Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Prognosis involves “the prediction of the course or outcome of an existing disease, based on empirical information, as well as the ability to recover from the disease”. In dentistry, the predictive probability of dental mortality is based on the stability of the supporting tissues.
- periodontal tissue
- prognosis
- permanent teeth
1. Introduction
Oral health care is an essential part of general health and provides people with an increased quality of life [1]. Tooth loss is a serious health problem that affects the functional abilities to chew and speak, psychology, aesthetics, and even social interaction [2]. There is currently no standardized tool to assess the general condition of a tooth and predict whether it is likely to have a long half-life [3].
Prognosis involves “the prediction of the course or outcome of an existing disease, based on empirical information, as well as the ability to recover from the disease” [4]. In dentistry, the predictive probability of dental mortality is based on the stability of the supporting tissues [5]. Various researchers postulate that the prognosis is complex, established before treatment, and is supported by clinical and radiographic findings, as well as factors related to the patient, and general factors, such as the systemic condition (diabetes mellitus, smoking habit, motivation, and commitment of the patient) and local factors (factors anatomical, caries, furcation involvement, tooth mobility, periodontal support, pulp involvement, and bone loss) [4]. Prognosis is a dynamic process and should be reassessed, according to the progression of treatment and maintenance of the teeth [3][5].
Understanding the complexity of the prognosis in treatment planning would benefit both the patient and the professional when dealing with other patients facing the same clinical scenario. The development of uniform concepts will facilitate dental education and improve patient care [6].
In recent decades, scientific documentation has positioned implants as the first treatment option in edentulous patients, influencing the decision to extract periodontally compromised teeth [7][8][9][10]. In ref. [11], the researchers also suggest that proactive or strategic extraction will prevent future bone destruction in a potential area for subsequent implant placement [11]. However, current evidence cannot always support decision-making, especially considering that any extracted tooth will result in alveolar bone resorption, which can occur despite the use of alveolar ridge preservation techniques or immediate implant placement [12][13][14].
On the other hand, the goal of periodontal therapy is the long-term retention of the natural tooth in a healthy, functional, aesthetically acceptable, and painless state [15]. By way of comparison, when an organ is compromised, measures are taken to prevent further damage or reverse it; however, when it involves a tooth, it is the patients and even some professionals who do not seem to value its preservation [16]. The option of retaining natural teeth, and adopting innovative and cost-effective restorative measures, can provide a practical, pragmatic, and predictable solution over time [17].
The comparison between the preservation of the natural tooth and the placement of an implant is difficult since implants should be considered as a treatment for tooth loss and not as a substitute for the tooth [12]. Clinicians are faced with the dilemma of whether to keep and treat a tooth or extract and replace it with a removable or partially fixed prosthesis. They are the ones who establish the prognosis and carry out the corresponding treatment under their criteria [6].
2. Compromised Teeth Preserve or Extract
The decision to keep or extract a periodontally compromised tooth with a hopeless or questionable prognosis is not always easy to predict. Assigning a long-term prognosis is critical, particularly in the dilemma of performing appropriate rehabilitative treatments after periodontal therapy, especially if it involves major prosthetic rehabilitation or implant placement [18]. Lundgren, D. et al. postulate that postponing the insertion of implants in patients susceptible to periodontitis should be considered strategically, optimizing the longevity of the natural dentitions [19] and facilitating a global solution that can reduce the risks of long-term implant treatment [20]. It has been shown that in teeth with a hopeless prognosis or with an indication for extraction, after periodontal treatment, it is possible to stop the progression of the disease to a certain extent and minimize or even prevent tooth loss [12][21][22][23][24]. It must be considered that the population is aging, and patients no longer accept removable dentures; they expect that the dentist’s knowledge and skills will allow them to maintain healthy mouths as they age [25]. That is why the demands of the patient must be taken into consideration, but it is the clinician who establishes the treatment plan, in favor or against preserving the tooth. The patient must be fully and adequately informed to have their consent.
