Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Bariatric surgery (BS) is the most effective treatment in patients with severe obesity in terms of durable weight loss and reduction of comorbidity burden and mortality. Pre-operative weight loss can limit anesthesiological and surgical risks. Ketogenic diet (KD) is an “umbrella term” under which different low-carbohydrate dietary protocols are included. The effect of KD for preoperative weight reduction in BS is described.
- ketogenic diet
- VLCKD
- bariatric surgery
1. Introduction
Bariatric surgery (BS) is the most effective treatment in patients with severe obesity in terms of durable weight loss and the reduction of comorbidity burden and mortality [1][2].
Among the different surgical techniques, Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) are the most commonly used [3] and they are usually performed laparoscopically [4], but in these patients surgical laparoscopic procedures represent a challenge because of the thickness of the abdominal wall, the considerable accumulation of visceral adipose tissue and the increased liver volume [5]. As a matter of fact, despite the overall low mortality rate, surgical complications such as anastomotic leakage, bleeding and infections remain quite common (5–20%) [6]. The excess of visceral fat increases the risk of surgical complications and also increases the conversion rate and operative time [7]. For example, an enlarged liver and the accumulation of visceral fat may hamper the surgical field and this is the cause of the conversions in RYGB in approximately 50% of conversions cases [8]. Moreover, a large neck circumference (>44 cm) often results in difficult intubation and problems with mechanical ventilation [9].
It has been reported that immediate pre-operative weight loss can limit anesthesiological and surgical risks [10] and also seems to improve short- and long-term outcomes [11], but its role is still matter of discussion [12]. In 2016 the American Society for Metabolic and Bariatric Surgery stated that “insurance-mandated preoperative weight loss is not supported by medical evidence and has not been shown to be effective for preoperative weight loss before BS or to provide any benefit for bariatric outcomes” [13]. Indeed, there is a lack of multicenter, randomized, controlled trials on this specific topic [14], so most of the evidence on the effects of pre-operative weight loss come from retrospective studies. Thus, at present, guidelines do not provide any conclusive indication about pre-operative weight reduction [15][16].
Different approaches used to induce weight loss before surgery have been investigated, such as pharmacotherapy with glucagon-like peptide-1 receptor agonists (GLP-1 RAs) [17] or the combination of a hypocaloric diet with intragastric balloon placement [18], which significantly decreased the rate of conversions and complications in a case-control study [19]. However, diet is probably the most common approach in clinical practice and previous studies have already described the beneficial effect of a Mediterranean diet on weight loss before and after BS [20][21]. Some authors have reported that patients who show greater adherence to a diet before surgery are also those who lose more weight after surgery, for example, following a low-calorie diet (LCD) [22]. For patients at higher risk, in order to obtain more rapid weight reductions, a very-low-calorie diet (VLCD), characterized by a daily caloric intake of about 600–800 kcal, may be a valid option [23].
Another interesting dietary approach that is more and more frequently used is a ketogenic diet (KD). KD is an “umbrella term” under which different low-carbohydrate dietary protocols are included. The common feature of these diets is that most of the caloric intake is derived from proteins and fats, inducing a fasting-like state with the development of physiological ketosis. For example, a very-low-calorie ketogenic diet (VLCKD) is characterized by a very important reduction in carbohydrate consumption (less than 50 g per day, providing approximately 13% of caloric intake), with adequate protein introduction (about 0.8–1.2 g for each kg of ideal body weight, providing approximately 45% of caloric intake) and a relatively increased consumption of fats (approximately 42% of caloric intake), with an average energy intake of 800 kcal/day [24] (Figure 1). KD is gaining growing popularity because patients usually report satisfaction with this nutritional approach, probably because ketone bodies have anorexigenic, euphoric and mood-stabilizing effects which lead to the reduction of hunger and a feeling of rapid satiety [25].
