Myelination in the Anterior Part of the Basolateral Amygdala of Male Balb/c Mice. Neuroscience 2008, 156, 1103–1110.
- Fani, N.; King, T.Z.; Brewster, R.; Srivastava, A.; Stevens, J.S.; Glover, E.M.; Norrholm, S.D.; Bradley, B.; Ressler, K.J.; Jovanovic, T. Fear-Potentiated Startle during Extinction Is Associated with White Matter Microstructure and Functional Connectivity. Cortex J. Devoted Study Nerv. Syst. Behav. 2015, 64, 249–259.
- Tottenham, N.; Hare, T.A.; Quinn, B.T.; McCarry, T.W.; Nurse, M.; Gilhooly, T.; Millner, A.; Galvan, A.; Davidson, M.C.; Eigsti, I.-M.; et al. Prolonged Institutional Rearing Is Associated with Atypically Large Amygdala Volume and Difficulties in Emotion Regulation. Dev. Sci. 2010, 13, 46–61.
- Troller-Renfree, S.V.; Barker, T.V.; Pine, D.S.; Fox, N.A. Cognitive Functioning in Socially Anxious Adults: Insights from the NIH Toolbox Cognition Battery. Front. Psychol. 2015, 6, 764.
This entry is offline, you can click here to edit this entry!