After reviewing the selected articles, the decision to keep or extract a tooth depends on several factors, such as the patient’s expectations, control of diabetes mellitus, socioeconomic level, age, oral hygiene, depth of periodontal probing, tooth mobility, root anomalies, furcation involvement, commitment to periodontal treatment and maintenance programs, extensive caries, smoking habit, among others [26][27]. Samet, N. et al. [3] established that the risk factors are divided into biological (systemic condition associated with the immune system and healing, alteration of salivary flow, special needs limiting oral hygiene, high count of Streptococcus mutans and Lactobacillus, family history, missing teeth), behavior (poor oral hygiene or compromised diet, cariogenic diet, low exposure to fluoride, parafunctional habits, commitment and willingness to adhere to a long-term maintenance protocol, smoking habit), and financial/personal (motivation during treatment, economic resources, time availability, attitude to tooth loss, knowledge about its condition and necessary treatments, aesthetic expectations). For example, in the study by Saminsky, M., et al. [24], the main reason when deciding whether or not the tooth should be extracted was periodontal causes; 11.7% of teeth with periodontal pockets of 4–6 mm and 37.7% with ≥7 mm were extracted (p < 0.001). Most patients (32 of 50) received two or more periodontal support treatments per year and multi-rooted teeth (17.9%) showed a higher risk of being extracted compared to single-rooted teeth (3.6%; p < 0.001). Among the patient characteristics, it was observed that age is strongly related to tooth loss, especially in patients ≥60 years old (13.9% present risk of extraction; p < 0.001). Goh, V., et al. [22] found similar results: sites with probing depth ≥6 mm were positively associated with tooth loss (p < 0.002), presenting a greater association when treatment was interrupted for several years (p < 0.001).
In this research, several articles postulate various treatment options. However, there are no randomized clinical trials available in the dental literature comparing fixed prostheses in teeth with questionable prognoses with fixed prostheses on implants. In addition, an exact comparison is not possible since each tooth is unique and determined by particular factors. For example, in the study by Tözüm, T.F. et al. [28], after performing the endodontic and periodontal treatment of the compromised tooth, the pain subsided, but the mobility persisted (grade 3). Subsequently, the extraction and intentional reimplantation were carried out, applying an autologous platelet gel inside the alveolus. This allowed a significant gain in clinical attachment level and alveolar bone level, and a total reduction in tooth mobility was observed after 18 months, without observing ankylosis or root resorption.
Another factor previously mentioned is that periodontal support therapy is considered to play an important role in tooth preservation, but the cost and efforts involved are rarely considered [29]. Progression of periodontal disease and reinfection of sites, as well as tooth loss, are possible, especially in patients susceptible to periodontitis [12]. Several factors can affect periodontal healing, such as the presence of morphological defects (a three-walled intraosseous defect will heal better than a one- or two-walled defect), tooth mobility, tissue graft treatments, dentist skills, and level of commitment of the patient [25]. In the study by Graetz, C. et al. [23], after periodontal therapy, the initial mean probing depth was 5.8 ± 2.1 mm and decreased to 3.5 ± 1.1 mm; patients who received adjuvant antibiotic therapy due to persistent inflammation showed an initially greater probing depth of 6.35 ± 2.42 mm and bone loss of >70% in 12.5% (70 teeth).
The fate of a tooth is usually influenced by the treatment planning that involves the entire dentition and the patient’s preferences, with the decision to extract or maintain it largely depending on the dentist, based on their experience and clinical judgment [26][30][31]. To achieve the ideal treatment, there are several factors to be considered during the treatment planning process. These factors include the main demand of the patient; an adequate analysis of the cost-benefit; and risks associated with oral hygiene, tobacco history, and periodontal disease [32]. Su, H. et al. consider that the factor that seems to have the greatest impact on treatment planning is the level of training of the dentist [6]. Clinicians with more than 15 years of experience prefer to perform extractions more frequently than clinicians with less than 5 years of experience [33]. On the other hand, Baba, N.Z. et al. postulate that the treatment decision should be based on satisfying the patient`s wishes and on the importance of evaluating each tooth individually to obtain the treatment with the best result in terms of aesthetics, comfort, function, and cost-effectiveness [34]. In the study by Zafiropoulos, G.G.K., et al. [35], no tooth was extracted in one of the treated patients, since he refused any extraction, opting for 6-monthly maintenance. During the last 4 years of follow-up, the multirooted teeth lost an average of 7.3 mm of clinical attachment, while in the rest of the teeth the loss was only 0.3–0.4 mm. Multirooted teeth with class III furcation involvement had a survival of 8 years.