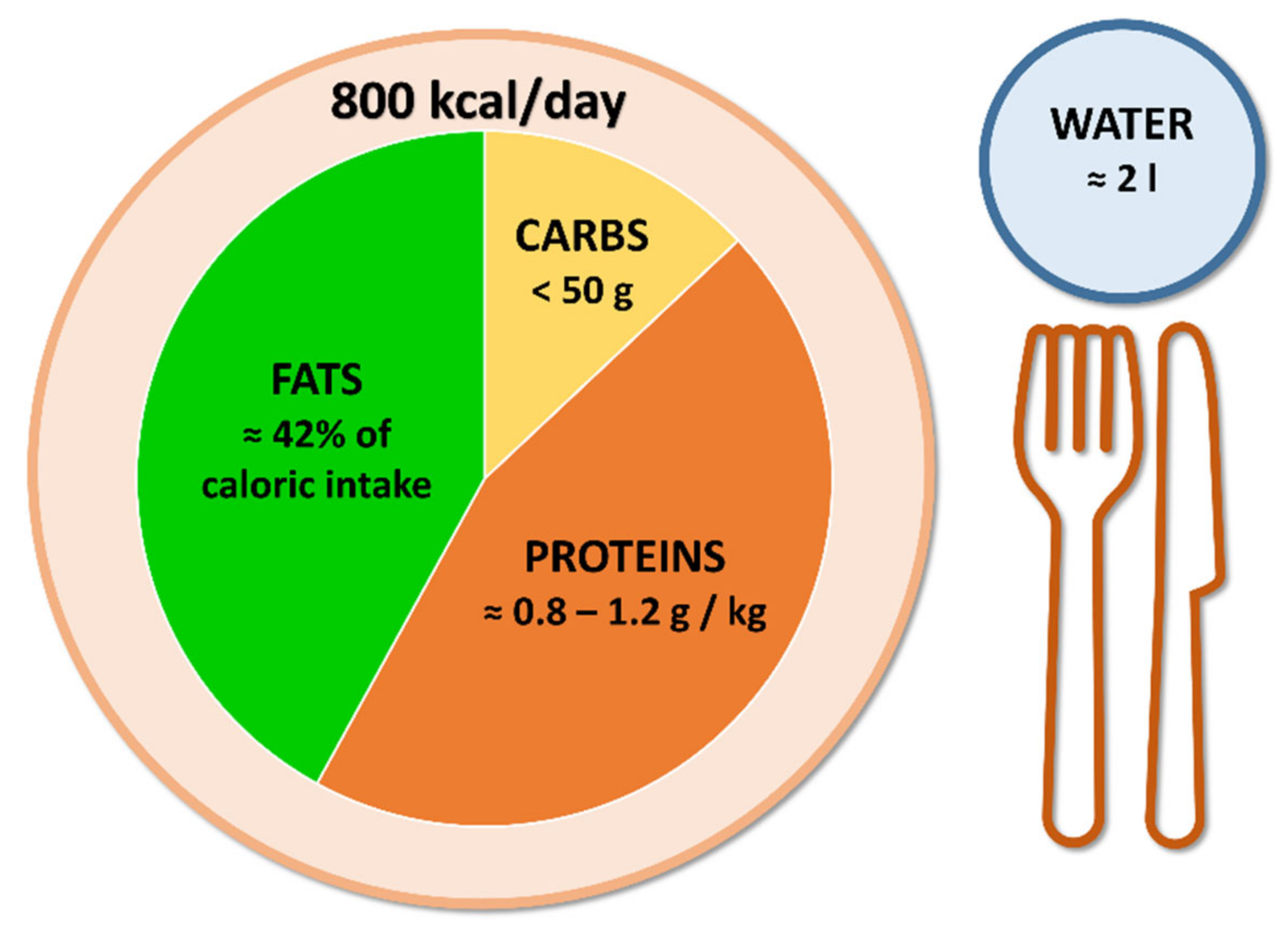
Figure 1. Very-low-calorie ketogenic diet principles.
Originally used to treat epilepsy in children [26], KD has been demonstrated to be a valid tool for weight management in patients with obesity. Particularly, a recent metaanalysis [27] reported that VLCKD is associated with a mean BMI reduction of 3.25 kg/m2 (95% CI: 2.63 to 3.86) already at 1-month follow-up and up to 7.11 kg/m2 (95% CI: 5.38 to 8.84) after 12-month follow-up, which are also very encouraging results for individuals who are not planning to undergo bariatric surgery. Significant reductions have also been reported in glycated haemoglobin (HbA1c) of 0.43% (95% CI: 0.16 to 0.70) and in low density lipoprotein (LDL) cholesterol of 9.04 mg/dL (95% CI: 4.15 to 13.94), which makes VLCKD a valid nutritional strategy for cardiovascular disease prevention as well, although these results are not superior in comparison with other weight loss interventions.
Overall, KD has proven to be a valid strategy to induce rapid weight loss [28] and its use before surgery, especially in short-time-available conditions, is particularly attractive [29].
2. Current Evidence and Future Perspectives
The results obtained from studies on KD before BS are summarized in Table 1.
