1. Degradation of Adhesive Interface/Hybrid Layer
1.1. Degradation of Adhesive Resins
The main factor involved in the chronic degradation of the adhesive resins is the hydrolysis and adhesive resin leaching from the resin-dentine matrix [
62,
63]. Water diffusion into the hydrophilic adhesive initiates the leaching process, and, due to the adhesive phase separation, there is a limited degree of polymerization in the hydrophilic domains [
64]. In the aqueous environment, the poorly polymerized hydrophilic phase undergoes degradation more quickly. The primary factor involved in the reduction of the bond strength of the resin adhesive interface is the hydrolysis within the hybrid layer, which contributes to poor adhesion after some time [
64]. Water begins to penetrate the resin restoration interface after prolonged exposure of the resin restorations to oral fluids. The water acts as a plasticizer between the polymer chains of the adhesives and as a molecular lubricant. This molecular lubricant will cause mechanical wear of the exposed adhesives [
64]. This allows for greater transport of both water and enzymes, along with increasing the surface area and abrading the resin dentine interface surface, leading to the acceleration of matrix degradation [
38].
The other factor that enhances the degradation of the resin interface is chemical hydrolysis due to the water transport or salivary fluids in methacrylate materials, which results in damage to the ester bonds [
38]. An immediate increase in the bond strength was observed after the infiltration of the exposed collagen fibrils by the hydrophilic 2-hydroxyethyl methacrylate (HEMA) monomer [
63,
65]. The limitation of these adhesive systems is that they compromise the longevity of the dentine-resin bond [
66]. One of the most important factors besides the presence of water, that contributes to the degradation of adhesive resins, is the incomplete polymerization of variable degrees that can be associated to the extent of fluid movement in the adhesive hybrid layer [
5,
62,
63,
67]. Contemporary dental adhesive systems comprise both hydrophilic and hydrophobic components. Hydrophobic monomers continue to stay on the surface, whereas the hydrophilic components infiltrate the interior of the hybrid layer [
60]. These systems produce heterogeneous resin layers due to the nanophase separation ration phenomenon [
68].
One of the most significant causes involved in the degradation of the resins is the hydrophobic camphorquinone (CQ) photo-initiator [
69]. The hydrophobic CQ initiator may potentially cause a suboptimal degree of conversion of hydrophilic monomers [
69], resulting in deficient polymerization in the hybrid layer deep zone [
69]. In that instance, to improve the degree of conversion of adhesives, it is suggested to use camphorquinone in addition to water-compatible photo-initiators, such as TPO (ethyl 4-dimethylaminobenzoate and diphenyl (2,4,6-trimethylbenzoyl)-phosphine oxide) [
69]. This photo-initiator possibly reduces the damaging effect of the nanophase separation by increasing the degree of conversion of the hydrophilic and the hydrophobic components of the resin polymer [
68,
70,
71]. Other minor causes of resin interface degradation include the expansions and the contraction in resin restorative materials due to temperature changes and occlusal forces. These factors compromised the dentine resin bond stability by allowing the penetration of oral fluids and water into the resin interface [
72]. Moreover, hydrophobic and hydrophilic cytotoxic by-products, such as ethylene glycol and methacrylic acid, are released because of the breakage of ester bonds present in the HEMA [
73]. This ester bond breakage also occurs when saliva, pulp, and bacteria release esterase enzymes [
74].
1.2. Degradation of Collagen
1.2.1. Matrix Metalloproteinase (MMP)
MMPs are proenzymes common to both bone and dentine. They are Zn
2+ and Ca
2+-dependent endogenous proteases that consist of a bridge between the Zn
2+ ions and the cysteine residue [
78]. The tertiary structure of MMPs is preserved by their Ca
2+ part, whereas the Zn
2+ ions are responsible for the enzyme activation. In the intact form, these MMPs prevent the binding of the Zn
2+ ions with the water molecules, thereby preventing enzyme activation (
Figure 1) [
78]. Their classification is based on the substrate on which they act similar to collagenases (MMP-1, -8, -13, and MMP-18), gelatinases (MMP-2 and MMP-9), stromelysins (MMP-3 and MMP-10), matrilysins (MMP-7 and MMP-26), and membrane-type MMPs (MMP-14, -15, -16, and MMP-24). MMPs that are present in human dentine are MMP-2, -3, -8, -9, and MMP-20 [
79].