The placement of implants to replace extracted teeth should be considered acceptable in the case of non-restorable teeth or patients with recurrent periodontal disease, with recurrences after periodontal treatment [34]. Only when the periodontal condition is stabilized and adequate bacterial plaque control is obtained, can the placement of implants be planned as an integral part of the rehabilitation [25]. This should be based on two levels of risk: (1) patient-level: gingival bleeding, the prevalence of residual pockets ≥5 mm, number of missing teeth, loss of attachment/support of the bone level concerning the patient’s age, systemic and genetic condition [34][36], and environmental factors, such as smoking; (2) site level: the presence of residual periapical lesions, alveolar bone height and quality, gingival biotype, the proximity of the anatomical structure, and condition of neighboring teeth (residual periodontal pockets, gingival bleeding and suppuration, tooth anatomy and position, compromise of furca, presence of iatrogenic factors and tooth mobility) [12][37].
It is necessary to expand research related to periodontal and dental prognosis, establish the dental condition at all times, and develop evidence-based treatment strategies [18]. In some cases, it is necessary to integrate the areas of endodontics, periodontics, and orthodontics, to maintain teeth without changing the long-term prognosis [31][38]. When deciding between keeping or replacing a tooth affected by periodontitis, it is important to consider the ability to understand and treat possible future diseases, such as peri-implantitis [32], in which treatment cannot be guaranteed to be predictable [12]. Therefore, it should be discussed whether or not a tooth with a periodontal disease without major restorative treatments should be extracted, assess the potential for success in periodontal treatment, and seriously question the advisability of replacing the tooth [32].
Another factor to consider is tooth extraction for aesthetic reasons, which will only be considered if the prosthetic restoration can significantly improve the aesthetic result and the satisfaction of the patient’s expectations (a key component in the planning of all treatments) [12]. Retaining a tooth may be advantageous in the presence of a thin biotype, unfavorable interproximal bone, or in the presence of a long-standing adjacent implant. It is likely that, after extraction of the tooth with periodontal compromise, the interdental papilla is not present, especially when the distance between the interproximal bone and the proximal contact is greater than 5 mm (>4 mm in thin biotype and >5 mm in thick biotype) [34]. The type of tooth and its position must also be considered; in particular, the molars show less improvement, associated with the complexity of the root anatomy. Martinez-Canut, P. [39] determined that the type of tooth is significantly associated with the risk of tooth loss due to periodontal disease (p < 0.001). The risk was multiplied by two in maxillary canines, maxillary incisors, and mandibular lateral incisors; and by seven in maxillary premolars, mandibular central incisors, mandibular canines, and mandibular premolars. In addition, the mandibular first molar was 2.5 times less likely to be lost than the rest of the molars. On the other hand, the absence of adjacent teeth contributed to a better result in teeth with periodontal compromise, since it facilitated the control of bacterial plaque, which must be considered clinically when deciding to extract or maintain a tooth under these conditions [40][41].