Table 1. Main findings of studies on KD before BS.
| Reference | Population | Intervention Description and Duration | Control Group | Main Findings |
|---|---|---|---|---|
| Leonetti F et al., 2014 [30] | 50 patients (31 F/19 M) |
OPOD regimen: VLCKD for 10 days, VLCD for 10 days, LCD for 10 days |
30 patients (18 F/12 M) standard LCD for 30 days |
Reduction in BMI from 53.5 ± 8.4 kg/m2 to 49.2 ± 8.7 kg/m2 (p < 0.001); improvement in fasting plasma glucose levels; mean 30% reduction in liver volume; improvement of steatosis pattern. |
| Pilone V et al., 2018 [31] | 119 patients (75 F/44 M) |
Sequential diet regimen: VLCKD for 10 days, hypocaloric scheme for 20 days. In addition: multimineral and multivitamin supplements. |
Absent | Reduction in BMI from 41.5 ± 7.6 kg/m2 to 34.1 ± 5.2 kg/m2 (p < 0.001); reduction of fat mass; preservation of fat-free mass; mean 30% reduction in liver volume; improvement of steatosis pattern. |
| Schiavo L et al., 2018 [32] | 27 patients (17 F/10 M) |
Ketogenic micronutrient-enriched diet for 4 weeks | Absent | Reduction in BMI from 46.9 ± 11.7 kg/m2 to 43.0 ± 13.4 kg/m2 (p < 0.001) in females; reduction in BMI from 44.5 ± 10.5 kg/m2 to 40.6 ± 6.5 kg/m2 (p < 0.001) in males; mean 19.8% reduction of left hepatic lobe; improvement in micronutrient status. |
| Albanese A et al., 2019 [33] | 72 patients (60 F/12 M) |
VLCKD for 3 weeks | 106 patients (79 F/27 M) VLCD for 3 weeks |
Total weight loss better in VLCKD than in VLCD group (5.8 ± 2.4 vs. 4.8 ± 2.5 kg, p = 0.008). Surgical outcomes: mean operative time slightly shorter in VLCKD group; percentage of patients requiring a longer-than-anticipated hospital stay lower in VLCKD group; lower drainage output and higher post-operative hemoglobin levels in VLCKD group. |
| Schiavo L et al., 2022 [34] | 34 patients (12 F/22 M) |
CPAP + LCKD for 4 weeks | 36 patients (14 F/22 M) CPAP for 4 weeks |
Apnea-hypopnea score improved in both groups; reduction in BMI (from 50.1 ± 5.9 kg/m2 to 45.3 ± 6.5 kg/m2, p < 0.001) was observed only in CPAP + LCKD group; reduction in CRP levels, blood pressure, HOMA index and cholesterol levels were observed only in CPAP + LCKD group. |
F: females. M: males.
Abbreviations: BMI, body mass index; CPAP, continuous positive airway pressure; CRP, c-reactive protein; F, females; HOMA, homeostasis model assessment; LCD, low-calorie diet; LCKD, low-calorie ketogenic diet; M, males; OPOD, obese pre-operative diet; VLCD, very-low-calorie diet; VLCKD, very-low-calorie ketogenic diet.
Altogether, these studies confirm the usefulness of losing weight before BS and show the potential advantages of VLCKD (Figure 2), particularly if associated with micronutrient integration.
