Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Oncology
Brain metastasis occurs in primary cancers, such as breast cancer, and is correlated with mortality. There are limited options available for treatment, but Clostridium perfringens Enterotoxin (CPE) and its interaction with Claudin-4, a possible diagnostic biomarker for breast cancer, can provide a molecular pathway basis for the development of treatment options for metastatic brain cancer.
- Claudin-4
- clostridium perfringens enterotoxin (CPE)
- brain cancer
1. Introduction
Clostridium perfringens (C. perfringens) is a spore-forming gram-positive bacterium that naturally exists in the environment in soil, sewage, and the guts of humans and animals [1]. C. perfringens is known for its role as a common disease-causing agent of food poisoning, diarrhea, and other gastrointestinal illnesses [2]. Clostridium perfringens type-A bacteria produce several toxins, prominent among these is Clostridium perfringens enterotoxin (CPE) which is the causative agent in antibiotic-associated diarrhea and symptoms linked to common gastrointestinal food-borne illnesses [3]. CPE creates pores in intestinal and colonic epithelial cells, rendering them permeable to an influx of Ca2+ and consequent cellular damage [4].
Functionally, CPE consists of two main domains: the pore-forming NH2-terminal region and the Claudin-binding c-CPE. By forming pores in the cytoplasmic membrane of mammalian host cells, the N-terminal region of CPE disrupts osmotic equilibrium and mediates a cytotoxic effect [5]. CPE and Claudin-4 have aromatic and hydrophobic interactions rather than hydrogen bonding, and Tyr306 is crucial to this binding [6]. CPE binds initially to the receptor proteins, creating a small (90 kDa) precursor complex which forms a larger SDS-resistant complex (155 kDa) that induces altered permeability in the cell membranes of sensitive mammalian cells [7]. The resulting modifications in cellular membrane permeability generate a calcium influx, triggering rapid apoptosis or oncosis. A hexameric prepore on the cell membrane is assembled first and then beta-hairpin loops generate a beta-barrel that infixes into the membrane, intensifying calcium influx through the active pore. Subsequent cell death causes fluid and electrolyte loss and damage to the intestines [8].
2. Use of C-Terminal CPE as a Therapeutic Agent in Brain Metastasis from Breast Cancer
2.1. Claudin-4 and C-CPE Interactions in Cancer Cells
CPE toxin is lethal for cells high in Claudin-4 expression. CPE gene transfer in vitro and in vivo, using the bacterial wild-type CPE cDNA (wtCPE) or optCPE cDNA, selectively killed tumor cells overexpressing Claudin-4. The expression of optCPE was more efficient and demonstrated quick cytotoxic activity, heightened by the bystander effect of CPE release. Up to 100% cytotoxicity in tumor lines expressing Claudin-4 specifically was reported 72 h following the transfer of CPE genes [49]. In vitro CPE treatment of breast cancer cell lines (MDA-MB-468, MCF-7, NT2.5-Luc) and normal human astrocytes led to a dose-dependent and accelerated cytolysis solely in breast cancer cells. The extent of cytolysis was limited by Claudin-4 expression [48]. Furthermore, the intracranial administration of CPE into breast metastatic cancer cells in the brain—using the murine model with brain tumors from the human breast cancer cell line MDA-MB-468 and the murine breast cancer cell line NT2.5-Luc. —improved survival significantly in comparison to mice treated with PBS [48]. Hence, CPE in its native form can be advantageous in treating various cancers with overexpressed Claudin CPE receptors, notwithstanding that immunogenicity and bystander toxicity pose a problem. Moreover, CPE impairment of tight junctions has now been shown to result in stemness, epithelial–mesenchymal transition (EMT), activation of the Yes-associated protein (YAP), a transcriptional coactivator in oral squamous cell carcinoma, and intracellular displacement of Claudin-4 to the cytoplasmic membrane [49]. These results imply that CPE might heighten the malignant transformation of cells via YAP activation.