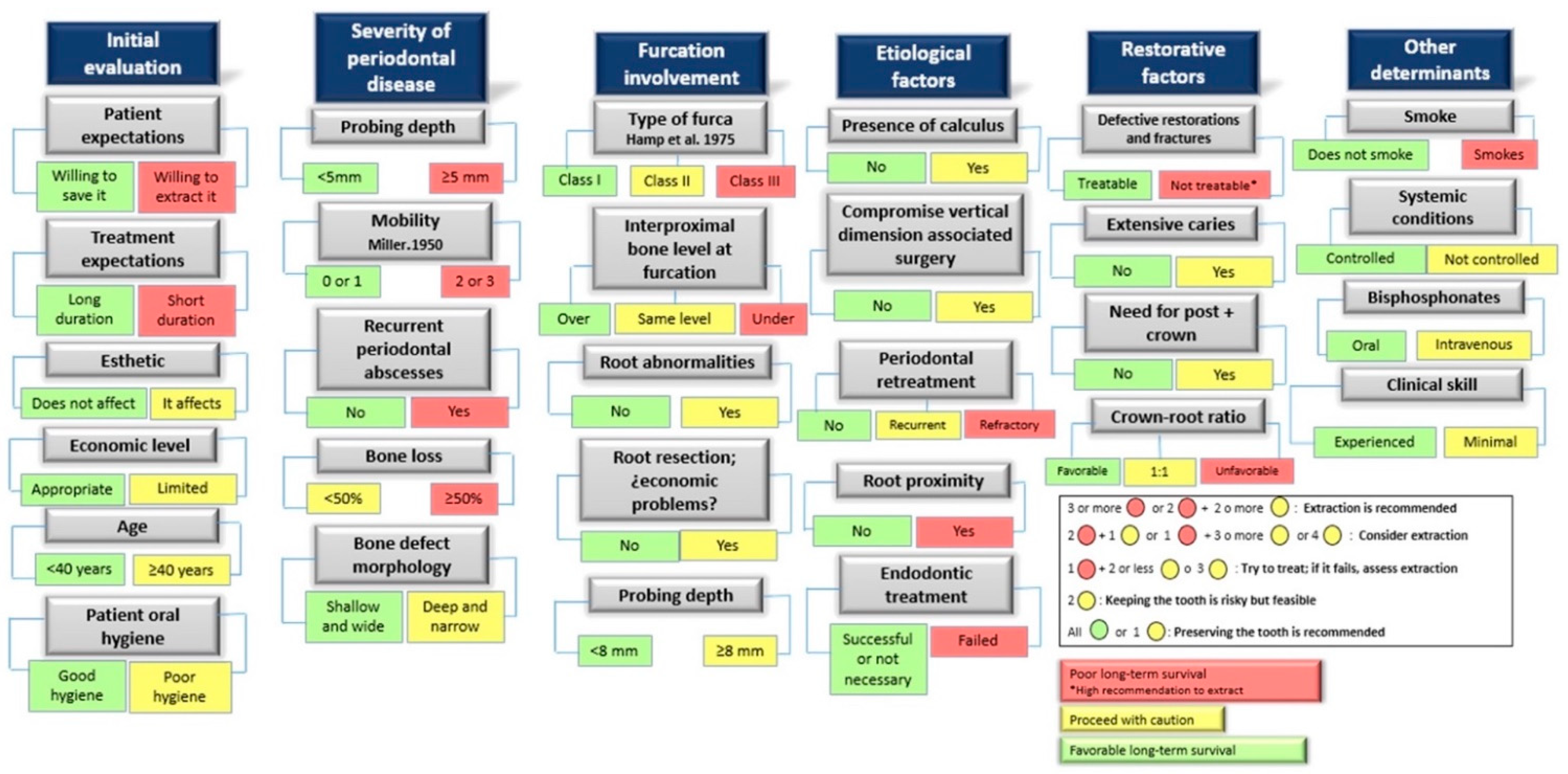
The evidence reflects that the decision to keep or extract a tooth must be multifactorial since it is an irreversible process. The periodontal status and the restorability of the affected tooth should be highlighted as the main factors for prognosis. Taking as reference the publications of Avila, G. et al., 2009 [26] and Nunn, M.E. et al., 2012 [18], researchers propose a schematic diagram of the prognostic indicators, which reflects the factors to be considered and the survival rate that each one represents, when deciding to keep or extract a tooth (Figure 1).
This entry is adapted from the peer-reviewed paper 10.3390/jcm11185301
References
- Polzer, I.; Schimmel, M.; Müller, F.; Biffar, R. Edentulism as part of the general health problems of elderly adults. Int. Dent. J. 2010, 60, 143–155.
- De Melo, M.A.; Lino, P.A.; Dos Santos, T.R.; Vasconcelos, M.; Lucas, S.D.; de Abreu, M.H. A 15-year time-series study of tooth extraction in brazil. Medicine 2015, 94, e1924.
- Samet, N.; Jotkowitz, A. Classification and prognosis evaluation of individual teeth—A comprehensive approach. Quintessence Int. 2009, 40, 377–387.
- Beck, J.D. Risk revisited. Community Dent. Oral Epidemiol. 1998, 26, 220–225.
- Kwok, V.; Caton, J.G. Commentary: Prognosis revisited: A system for assigning periodontal prognosis. J. Periodontol. 2007, 78, 2063–2071.