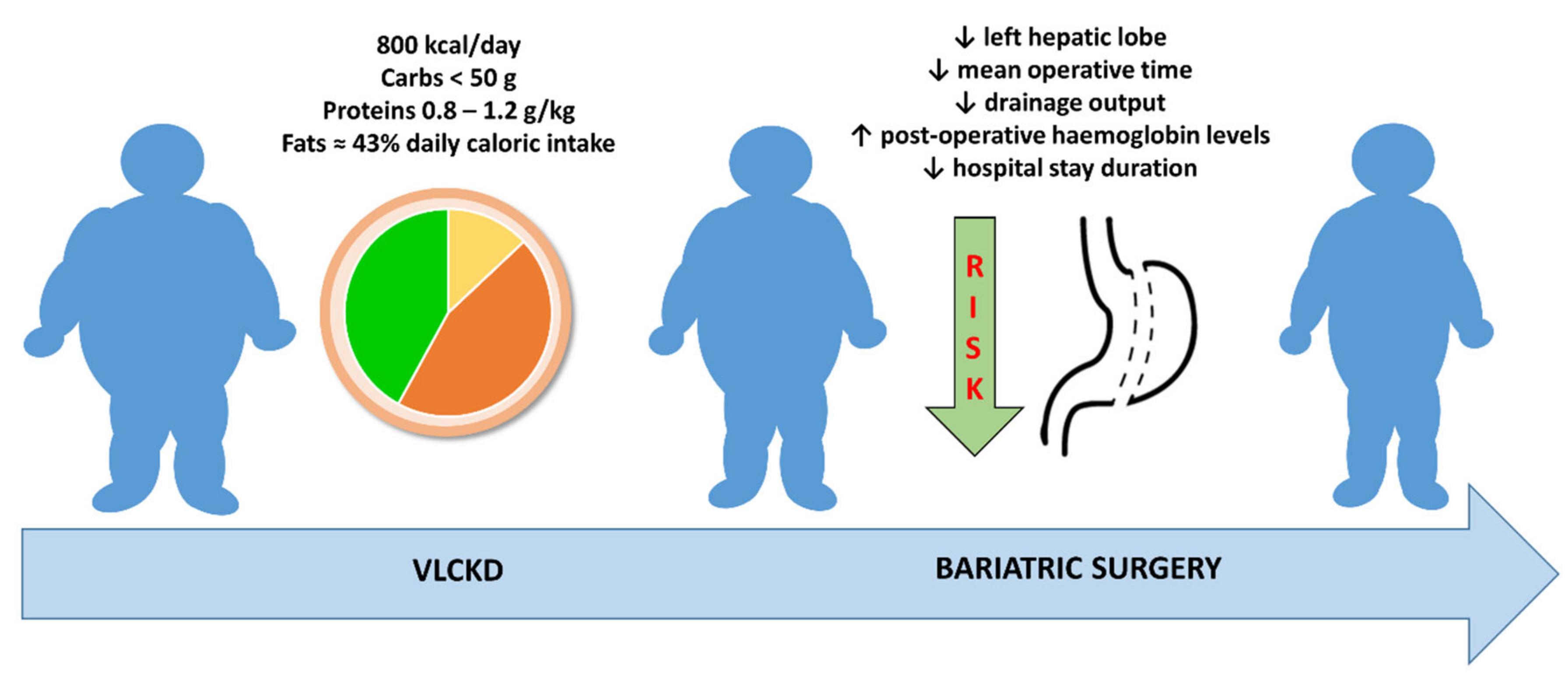
Figure 2. A very-low-calorie ketogenic diet can be a valid tool to induce weight loss before bariatric surgery, leading to the reduction of surgical risks.
However, the current evidence has some limitations. First of all, the studies presented here are highly heterogeneous in terms of the intervention proposed: because of the small number of studies regarding this subject, we decided to take in consideration not only better-defined protocols such as VLCKD [35] but also more generic KDs. Similarly, studies evaluated different outcomes in addition to weight loss, varying from micronutrient status to drainage output. The designs of the studies and the absence of a control group did not allow us to obtain an understanding of the advantages exclusive to KD, other than those generically provided by weight loss. Particularly, regarding improved surgical outcomes, there could be many other explanations other than diet that were not properly analyzed. The number of patients included in these studies is limited and most of the patients were female. Finally, the absence of a follow-up excludes the possibility of investigating potential post-surgery effects. In fact, the reported outcomes should be considered associations rather than being causally related to KD. These issues can be addressed in future research, with the planning of randomized controlled trials with clearly defined dietary protocols, larger populations (with both genders equally represented), clinically relevant outcomes and longer follow-up times to evaluate potential effects that have not yet been investigated.
This entry is adapted from the peer-reviewed paper 10.3390/nu14173610
References
- Sjöström, L. Review of the key results from the Swedish Obese Subjects (SOS) trial—A prospective controlled intervention study of bariatric surgery. J. Intern. Med. 2013, 273, 219–234.
- Sjöström, L.; Peltonen, M.; Jacobson, P.; Sjöström, C.D.; Karason, K.; Wedel, H.; Ahlin, S.; Anveden, Å.; Bengtsson, C.; Bergmark, G.; et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012, 307, 56–65.
- Perrone, F.; Bianciardi, E.; Ippoliti, S.; Nardella, J.; Fabi, F.; Gentileschi, P. Long-term effects of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for the treatment of morbid obesity: A monocentric prospective study with minimum follow-up of 5 years. Updates Surg. 2017, 69, 101–107.
- Sundbom, M. Laparoscopic revolution in bariatric surgery. World J. Gastroenterol. 2014, 20, 15135–15143.
