This work shows a global vision of the situation, placing the reader in a concise and orderly manner in perspective of the current state of treatment of metastatic uveal melanoma. Uveal melanoma (UM) is the most common primary intraocular malignancy in adults. The most frequent location is the choroid, representing 80% of the total, followed by the ciliary body, 12%, and the iris, 8%. The incidence of UM ranges from 5.3 to 10.9 cases per million inhabitants per year. Risk factors for developing UM include fair skin, congenital ocular melanocytosis, melanocytoma, and BAP1-tumor predisposition syndrome.
- uveal melanoma
- metastatic
- review
1.Introduction
More than 50% of patients with uveal melanoma end up developing metastases. Currently, there is no standard first-line treatment that facilitates proper management of the metastatic disease.
Therefore, improvements in primary tumor management have not translated into longer survival in patients with UM [1][2]. The 5-year survival rate among patients with the primary disease is approximately 60–70%; however, in advanced stages, with the presence of metastatic disease, the median overall survival falls to approximately 6–10 months, with only 8% of patients surviving to 2 years [3][4]. There has been considerable development in the field of treatment of metastatic UM over the past few decades, but new treatments do not appear to have demonstrated clear benefits [5][6].
2. Conventional Chemotherapy
Most of the systemic treatments in metastatic UM have been extrapolations from experience in cutaneous melanoma. With regard to conventional chemotherapy, the most commonly used drugs have been dacarbazine, fotemustine, and temozolomide, although studies have also been conducted with more modern agents, such as docosahexaenoic acid and paclitaxel and liposomal vincristine [7]. However, unlike its cutaneous counterpart, UM tends to be characterized by chemoresistance, as shown by the average survival rates provided by this review, which range from 4.6 to 17 months [7][8][9][10][11][12][13][14][15][16][17][18][19][20][21].
In recent years, studies on temozolomide and dacarbazine with medians of OS between 5 and 13 months and progression-free interval (PFI) of up to 5.5 months have been the most consistent within this group [7][8][10][11][13][18]. The results with the combination of treosulfan and gemcitabine, on the other hand, are the most encouraging, even reaching medians of 14 months and annual survival rates of 80%, as in the Pföhler et al.’s trial [17].
Despite the large number of studies concerning conventional therapy, very few present exceptional data that deviate from the average. Among them, we found one patient alive at 5 years in the study by Leyvraz et al. [16], with fotemustine, a 57-month survival patient in the trial by Terheyden et al. [22], with gemcitabine and treosulfan, and another patient who survived 72 months in the study by Schinzari et al. [12], with a combination of cisplatin, dacarbazine, and vinblastine.
In terms of adverse effects, nausea and vomiting induced by chemotherapy represent the most frequent toxic effect, appearing in approximately 40–50% of the patients in the studies, and although they are often mild, they constitute one of the phenomena, which most deteriorate the quality of life of the oncological patient [23]. The vast majority of chemotherapy agents negatively affect the hematopoietic system [24][25], providing the most serious toxicities by affecting all cell series. Fotemustine [16] has the highest toxicity data, and dacarbazine or temozolomide [10] has the lowest (Figure 1).
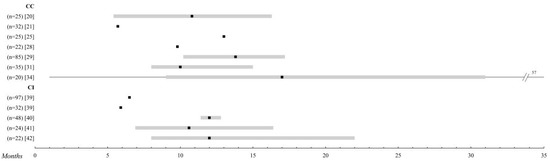
Figure 1. Systemic chemotherapy. Comparison of the overall survival of the different treatments in metastatic uveal melanoma (UM). Those studies with n > 20 patients were selected. The black square indicates the median, and the 95% confidence intervals are represented in a grey bar. The range is established by the black lines. The overall survival is shown up to 35 months; when it is extended, the maximum time data (in months) is added. Abbreviations: CC, conventional chemotherapy; CI, chemoimmunotherapy.
3. Chemoimmunotherapy
Different hypotheses maintain that the immune privilege enjoyed by the eye favors the growth and development of complex tissues, thanks to different mechanisms for the suppression of immune responses. Thus, to address the difficulty of metastatic treatment, different combinations of chemo-immune therapy have been proposed [26].
It is noteworthy that in this group [22][27][28][29][30][31][32], with the exception of the study of Pyrhönen et al. [30], all treatments are specifically studied as a first-line. The overall survival data range from 3, 7 to 12 months, although the range of PFI is much wider (1, 6–12 months). A multi-center study has analyzed the efficacy of BOLD (bleomycin, vincristine, lomustine, and dacarbazine) plus recombinant interferon α-2b, a form of TIQ, due to very promising pilot reports [33][34], but ultimately the expected results could not be confirmed. Adverse effects are practically superimposed on those of isolated chemotherapy, except for complications arising from the intra-arterial catheter used in the study by Becker et al. [28] and the liver toxicity of up to 80% found by Kivelä et al. [29] (Figure 1).