- Su, H.; Liao, H.; Fiorellini, J.P.; Kim, S. Factors affecting treatment planning decisions for compromised anterior teeth. Int. J. Periodontics Restor. Dent. 2014, 34, 389–398.
- Greenstein, G.; Greenstein, B.; Cavallaro, J. Prerequisite for treatment planning implant dentistry: Periodontal prognostication of compromised teeth. Compend. Contin. Educ. Dent. 2007, 28, 436–446.
- Pjetursson, B.E.; Tan, W.C.; Tan, K.; Brägger, U.; Zwahlen, M.; Lang, N.P. A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin. Oral Implants Res. 2008, 19, 131–141.
- Carlsson, G.E. Critical review of some dogmas in prosthodontics. J. Prosthodont. Res. 2009, 53, 3–10.
- Lekholm, U.; Gunne, J.; Henry, P.; Higuchi, K.; Lindén, U.; Bergström, C. Survival of the brånemark implant in partially edentulous jaws: A 10-year prospective multicenter study. Int. J. Oral Maxillofac. Implants. 1999, 14, 639–645.
- Kao, R.T. Strategic extraction: A paradigm shift that is changing our profession. J. Periodontol. 2008, 79, 971–977.
- Donos, N.; Laurell, L.; Mardas, N. Hierarchical decisions on teeth vs. implants in the periodontitis-susceptible patient: The modern dilemma. Periodontol. 2000 2012, 59, 89–110.
- Araújo, M.G.; Sukekava, F.; Wennström, J.L.; Lindhe, J. Tissue modeling following implant placement in fresh extraction sockets. Clin. Oral Implant. Res. 2006, 17, 615–624.
- Botticelli, D.; Berglundh, T.; Lindhe, J. Hard-tissue alterations following immediate implant placement in extraction sites. J. Clin. Periodontol. 2004, 31, 820–828.
- Hirschfeld, L.; Wasserman, B. A long-term survey of tooth loss in 600 treated periodontal patients. J. Periodontol. 1978, 49, 225–237.
- Park, H.; Song, H.Y.; Han, K.; Cho, K.; Kim, Y. Number of remaining teeth and health–related quality of life: The korean national health and nutrition examination survey 2010–2012. Health Qual. Life Outcomes 2019, 17, 1–10.
- Meyers, I.A. Herodontics–is there a place for maintaining the apparently hopeless tooth? Aust. Dent. J. 2019, 64, S71–S79.
- Nunn, M.E.; Fan, J.; Su, X.; Levine, R.A.; Lee, H.; McGuire, M.K. Development of prognostic indicators using classification and regression trees for survival. Periodontol. 2000 2012, 58, 134–142.
- Lundgren, D.; Rylander, H.; Laurell, L. To save or to extract, that is the question. natural teeth or dental implants in periodontitis-susceptible patients: Clinical decision-making and treatment strategies exemplified with patient case presentations. Periodontol. 2000 2008, 47, 27–50.
- Levin, L.; Halperin-Sternfeld, M. Tooth preservation or implant placement: A systematic review of long-term tooth and implant survival rates. J. Am. Dent. Assoc. 2013, 144, 1119–1133.
- D’Aiuto, F.; Ready, D.; Parkar, M.; Tonetti, M.S. Relative contribution of patient-, tooth-, and site-associated variability on the clinical outcomes of subgingival debridement. I. probing depths. J. Periodontol. 2005, 76, 398–405.
- Goh, V.; Hackmack, P.P.; Corbet, E.F.; Leung, W.K. Moderate-to long-term periodontal outcomes of subjects failing to complete a course of periodontal therapy. Aust. Dent. J. 2017, 62, 152–160.
- Graetz, C.; Sälzer, S.; Plaumann, A.; Schlattmann, P.; Kahl, M.; Springer, C.; Dörfer, C.; Schwendicke, F. Tooth loss in generalized aggressive periodontitis: Prognostic factors after 17 years of supportive periodontal treatment. J. Clin. Periodontol. 2017, 44, 612–619.
- Saminsky, M.; Halperin-Sternfeld, M.; Machtei, E.E.; Horwitz, J. Variables affecting tooth survival and changes in probing depth: A long-term follow-up of periodontitis patients. J. Clin. Periodontol. 2015, 42, 513–519.