- Riess, K.P.; Baker, M.T.; Lambert, P.J.; Mathiason, M.A.; Kothari, S.N. Effect of preoperative weight loss on laparoscopic gastric bypass outcomes. Surg. Obes. Relat. Dis. 2008, 4, 704–708.
- Picot, J.; Jones, J.; Colquitt, J.L.; Gospodarevskaya, E.; Loveman, E.; Baxter, L.; Clegg, A. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: A systematic review and economic evaluation. Health Technol. Assess. 2009, 13, 1–190, 215–357.
- Tarnoff, M.; Kaplan, L.M.; Shikora, S. An evidenced-based assessment of preoperative weight loss in bariatric surgery. Obes. Surg. 2008, 18, 1059–1061.
- Schwartz, M.L.; Drew, R.L.; Chazin-Caldie, M. Laparoscopic Roux-en-Y gastric bypass: Preoperative determinants of prolonged operative times, conversion to open gastric bypasses, and postoperative complications. Obes. Surg. 2003, 13, 734–738.
- Gonzalez, H.; Minville, V.; Delanoue, K.; Mazerolles, M.; Concina, D.; Fourcade, O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth. Analg. 2008, 106, 1132–1136.
- Gerber, P.; Anderin, C.; Thorell, A. Weight loss prior to bariatric surgery: An updated review of the literature. Scand. J. Surg. 2015, 104, 33–39.
- Livhits, M.; Mercado, C.; Yermilov, I.; Parikh, J.A.; Dutson, E.; Mehran, A.; Ko, C.Y.; Gibbons, M.M. Does weight loss immediately before bariatric surgery improve outcomes: A systematic review. Surg. Obes. Relat. Dis. 2009, 5, 713–721.
- Schiavo, L.; Sans, A.; Scalera, G.; Barbarisi, A.; Iannelli, A. Why Preoperative Weight Loss in Preparation for Bariatric Surgery Is Important. Obes. Surg. 2016, 26, 2790–2792.
- Kim, J.J.; Rogers, A.M.; Ballem, N.; Schirmer, B. ASMBS updated position statement on insurance mandated preoperative weight loss requirements. Surg. Obes. Relat. Dis. 2016, 12, 955–959.
- Bettini, S.; Belligoli, A.; Fabris, R.; Busetto, L. Diet approach before and after bariatric surgery. Rev. Endocr. Metab. Disord. 2020, 21, 297–306.
- Mechanick, J.I.; Apovian, C.; Brethauer, S.; Garvey, W.T.; Joffe, A.M.; Kim, J.; Kushner, R.F.; Lindquist, R.; Pessah-Pollack, R.; Seger, J.; et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures—2019 update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg. Obes. Relat. Dis. 2020, 16, 175–247.
- Fried, M.; Yumuk, V.; Oppert, J.-M.; Scopinaro, N.; Torres, A.J.; Weiner, R.; Yashkov, Y.; Frühbeck, G. Interdisciplinary European Guidelines on metabolic and bariatric surgery. Obes. Facts 2013, 6, 449–468.
- Tang, T.; Abbott, S.; Le Roux, C.W.; Wilson, V.; Singhal, R.; Bellary, S.; Tahrani, A.A. Preoperative weight loss with glucagon-like peptide-1 receptor agonist treatment predicts greater weight loss achieved by the combination of medical weight management and bariatric surgery in patients with type 2 diabetes: A longitudinal analysis. Diabetes Obes. Metab. 2018, 20, 745–748.
- Adrianzén Vargas, M.; Fernández, N.C.; Serrano, J.O. Preoperative weight loss in patients with indication of bariatric surgery: Which is the best method? Nutr. Hosp. 2011, 26, 1227–1230.
- Busetto, L.; Segato, G.; De Luca, M.; Bortolozzi, E.; Maccari, T.; Magon, A.; Inelmen, E.M.; Favretti, F.; Enzi, G. Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: A case-control study. Obes. Surg. 2004, 14, 671–676.
- Gastaldo, I.; Casas, R.; Moizé, V. Clinical Impact of Mediterranean Diet Adherence before and after Bariatric Surgery: A Narrative Review. Nutrients 2022, 14, 393.
- Schiavo, L.; Scalera, G.; Sergio, R.; De Sena, G.; Pilone, V.; Barbarisi, A. Clinical impact of Mediterranean-enriched-protein diet on liver size, visceral fat, fat mass, and fat-free mass in patients undergoing sleeve gastrectomy. Surg. Obes. Relat. Dis. 2015, 11, 1164–1170.