4. Immunotherapy
Immunotherapy has been shown to have a large survival benefit in the treatment of metastatic skin melanoma; however, it is unclear whether this advantage translates into UM, as it is a less immunogenic tumor [35].
For this reason, it has been precisely this immunological field on which studies in recent years have focused their attention in a very noticeable way, as can be seen in the articles included in this review [8][9][36][37][38][39][40][41][42][43][44][45][46][47][48][49][50][51][52][53][54][55][56][57][58].
Ipilimumab, a monoclonal antibody to cytotoxic T-lymphocyte antigen 4 (CTLA-4), blocks the effects of this regulator and increases T-cell responses against cancer cells, thus promoting increased immune system performance. Phase III trials have shown a clear survival benefit in metastatic skin melanoma [59]. However, in UM, survival is not increased with average values of approximately 10 months [8][38][43][50].
Anti-PD1 (anti-receptor of programmed death) therapy, such as pembrolizumab or nivolumab, is also being studied, but the results are very similar to those of ipilimumab in both OS and PFI, which is about 2–3 months long [7][41][42][45][46][49][52].
The best results of this group are obtained by combining several immunotherapies, as in Kirchberg et al. [44], (Ipilimumab + Pembrolizumab), and Pelster et al. [48], (Nivolumab + Ipilimumab), with median OS of 18.4 and 19.1 months, respectively.
In this treatment group, it is remarkable how a few exceptional events are observed in certain studies. Extreme survival can be appreciated in the four alive patients at 5 years in the study by Klemen et al. [37] or the 46 months reached by a patient in the study by Bol et al. [8] with ipilimumab.
The adverse effects are closely related to the hyperactivation of the immune system, with skin reactions and pseudo-flu symptoms being the most frequent in this group, which, in the vast majority of studies, are described as easily controllable. Among the most serious, hormonal alterations at the thyroid and pituitary levels and autoimmune colitis stand out, which, in the study by Rozeman et al. [38] with 10 mg of ipilimumab, affected 47% of the patients included (Figure 2).
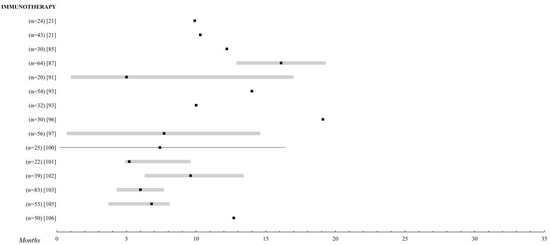
Figure 2. Immunotherapy. Comparison of the overall survival of the different treatments for metastatic UM. Those studies with n > 20 patients were selected. The black square indicates the median, the 95% confidence intervals are the grey bar. The range is established by the black lines. The overall survival is shown up to 35 months; when it is extended, the maximum time data (in months) is added.
5. Targeted Therapy
Targeted therapy refers to drugs designed to interfere with a specific molecular pathway that is believed to play a critical role in tumor development or progression [59]. UM has a distinctive genetic profile that makes it an attractive candidate for the treatment with molecular target therapy. Unlike skin melanomas, BRAF mutations are extremely rare in uveal melanomas, where the vast majority show mutations in the genes GNAQ and GNA11 [60][61] that activate the mitogen-activated protein kinase (MAPK) pathway and, consequently, result in increased cell proliferation. These include drugs that can modify the pathways that regulate the cell cycle, inhibit the molecules involved in invasion and metastasis, and inhibit tumor angiogenesis [59] (Figure 3).
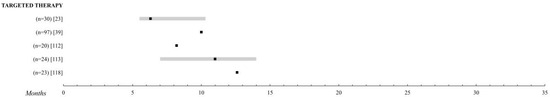
Figure 3. Targeted therapy. Comparison of the overall survival of the different treatments for metastatic UM. Those studies with n > 20 patients were selected. The black square indicates the median, the 95% confidence intervals are the grey bar. The range is established by the black lines. The overall survival is shown up to 35 months; when it is extended, the maximum time data (in months) is added.
5.1. MAPK Inhibitors
The targeted therapies explored have been sunitinib [62], sorafenib [63][64][65], imatinib [66][67], cabozatinib [10][68], and selumetenib [27] alone or in combination with chemotherapy, reaching a median OS at 6, 3–12 months. The work of Niederkorn et al. [65] with sorafenib and fotemustine was unremarkable, providing an OS of 15.9 months and a 75% survival rate at one year, but this might be of little relevance due to the small sample size of the study—25 patients.