Alternatively, the Claudin-binding C-terminal domain of CPE (c-CPE) can be employed to reversibly regulate TJs and enhance permeability in order to permit the delivery of solutes and chemotherapeutic agents across epithelial cell sheets [50]. In the absence of the toxic pore-forming N-terminal of CPE, c-CPE protein complexes are effective and a better candidate than native CPE for cancer therapy. C-CPE peptide comprises amino acids 184 to 319 and contains the receptor-binding region at amino acids 290 to 319. The superimposition of a homology model of the human Claudin-4 apo form on the Claudin-4•c-CPE fusion protein structure revealed substantial changes in conformation when c-CPE bound with Claudin-4 in both the ECL1 and ECL2 domains [51]. c-CPE binds to and removes Claudin-4 from TJs without redistributing the unbound Claudins and damaging the plasma membrane, allowing for drug entry and absorption to occur (Figure 1) [52].
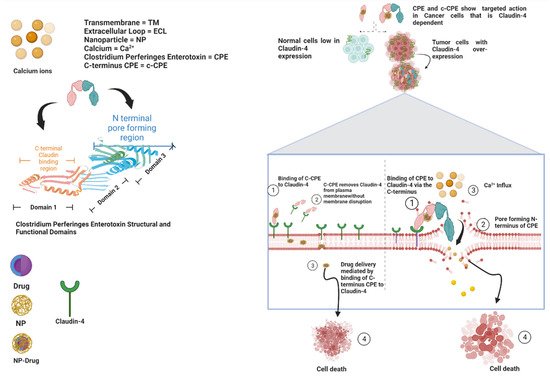
Figure 1. Diagrammatic representation of the mechanisms of CPE and c-CPE interaction with Claudin-4 and structural and functional domains of both CPE and Claudin-4.
This mechanism is much slower and more reversible because it is dependent on the c-CPE concentration [34]. Consequently, c-CPE can act as a Claudin modulator to open TJs for improved delivery of drugs across tissue membranes by disrupting TJs to increase paracellular permeability without destroying the plasma membrane integrity and incurring cytotoxicity [53,54]. For example, Polysialic acid nanoparticles conjugated to CPE peptides (C-SNPs) were recently developed for targeted therapy against pancreatic cancer. C-SNPs with loadings of doxorubicin (DOX-C-SNPs) collocate and target Claudin-4 in pancreatic cancer cells, disrupting TJs while being significantly reduced in normal pancreatic cells [55]. Similarly, nanoparticles made of the biocompatible and biodegradable polymer, Poly(lactic-co-glycolic-acid) (PLGA-NPs), altered with c-CPE (c-CPE-NPs) and transferred intraperitoneally, significantly inhibited tumor growth in ovarian cancer cells without much activity in normal ovarian cells [56]. Moreover, c-CPE mutants have shown exclusive binding capabilities to Claudin-4. For instance, c-CPE 194 is a c-CPE mutant that binds only to Claudin-4 and enhances the effectiveness of anticancer agents. In well-differentiated HPAC (a pancreatic cancer cell line) duct epithelial cells, c-CPE 194 interrupted barrier functions without changing Claudin-4 expression while increasing MAPK phosphorylation. c-CPE 194 also augmented the cytotoxicity of gemcitabine and S-1 (two anticancer drugs), reduced the expression of Claudin-4, and improved MAPK activity in a poorly differentiated pancreatic cancer cell line, PANC-1. In normal human pancreatic duct epithelial cells, c-CPE 194 diminished Claudin-4 expressions and improved the MAPK activity without impacting the cytotoxicity of the anticancer drugs [57]. In breast cancer cells, c-CPE fused to protein synthesis inhibitory factor (PSIF) showed cytotoxicity leading to dose-dependent cell death in MCF-7 human breast cancer cells but not in mouse fibroblast L cells due to the presence of Claudin-4 in the breast cancer cells and the absence in mouse fibroblast L cells [58]. c-CPE also shows Claudin-4 dependence in mediating its cytotoxicity in breast cancer cells [58]. c-CPE binding, which correlated with the expression of Claudin-4, aids the cytotoxic actions of carboplatin and paclitaxel by sensitizing epithelial ovarian cancer cells. c-CPE significantly increased tumor suppression through the inhibition of tumor cell proliferation and acceleration of tumor apoptosis when added to carboplatin and paclitaxel compared to when the anticancer agents were used independently [54]. Modulation of Claudins by c-CPE increases drug absorption by 400-fold when compared to sodium caprate, an absorption enhancer utilized in the clinic [59]. Additionally, Claudin-4 positive human ovarian carcinoma cells experienced a 6.7-fold elevation in toxicity when treated with a fusion of recombinant c-CPE and tumor necrosis factor (TNF) than with TNF alone [60]. Recombinant c-CPE-proteins can thus be developed as TJ modulators for enhanced delivery of drugs into breast cancer and brain metastatic cells overexpressing Claudin-4. The treatment of breast cancer cells and brain metastasis with c-CPE in its various forms is effective because Claudin-4 is steadily expressed in those cancers. Furthermore, Claudin-4 expression in normal areas of the central nervous system (CNS) is negligible, which restricts apoptosis exclusively to brain tumor cells and hinders tumor growth [48]. c-CPE thus has theranostic value.