- Hutcheon, D.A.; Hale, A.L.; Ewing, J.A.; Miller, M.; Couto, F.; Bour, E.S.; Cobb, W.S.; Scott, J.D. Short-Term Preoperative Weight Loss and Postoperative Outcomes in Bariatric Surgery. J. Am. Coll. Surg. 2018, 226, 514–524.
- Hollis, G.; Franz, R.; Bauer, J.; Bell, J. Implementation of a very low calorie diet program into the pre-operative model of care for obese general elective surgery patients: Outcomes of a feasibility randomised control trial. Nutr. Diet 2020, 77, 490–498.
- Cicero, A.F.; Benelli, M.; Brancaleoni, M.; Dainelli, G.; Merlini, D.; Negri, R. Middle and Long-Term Impact of a Very Low-Carbohydrate Ketogenic Diet on Cardiometabolic Factors: A Multi-Center, Cross-Sectional, Clinical Study. High Blood Press. Cardiovasc. Prev. 2015, 22, 389–394.
- Ricci, A.; Idzikowski, M.A.; Soares, C.N.; Brietzke, E. Exploring the mechanisms of action of the antidepressant effect of the ketogenic diet. Rev. Neurosci. 2020, 31, 637–648.
- Freeman, J.M.; Kossoff, E.H.; Hartman, A.L. The ketogenic diet: One decade later. Pediatrics 2007, 119, 535–543.
- Muscogiuri, G.; El Ghoch, M.; Colao, A.; Hassapidou, M.; Yumuk, V.; Busetto, L.; Obesity Management Task Force (OMTF) of the European Association for the Study of Obesity (EASO). European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes. Facts 2021, 14, 222–245.
- Cappello, G.; Franceschelli, A.; Cappello, A.; De Luca, P. Ketogenic enteral nutrition as a treatment for obesity: Short term and long term results from 19,000 patients. Nutr. Metab. 2012, 9, 96.
- Tabesh, M.R.; Maleklou, F.; Ejtehadi, F.; Alizadeh, Z. Nutrition, Physical Activity, and Prescription of Supplements in Pre- and Post-bariatric Surgery Patients: A Practical Guideline. Obes. Surg. 2019, 29, 3385–3400.
- Leonetti, F.; Campanile, F.C.; Coccia, F.; Capoccia, D.; Alessandroni, L.; Puzziello, A.; Coluzzi, I.; Silecchia, G. Very low-carbohydrate ketogenic diet before bariatric surgery: Prospective evaluation of a sequential diet. Obes. Surg. 2015, 25, 64–71.
- Pilone, V.; Tramontano, S.; Renzulli, M.; Romano, M.; Cobellis, L.; Berselli, T.; Schiavo, L. Metabolic effects, safety, and acceptability of very low-calorie ketogenic dietetic scheme on candidates for bariatric surgery. Surg. Obes. Relat. Dis. 2018, 14, 1013–1019.
- Schiavo, L.; Pilone, V.; Rossetti, G.; Barbarisi, A.; Cesaretti, M.; Iannelli, A. A 4-Week Preoperative Ketogenic Micronutrient-Enriched Diet Is Effective in Reducing Body Weight, Left Hepatic Lobe Volume, and Micronutrient Deficiencies in Patients Undergoing Bariatric Surgery: A Prospective Pilot Study. Obes. Surg. 2018, 28, 2215–2224.
- Albanese, A.; Prevedello, L.; Markovich, M.; Busetto, L.; Vettor, R.; Foletto, M. Pre-operative Very Low Calorie Ketogenic Diet (VLCKD) vs. Very Low Calorie Diet (VLCD): Surgical Impact. Obes. Surg. 2019, 29, 292–296.
- Schiavo, L.; Pierro, R.; Asteria, C.; Calabrese, P.; Di Biasio, A.; Coluzzi, I.; Severino, L.; Giovanelli, A.; Pilone, V.; Silecchia, G. Low-Calorie Ketogenic Diet with Continuous Positive Airway Pressure to Alleviate Severe Obstructive Sleep Apnea Syndrome in Patients with Obesity Scheduled for Bariatric/Metabolic Surgery: A Pilot, Prospective, Randomized Multicenter Comparative Study. Obes. Surg. 2022, 32, 634–642.
- Muscogiuri, G.; Barrea, L.; Laudisio, D.; Pugliese, G.; Salzano, C.; Savastano, S.; Colao, A. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J. Transl. Med. 2019, 17, 356.
This entry is offline, you can click here to edit this entry!