Promising results had initially been obtained with selumetinib, a phosphorylation inhibitor of MAPKs versus chemotherapy, but the recent SUMIT study led by Carvajal et al. [27], a phase II trial intended to confirm these results, finally found no difference between dacarbazine and dacarbazine with selumetinib with a median OS of about 10 months and a PFI of 2.8.
5.2. Heat Shock Protein 90 Protein Inhibitor
Hsp90 (heat shock protein) is a 90 kDa chaperone that promotes the folding of other proteins, allowing them to acquire their native three-dimensional conformation and thus perform their biological function [119]. It interacts with several client proteins, including signaling kinases (RAF and AKT), growth factor receptors (MET and KIT), and cell cycle regulators [69][70]. Several studies have found overexpression of Hsp90 in both solid and hematological malignancies, and data from cell line-based experiments suggest that this overexpression can also be seen in UM [71].
Ganetespib (STA-9090) is a synthetic small molecule that binds to Hsp90 and inactivates it [72]. Preclinical data have shown that in both in vitro and in vivo systems, ganetespib exhibits potent cytotoxicity and anti-tumor activity. Taking this as a reference, Shah et al. [73] conducted a prospective, controlled clinical trial with 17 patients in which different dosages of the drug were evaluated. Unfortunately, the median OS did not exceed 8.5 months.
6. Liver Thermotherapy
Other local ablative treatment techniques, such as CT-guided multi-probe stereotactic radiofrequency ablation (SRFA) or percutaneous magnetic resonance imaging (MRI)-guided laser-induced interstitial thermotherapy (LITT), have also been investigated for metastatic UM. The survival results are spectacular, reaching 38 months of the median OS with SRFA [73] and 33.6 months with LITT [74], making them an attractive alternative enhanced by minimal adverse effects. However, the scarcity of studies and their small sample size make it clear that new work is needed to confirm these theories.
This entry is adapted from the peer-reviewed paper 10.3390/cancers12092557
References
- Singh, A.D.; Turell, M.E.; Topham, A.K. Uveal melanoma: Trends in incidence, treatment, and survival. Ophthalmology 2011, 118, 1881–1885.
- Abrahamsson, M. Malignant melanoma of the choroid and the ciliary body 1956-1975 in Halland and Gothenburg. Incidence, histopathology and prognosis. Acta Ophthalmol. 1983, 61, 600–610.
- Bertil Damato; Antonio Eleuteri; Azzam F.G. Taktak; Sarah E. Coupland; Estimating prognosis for survival after treatment of choroidal melanoma. Progress in Retinal and Eye Research 2011, 30, 285-295, 10.1016/j.preteyeres.2011.05.003.
- Benjamin A Krantz; Nikita Dave; Kimberly M Komatsubara; Brian P Marr; Richard D Carvajal; Uveal melanoma: epidemiology, etiology, and treatment of primary disease. Clinical Ophthalmology 2017, 11, 279-289, 10.2147/opth.s89591.
- Augsburger, J.J.; Correa, Z.M.; Shaikh, A.H. Effectiveness of treatments for metastatic uveal melanoma. Am. J. Ophthalmol. 2009, 148, 119–127.
- Buder, K.; Gesierich, A.; Gelbrich, G.; Goebeler, M. Systemic treatment of metastatic uveal melanoma: Review of literature and future perspectives. Cancer Med. 2013, 2, 674–686.
- Francesc Pons; Maria Plana; Josep Maria Caminal; Joan Pera; Isabel Fernandes; Javier Perez; Xavier Garcia-Del-Muro; Joaquim Marcoval; Rosa Penin; Àngels Fabra; et al. Metastatic uveal melanoma. Melanoma Research 2011, 21, 217-222, 10.1097/cmr.0b013e3283457726.
- Bol, K.F.; Ellebaek, E.; Hoejberg, L.; Bagger, M.M.; Larsen, M.S.; Klausen, T.W.; Kohler, U.H.; Schmidt, H.; Bastholt, L.; Kiilgaard, J.F.; et al. Real-World Impact of Immune Checkpoint Inhibitors in Metastatic Uveal Melanoma. Cancers 2019, 11, 1489.
- Xu, L.T.; Funchain, P.F.; Bena, J.F.; Li, M.; Tarhini, A.; Berber, E.; Singh, A.D. Uveal Melanoma Metastatic to the Liver: Treatment Trends and Outcomes. Ocul. Oncol. Pathol. 2019, 5, 323–332.
- Luke, J.J.; Olson, D.J.; Allred, J.B.; Strand, C.A.; Bao, R.; Zha, Y.; Carll, T.; Labadie, B.W.; Bastos, B.R.; Butler, M.O.; et al. Randomized Phase II Trial and Tumor Mutational Spectrum Analysis from Cabozantinib versus Chemotherapy in Metastatic Uveal Melanoma (Alliance A091201). Clin. Cancer Res. 2020, 26, 804–811.