2.2. Crossing the Blood–Brain Barrier
The blood–brain barrier (BBB) hinders the passage of neurotoxic substances and drugs into the brain. c-CPE has been modified in studies to transiently open and cross the BBB by binding to Claudin-5 (Cldn-5) in the endothelial TJs that form the paracellular barrier in BBB [61,62,63]. Recently, several different approaches have been undertaken to enhance the uptake of chemotherapeutic agents into malignant tumors, including conjugating drugs to micelles, liposomes, dendrimers, and nanoparticles—which may be proteinaceous, polymeric, or inorganic—that can cross the BBB [64]. The uniqueness of each drug delivery system lies within its bioavailability, hydrophilicity, biocompatibility, membrane permeability, and biodegradability [65]. Notably, nontoxicity and the capacity for localization to tumor sites are important when considering the suitability of drug delivery techniques in cancer treatment. Preferably, an ideal drug delivery vehicle would be nontoxic, able to solubilize in the body, permeable to the tissue barriers, biodegradable, and capable of providing direct, targeted, and sustained effects against tumor cells [66]. Using Claudin-4 as a target for fluorescent molecules, c-CPE bound to NP (c-CPE NP) can be further localized and administered intraperitoneally (IP) in breast cancer cells to significantly lessen systemic toxicity than with the same dose administered intravenously. Further, CPE-expressing vectors can be utilized to transfer genes intratumorally for selective suicide gene therapy of chemotherapy-resistant cells in tumors expressing Claudin-4. For instance, in ovarian cancer resistant to IP chemotherapy, fluorescent FITC conjugated to CPE accumulated predominantly in the ovarian tumor and not the normal ovarian cells [39]. Furthermore, c-CPE-NPs were used to deliver Diphtheria Toxin Subunit-A (DT-A), a therapeutic agent, via the p16 promoter highly expressed in ovarian tumors. The p16 DT-A vector enclosed in CPE-NPs (p16 DT-A c-CPE-NPs) led to cell death in ovarian cancer in vitro. IP injections of p16 DT-A c-CPE-NPs inhibited tumor growth significantly more than using control NPs in mice harboring chemotherapy-resistant tumors (p = 0.041) [56]. Nanoparticles conjugated with c-CPE thus depict a nontoxic binal-targeting approach for treating chemotherapy-resistant cancer cells via selective gene therapy and for drug delivery to non-chemo-resistant brain metastatic cancer cells. To date, there is not extensive research that shows the interaction between c-CPE conjugated to drugs in breast cancer metastasis in the brain. However, several drugs have been shown to concentrate in breast cancer metastasis in the brain, crossing the impaired BBB caused by tumorigenesis [67]. Such drugs include trastuzumab, Zr trastuzumab, C-paclitaxel, C-doxorubicin, and C-lapatinib [68,69,70,71]. As stated, c-CPE-NPs conjugated to drugs like doxorubicin and paclitaxel have shown efficacy in other cancer cell types, such as ovarian and pancreatic cell lines. Thus, c-CPE mutants that bind to Cldn-5, a major TJ protein in the BBB, and are conjugated with drug-NPs can potentially serve as a novel technique to direct cancer therapy to breast cancer metastasis in the brain.
This entry is adapted from the peer-reviewed paper 10.3390/cancers14174309
This entry is offline, you can click here to edit this entry!