- Caplan, D.J.; Li, Y.; Wang, W.; Kang, S.; Marchini, L.; Cowen, H.J.; Yan, J. Dental restoration longevity among geriatric and special needs patients. JDR Clin. Transl. Res. 2019, 4, 41–48.
- Avila, G.; Galindo-Moreno, P.; Soehren, S.; Misch, C.E.; Morelli, T.; Wang, H. A novel decision-making process for tooth retention or extraction. J. Periodontol. 2009, 80, 476–491.
- Halperin–Sternfeld, M.; Levin, L. Do we really know how to evaluate tooth prognosis? A systematic review and suggested approach. Quintessence Int. 2013, 44, 447–456.
- Tözüm, T.F.; Keçeli, H.G.; Serper, A.; Tuncel, B. Intentional replantation for a periodontally involved hopeless incisor by using autologous platelet-rich plasma. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, e119–e124.
- Pretzl, B.; Wiedemann, D.; Cosgarea, R.; Kaltschmitt, J.; Kim, T.S.; Staehle, H.J.; Eickholz, P. Effort and costs of tooth preservation in supportive periodontal treatment in a german population. J. Clin. Periodontol. 2009, 36, 669–676.
- D’Cruz, L. Dento-legal considerations about an MI approach. Br. Dent. J. 2017, 223, 199–201.
- Diamantatou, T.; Kotina, E.; Roussou, I.; Kourtis, S. Treatment options for anterior teeth with questionable prognosis: Critical factors in determining whether to maintain or extract. J. Esthet. Restor. Dent. 2016, 28, 157–170.
- Moshaverinia, A.; Kar, K.; Chee, W.W. Treatment planning decisions: Implant placement versus preserving natural teeth. J. Calif. Dent. Assoc. 2014, 42, 859–868.
- Saghafi, N.; Heaton, L.J.; Bayirli, B.; Turpin, D.L.; Khosravi, R.; Bollen, A. Influence of clinicians’ experience and gender on extraction decision in orthodontics. Angle. Orthod. 2017, 87, 641–650.
- Baba, N.Z.; Goodacre, C.J.; Kattadiyil, M.T. Tooth retention through root canal treatment or tooth extraction and implant placement: A prosthodontic perspective. Quintessence Int. 2014, 45, 405–416.
- Zafiropoulos, G.K.; di Prisco, M.O.; Deli, G.; Hoffmann, O. Maintenance of class III trifurcated molars versus implant placement in regenerated extraction sockets: Long-term results of 2 cases. J. Oral Implantol. 2011, 37, 141–155.
- Martu, M.A.; Maftei, G.A.; Luchian, I.; Popa, C.; Filioreanu, A.M.; Tatarciuc, D.; Nichitean, G.; Hurjui, L.-L.; Foia, L.-G. Wound healing of periodontal and oral tissues: Part II-Patho-phisiological conditions and metabolic diseases. Rom. J. Oral Rehabil. 2020, 12, 30–40.
- Clark, D.; Levin, L. In the dental implant era, why do we still bother saving teeth? J. Endod. 2019, 45, S57–S65.
- Popa, C.G.; Luchian, I.; Ioanid, N.; Goriuc, A.; Martu, I.; Bosinceanu, D.; Martu, M.A.; Tirca, T.; Martu, S. ELISA Evaluation of RANKL Levels in Gingival Fluid in Patients with Periodontitis and Occlusal Trauma. Rev. Chim. 2018, 69, 1578–1580.
- Martinez-Canut, P. Predictors of tooth loss due to periodontal disease in patients following long-term periodontal maintenance. J. Clin. Periodontol. 2015, 42, 1115–1125.
- Lin, J.; Tu, C.; Chen, Y.; Wang, C.Y.; Liu, C.M.; Kuo, M.Y.P.; Chang, P.C. Influence of adjacent teeth absence or extraction on the outcome of non-surgical periodontal therapy. Int. J. Environ. Res. Public Health. 2019, 16, 4344.
- Ettinger, R.L. Restoring the ageing dentition: Repair or replacement? Int. Dent. J. 1990, 40, 275–282.
This entry is offline, you can click here to edit this entry!