- Tulokas, S.; Maenpaa, H.; Peltola, E.; Kivela, T.; Vihinen, P.; Virta, A.; Makela, S.; Kallio, R.; Hernberg, M. Selective internal radiation therapy (SIRT) as treatment for hepatic metastases of uveal melanoma: A Finnish nation-wide retrospective experience. Acta Oncol. 2018, 57, 1373–1380.
- Schinzari, G.; Rossi, E.; Cassano, A.; Dadduzio, V.; Quirino, M.; Pagliara, M.; Blasi, M.A.; Barone, C. Cisplatin, dacarbazine and vinblastine as first line chemotherapy for liver metastatic uveal melanoma in the era of immunotherapy: A single institution phase II study. Melanoma Res. 2017, 27, 591–595.
- Carling, U.; Dorenberg, E.J.; Haugvik, S.P.; Eide, N.A.; Berntzen, D.T.; Edwin, B.; Dueland, S.; Rosok, B. Transarterial Chemoembolization of Liver Metastases from Uveal Melanoma Using Irinotecan-Loaded Beads: Treatment Response and Complications. Cardiovasc. Interv. Radiol. 2015, 38, 1532–1541.
- Corrie, P.G.; Shaw, J.; Spanswick, V.J.; Sehmbi, R.; Jonson, A.; Mayer, A.; Bulusu, R.; Hartley, J.A.; Cree, I.A. Phase I trial combining gemcitabine and treosulfan in advanced cutaneous and uveal melanoma patients. Br. J. Cancer 2005, 92, 1997–2003.
- Homsi, J.; Bedikian, A.Y.; Papadopoulos, N.E.; Kim, K.B.; Hwu, W.J.; Mahoney, S.L.; Hwu, P. Phase 2 open-label study of weekly docosahexaenoic acid-paclitaxel in patients with metastatic uveal melanoma. Melanoma Res. 2010, 20, 507–510.
- Leyvraz, S.; Piperno-Neumann, S.; Suciu, S.; Baurain, J.F.; Zdzienicki, M.; Testori, A.; Marshall, E.; Scheulen, M.; Jouary, T.; Negrier, S.; et al. Hepatic intra-arterial versus intravenous fotemustine in patients with liver metastases from uveal melanoma (EORTC 18021): A multicentric randomized trial. Ann. Oncol. 2014, 25, 742–746.
- Pfohler, C.; Cree, I.A.; Ugurel, S.; Kuwert, C.; Haass, N.; Neuber, K.; Hengge, U.; Corrie, P.G.; Zutt, M.; Tilgen, W.; et al. Treosulfan and gemcitabine in metastatic uveal melanoma patients: Results of a multicenter feasibility study. Anticancer Drugs 2003, 14, 337–340.
- Piperno-Neumann, S.; Diallo, A.; Etienne-Grimaldi, M.C.; Bidard, F.C.; Rodrigues, M.; Plancher, C.; Mariani, P.; Cassoux, N.; Decaudin, D.; Asselain, B.; et al. Phase II Trial of Bevacizumab in Combination With Temozolomide as First-Line Treatment in Patients With Metastatic Uveal Melanoma. Oncologist 2016, 21, 281–282.
- Schmittel, A.; Scheulen, M.E.; Bechrakis, N.E.; Strumberg, D.; Baumgart, J.; Bornfeld, N.; Foerster, M.H.; Thiel, E.; Keilholz, U. Phase II trial of cisplatin, gemcitabine and treosulfan in patients with metastatic uveal melanoma. Melanoma Res. 2005, 15, 205–207.
- Schmittel, A.; Schuster, R.; Bechrakis, N.E.; Siehl, J.M.; Foerster, M.H.; Thiel, E.; Keilholz, U. A two-cohort phase II clinical trial of gemcitabine plus treosulfan in patients with metastatic uveal melanoma. Melanoma Res. 2005, 15, 447–451.
- Terheyden, P.; Brocker, E.B.; Becker, J.C. Clinical evaluation of in vitro chemosensitivity testing: The example of uveal melanoma. J. Cancer Res. Clin. Oncol. 2004, 130, 395–399.
- Patrick Terheyden; Eckhart Kämpgen; Thomas M. Rünger; Eva-Bettina Bröcker; Jürgen C. Becker; Immunochemotherapie des metastasierenden Uveamelanoms mit Interferon-α2b, Interleukin-2 und Fotemustin. Der Hautarzt 1998, 49, 770-773, 10.1007/s001050050823.
- P.L.R. Andrews; W.G. Rapeport; G.J. Sanger; Neuropharmacology of emesis induced by anti-cancer therapy. Trends in Pharmacological Sciences 1988, 9, 334-341, 10.1016/0165-6147(88)90106-x.
- Pedersen-Bjergaard, J.; Rowley, J.D. The balanced and the unbalanced chromosome aberrations of acute myeloid leukemia may develop in different ways and may contribute differently to malignant transformation. Blood 1994, 83, 2780–2786.
- Pedersen-Bjergaard, J.; Daugaard, G.; Hansen, S.W.; Philip, P.; Larsen, S.O.; Rorth, M. Increased risk of myelodysplasia and leukaemia after etoposide, cisplatin, and bleomycin for germ-cell tumours. Lancet 1991, 338, 359–363.
- S. A. J. Ijland; M. J. Jager; B. M. Heijdra; J. R. Westphal; R. Peek; Expression of angiogenic and immunosuppressive factors by uveal melanoma cell lines. Melanoma Research 1999, 9, 445-450, 10.1097/00008390-199910000-00003.
- Carvajal, R.D.; Piperno-Neumann, S.; Kapiteijn, E.; Chapman, P.B.; Frank, S.; Joshua, A.M.; Piulats, J.M.; Wolter, P.; Cocquyt, V.; Chmielowski, B.; et al. Selumetinib in Combination With Dacarbazine in Patients With Metastatic Uveal Melanoma: A Phase III, Multicenter, Randomized Trial (SUMIT). J. Clin. Oncol. 2018, 36, 1232–1239.
- Becker, J.C.; Terheyden, P.; Kampgen, E.; Wagner, S.; Neumann, C.; Schadendorf, D.; Steinmann, A.; Wittenberg, G.; Lieb, W.; Brocker, E.B. Treatment of disseminated ocular melanoma with sequential fotemustine, interferon alpha, and interleukin 2. Br. J. Cancer 2002, 87, 840–845.
- Kivela, T.; Suciu, S.; Hansson, J.; Kruit, W.H.; Vuoristo, M.S.; Kloke, O.; Gore, M.; Hahka-Kemppinen, M.; Parvinen, L.M.; Kumpulainen, E.; et al. Bleomycin, vincristine, lomustine and dacarbazine (BOLD) in combination with recombinant interferon alpha-2b for metastatic uveal melanoma. Eur. J. Cancer 2003, 39, 1115–1120.
- Pyrhonen, S.; Hahka-Kemppinen, M.; Muhonen, T.; Nikkanen, V.; Eskelin, S.; Summanen, P.; Tarkkanen, A.; Kivela, T. Chemoimmunotherapy with bleomycin, vincristine, lomustine, dacarbazine (BOLD), and human leukocyte interferon for metastatic uveal melanoma. Cancer 2002, 95, 2366–2372.
- Solti, M.; Berd, D.; Mastrangelo, M.J.; Sato, T. A pilot study of low-dose thalidomide and interferon alpha-2b in patients with metastatic melanoma who failed prior treatment. Melanoma Res. 2007, 17, 225–231.
- Vihinen, P.P.; Hernberg, M.; Vuoristo, M.S.; Tyynela, K.; Laukka, M.; Lundin, J.; Ivaska, J.; Pyrhonen, S. A phase II trial of bevacizumab with dacarbazine and daily low-dose interferon-alpha2a as first line treatment in metastatic melanoma. Melanoma Res. 2010, 20, 318–325.
- Nathan, F.E.; Berd, D.; Sato, T.; Shield, J.A.; Shields, C.L.; De Potter, P.; Mastrangelo, M.J. BOLD+interferon in the treatment of metastatic uveal melanoma: First report of active systemic therapy. J. Exp. Clin. Cancer Res. CR 1997, 16, 201–208.
- Pyrhonen, S. The treatment of metastatic uveal melanoma. Eur. J. Cancer 1998, 34 (Suppl. 3), S27–S30.
- Markus V. Heppt; Theresa Steeb; Justin Gabriel Schlager; Stefanie Rosumeck; C. Dressler; Thomas Ruzicka; Alexander Nast; Carola Berking; Immune checkpoint blockade for unresectable or metastatic uveal melanoma: A systematic review. Cancer Treatment Reviews 2017, 60, 44-52, 10.1016/j.ctrv.2017.08.009.
- Malinda Itchins; Paolo A Ascierto; Alexander M. Menzies; Meredith Oatley; Serigne Lo; Dariush Douraghi-Zadeh; Timmothy Harrington; Richard Maher; Antonio M. Grimaldi; Alexander Guminski; et al. A multireferral centre retrospective cohort analysis on the experience in treatment of metastatic uveal melanoma and utilization of sequential liver-directed treatment and immunotherapy. Melanoma Research 2017, 27, 243-250, 10.1097/cmr.0000000000000343.
- Klemen, N.D.; Wang, M.; Rubinstein, J.C.; Olino, K.; Clune, J.; Ariyan, S.; Cha, C.; Weiss, S.A.; Kluger, H.M.; Sznol, M. Survival after checkpoint inhibitors for metastatic acral, mucosal and uveal melanoma. J. Immunother. Cancer 2020, 8, e000341.
- Rozeman, E.A.; Prevoo, W.; Meier, M.A.J.; Sikorska, K.; Van, T.M.; van de Wiel, B.A.; van der Wal, J.E.; Mallo, H.A.; Grijpink-Ongering, L.G.; Broeks, A.; et al. Phase Ib/II trial testing combined radiofrequency ablation and ipilimumab in uveal melanoma (SECIRA-UM). Melanoma Res. 2020, 30, 252–260.
- Heppt, M.V.; Amaral, T.; Kahler, K.C.; Heinzerling, L.; Hassel, J.C.; Meissner, M.; Kreuzberg, N.; Loquai, C.; Reinhardt, L.; Utikal, J.; et al. Combined immune checkpoint blockade for metastatic uveal melanoma: A retrospective, multi-center study. J. Immunother. Cancer 2019, 7, 299.
- Karivedu, V.; Eldessouki, I.; Taftaf, A.; Zhu, Z.; Makramalla, A.; Karim, N.A. Nivolumab and Ipilimumab in the Treatment of Metastatic Uveal Melanoma: A Single-Center Experience. Case Rep. Oncol. Med. 2019, 2019, 3560640.
- Rossi, E.; Pagliara, M.M.; Orteschi, D.; Dosa, T.; Sammarco, M.G.; Caputo, C.G.; Petrone, G.; Rindi, G.; Zollino, M.; Blasi, M.A.; et al. Pembrolizumab as first-line treatment for metastatic uveal melanoma. Cancer Immunol. Immunother. CII 2019, 68, 1179–1185.
- Namikawa, K.; Takahashi, A.; Mori, T.; Tsutsumida, A.; Suzuki, S.; Motoi, N.; Jinnai, S.; Kage, Y.; Mizuta, H.; Muto, Y.; et al. Nivolumab for patients with metastatic uveal melanoma previously untreated with ipilimumab: A single-institution retrospective study. Melanoma Res. 2020, 30, 76–84.
- Arzu Yasar, H.; Turna, H.; Esin, E.; Murat Sedef, A.; Alkan, A.; Oksuzoglu, B.; Ozdemir, N.; Sendur, M.N.; Sezer, A.; Kilickap, S.; et al. Prognostic factors for survival in patients with mucosal and ocular melanoma treated with ipilimumab: Turkish Oncology Group study. J. Oncol. Pharm. Pract. 2020, 26, 267–272.
- Kirchberger, M.C.; Moreira, A.; Erdmann, M.; Schuler, G.; Heinzerling, L. Real world experience in low-dose ipilimumab in combination with PD-1 blockade in advanced melanoma patients. Oncotarget 2018, 9, 28903–28909.
- Heppt, M.V.; Heinzerling, L.; Kahler, K.C.; Forschner, A.; Kirchberger, M.C.; Loquai, C.; Meissner, M.; Meier, F.; Terheyden, P.; Schell, B.; et al. Prognostic factors and outcomes in metastatic uveal melanoma treated with programmed cell death-1 or combined PD-1/cytotoxic T-lymphocyte antigen-4 inhibition. Eur. J. Cancer 2017, 82, 56–65.
- Bender, C.; Enk, A.; Gutzmer, R.; Hassel, J.C. Anti-PD-1 antibodies in metastatic uveal melanoma: A treatment option? Cancer Med. 2017, 6, 1581–1586.
- Okada, M.; Kijima, T.; Aoe, K.; Kato, T.; Fujimoto, N.; Nakagawa, K.; Takeda, Y.; Hida, T.; Kanai, K.; Imamura, F.; et al. Clinical Efficacy and Safety of Nivolumab: Results of a Multicenter, Open-label, Single-arm, Japanese Phase II study in Malignant Pleural Mesothelioma (MERIT). Clin. Cancer Res. 2019, 25, 5485–5492.
- Pelster, M.; Gruschkus, S.K.; Bassett, R.; Gombos, D.S.; Shephard, M.; Posada, L.; Glover, M.; Diab, A.; Hwu, P.; Patel, S.P. Phase II study of ipilimumab and nivolumab (ipi/nivo) in metastatic uveal melanoma (UM).in metastatic uveal melanoma (UM). J. Clin. Oncol. 2019, 37, 9522.
- Algazi, A.P.; Tsai, K.K.; Shoushtari, A.N.; Munhoz, R.R.; Eroglu, Z.; Piulats, J.M.; Ott, P.A.; Johnson, D.B.; Hwang, J.; Daud, A.I.; et al. Clinical outcomes in metastatic uveal melanoma treated with PD-1 and PD-L1 antibodies. Cancer 2016, 122, 3344–3353.
- Danielli, R.; Ridolfi, R.; Chiarion-Sileni, V.; Queirolo, P.; Testori, A.; Plummer, R.; Boitano, M.; Calabro, L.; Rossi, C.D.; Giacomo, A.M.; et al. Ipilimumab in pretreated patients with metastatic uveal melanoma: Safety and clinical efficacy. Cancer Immunol. Immunother. CII 2012, 61, 41–48.
- Joshua, A.M.; Monzon, J.G.; Mihalcioiu, C.; Hogg, D.; Smylie, M.; Cheng, T. A phase 2 study of tremelimumab in patients with advanced uveal melanoma. Melanoma Res. 2015, 25, 342–347.
- Karydis, I.; Chan, P.Y.; Wheater, M.; Arriola, E.; Szlosarek, P.W.; Ottensmeier, C.H. Clinical activity and safety of Pembrolizumab in Ipilimumab pre-treated patients with uveal melanoma. Oncoimmunology 2016, 5, e1143997.
- Kelderman, S.; van der Kooij, M.K.; van den Eertwegh, A.J.; Soetekouw, P.M.; Jansen, R.L.; van den Brom, R.R.; Hospers, G.A.; Haanen, J.B.; Kapiteijn, E.; Blank, C.U. Ipilimumab in pretreated metastastic uveal melanoma patients. Results of the Dutch Working group on Immunotherapy of Oncology (WIN-O). Acta Oncol. 2013, 52, 1786–1788.
- Luke, J.J.; Callahan, M.K.; Postow, M.A.; Romano, E.; Ramaiya, N.; Bluth, M.; Giobbie-Hurder, A.; Lawrence, D.P.; Ibrahim, N.; Ott, P.A.; et al. Clinical activity of ipilimumab for metastatic uveal melanoma: A retrospective review of the Dana-Farber Cancer Institute, Massachusetts General Hospital, Memorial Sloan-Kettering Cancer Center, and University Hospital of Lausanne experience. Cancer 2013, 119, 3687–3695.
- Maio, M.; Danielli, R.; Chiarion-Sileni, V.; Pigozzo, J.; Parmiani, G.; Ridolfi, R.; De Rosa, F.; Del Vecchio, M.; Di Guardo, L.; Queirolo, P.; et al. Efficacy and safety of ipilimumab in patients with pre-treated, uveal melanoma. Ann. Oncol. 2013, 24, 2911–2915.
- van der Kooij, M.K.; Joosse, A.; Speetjens, F.M.; Hospers, G.A.; Bisschop, C.; de Groot, J.W.; Koornstra, R.; Blank, C.U.; Kapiteijn, E. Anti-PD1 treatment in metastatic uveal melanoma in the Netherlands. Acta Oncol. 2017, 56, 101–103.
- Zimmer, L.; Vaubel, J.; Mohr, P.; Hauschild, A.; Utikal, J.; Simon, J.; Garbe, C.; Herbst, R.; Enk, A.; Kampgen, E.; et al. Phase II DeCOG-study of ipilimumab in pretreated and treatment-naive patients with metastatic uveal melanoma. PLoS ONE 2015, 10, e0118564.
- Piulats, J.M.; Cruz-Merino, L.D.L.; Garcia, M.T.C.; Berrocal, A.; Alonso-Carrión, L.; Espinosa, E.; Castro, R.L.; Rodriguez-Abreu, D.; Fra, P.L.; Martin-Algarra, S. Phase II multicenter, single arm, open label study of nivolumab (NIVO) in combination with ipilimumab (IPI) as first line in adult patients (pts) with metastatic uveal melanoma (MUM): GEM1402 NCT02626962. J. Clin. Oncol. 2017, 35, 9533.
- F. Stephen Hodi; Steven J. O'day; David F. McDermott; Robert W. Weber; Jeffrey A. Sosman; John B. Haanen; Rene Gonzalez; Caroline Robert; Dirk Schadendorf; Jessica C. Hassel; et al. Improved Survival with Ipilimumab in Patients with Metastatic Melanoma. New England Journal of Medicine 2010, 363, 711-723, 10.1056/nejmoa1003466.
- Onken, M.D.; Worley, L.A.; Long, M.D.; Duan, S.; Council, M.L.; Bowcock, A.M.; Harbour, J.W. Oncogenic mutations in GNAQ occur early in uveal melanoma. Investig. Ophthalmol. Vis. Sci. 2008, 49, 5230–5234.
- Van Raamsdonk, C.D.; Griewank, K.G.; Crosby, M.B.; Garrido, M.C.; Vemula, S.; Wiesner, T.; Obenauf, A.C.; Wackernagel, W.; Green, G.; Bouvier, N.; et al. Mutations in GNA11 in uveal melanoma. N. Engl. J. Med. 2010, 363, 2191–2199.
- Amit Mahipal; Lukman Tijani; Kathryn Chan; Maryann Laudadio; Michael J. Mastrangelo; Takami Sato; A pilot study of sunitinib malate in patients with metastatic uveal melanoma. Melanoma Research 2012, 22, 440-446, 10.1097/cmr.0b013e328358b373.
- Bhatia, S.; Moon, J.; Margolin, K.A.; Weber, J.S.; Lao, C.D.; Othus, M.; Aparicio, A.M.; Ribas, A.; Sondak, V.K. Phase II trial of sorafenib in combination with carboplatin and paclitaxel in patients with metastatic uveal melanoma: SWOG S0512. PLoS ONE 2012, 7, e48787.
- Mouriaux, F.; Servois, V.; Parienti, J.J.; Lesimple, T.; Thyss, A.; Dutriaux, C.; Neidhart-Berard, E.M.; Penel, N.; Delcambre, C.; Peyro Saint Paul, L.; et al. Sorafenib in metastatic uveal melanoma: Efficacy, toxicity and health-related quality of life in a multicentre phase II study. Br. J. Cancer 2016, 115, 20–24.
- Niederkorn, A.; Wackernagel, W.; Artl, M.; Schwantzer, G.; Aigner, B.; Richtig, E. Response of patients with metastatic uveal melanoma to combined treatment with fotemustine and sorafenib. Acta Ophthalmol. 2014, 92, e696–e697.
- Hofmann, U.B.; Kauczok-Vetter, C.S.; Houben, R.; Becker, J.C. Overexpression of the KIT/SCF in uveal melanoma does not translate into clinical efficacy of imatinib mesylate. Clin. Cancer Res. 2009, 15, 324–329.
- Penel, N.; Delcambre, C.; Durando, X.; Clisant, S.; Hebbar, M.; Negrier, S.; Fournier, C.; Isambert, N.; Mascarelli, F.; Mouriaux, F. O-Mel-Inib: A Cancero-pole Nord-Ouest multicenter phase II trial of high-dose imatinib mesylate in metastatic uveal melanoma. Investig. New Drugs 2008, 26, 561–565.
- Adil Daud; Harriet M Kluger; Razelle Kurzrock; Frauke Schimmoller; Aaron L Weitzman; Thomas A Samuel; Ali H Moussa; Michael S Gordon; Geoffrey I Shapiro; Phase II randomised discontinuation trial of the MET/VEGF receptor inhibitor cabozantinib in metastatic melanoma. British Journal of Cancer 2017, 116, 432-440, 10.1038/bjc.2016.419.
- Stebbins, C.E.; Russo, A.A.; Schneider, C.; Rosen, N.; Hartl, F.U.; Pavletich, N.P. Crystal structure of an Hsp90-geldanamycin complex: Targeting of a protein chaperone by an antitumor agent. Cell 1997, 89, 239–250.
- Whitesell, L.; Lindquist, S.L. HSP90 and the chaperoning of cancer. Nat. Rev. Cancer 2005, 5, 761–772.
- Dana Faingold; Jean-Claude Marshall; Emilia Antecka; Sebastian Di Cesare; Alexandre N Odashiro; Silvin Bakalian; Bruno F Fernandes; Miguel N Burnier; Immune Expression and Inhibition of Heat Shock Protein 90 in Uveal Melanoma. Clinical Cancer Research 2008, 14, 847-855, 10.1158/1078-0432.ccr-07-0926.
- Shanu Modi; Komal Jhaveri; Ganetespib: research and clinical development. OncoTargets and Therapy 2015, 8, 1849-1858, 10.2147/OTT.S65804.
- Shalin Shah; Jason J. Luke; Heather A. Jacene; Tianqi Chen; Anita Giobbie-Hurder; Nageatte Ibrahim; Elizabeth Buchbinder; David F. McDermott; Keith T. Flaherty; R.J. Sullivan; et al. Results from phase II trial of HSP90 inhibitor, STA-9090 (ganetespib), in metastatic uveal melanoma. Melanoma Research 2018, 28, 605-610, 10.1097/cmr.0000000000000509.
- Katrin Eichler; S. Zangos; T. Gruber-Rouh; T.J. Vogl; M.G. Mack; MR-guided laser-induced thermotherapy (LITT) in patients with liver metastases of uveal melanoma. Journal of the European Academy of Dermatology and Venereology 2014, 28, 1756-1760, 10.1111/jdv.12405.