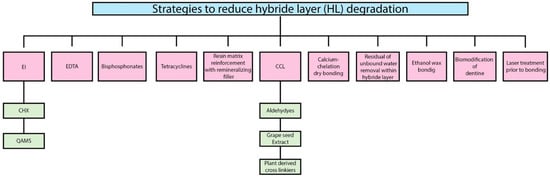
Figure 1. Summary of the strategies used to reduce hybrid layer degradation. EI → Enzymes Inhibitors; CHX → Chlorhexidine; QAMS → Quaternary ammonium methacrylate compounds; EDTA → Ethylene diamine tetra acetic acid (EDTA); CCL → Collagen Cross Linkers.
1.2.2. Cysteine Cathepsins
In dentine matrices, the prominent endogenous proteolytic enzymes that are involved in the degradation of dentine are cysteine cathepsins (CTs). The presence of CTs in dentine was reported to compromise 98% of the cathepsin activity against dentine collagen [
90,
91]. These proteases are expressed by mature human odontoblasts cells and pulpal tissues. In human dentine, there are 11 CTs that have been found involving the CT-K, CT-L, and CT-B [
92]. They can generate multiple collagen fragments due to the presence of glycosaminoglycan (GAG) side chains, as they are able to cleave helical collagen at multiple sites, whereas other CTs and MMPs can only cleave the non-helical telopeptide part of the collagen cleave [
93]. The association of cysteine cathepsins with caries progression and hybrid layer degradation was demonstrated by a few researchers [
90,
91,
94]. MMPs and cysteine cathepsins are located near the target substrate and are close to each other. Therefore, there is synergistic activity between them that was found in sound and carious dentine. In this way, the two different classes of these proteases worked as a cascade network [
90,
91,
94]. Dentine-bounded MMPs were further activated by the acidic activation of cysteine cathepsins [
95]. In addition, the spectrofluorometric use of fluorogenic substrates was carried out for these proteases (MMP and CT activities), and it was found that, in matrix degradation, two types of proteases have diverse coordinated roles. Interestingly, in dentine CT-MMP interactions, it was found and demonstrated that MMPs and CTs regulate the activities of each other [
91].
1.3. Incomplete Infiltration of the Resin Adhesives
Incomplete hybridization of the adhesive in the collagen complex in the Etch and Rinse technique is a result of the difference between penetration of the adhesive and action of the conditioning acidic agents [
96]. Nanopercolation occurs because of the incomplete hybridization of collagen networks, as they become more susceptible to hydrolytic degradation [
96]. A stable and complete hybrid layer cannot be achieved such as in the inter- and intrafibrillar compartments; the monomers are not able to replace the free and collagen-bound water [
97,
98]. In addition, large monomers such as BIS-GMA were entrapped in inter-fibrillary spaces due to highly hydrated proteoglycan hydrogels. These proteoglycan hydrogels only allow small monomers such as HEMA to penetrate toward the base of the hybrid layer [
99]. As HEMA creates weak linear chains, they will cause cyclic fatigue failure of the collagen chains when subjected to stress [
100].
2. Strategies to Reduce Hybrid Layer (HL) Degradation
2.1. Enzymes Inhibitors
2.1.1. Chlorhexidine (CHX)
Chlorhexidine is the most extensively investigated enzymatic inhibitor and an antimicrobial agent and is characterized by the excellent inhibition of MMP activity in both dentine and resin [
104]. Due to chelating properties at low concentrations (0.2%), it showed excellent inhibition of protease enzymes [
104,
105,
106,
107,
108,
109]. The literature regarding the mechanism of action of CHX is scarce, but it might be because of the cationic behavior of CHX, as it binds to both mineralized and unmineralized dentine [
105,
106,
107,
108]. As CHX consists of chlorine, it prevents its hydrolytic activity by binding to the zinc of the catalytic domain of MMPs [
104]. When CHX digluconate (0.5 wt.%, 2.0 wt.% and 4.0 wt.%) was incorporated in experimental etch-and-rinse adhesives, no adverse effects on the degree of conversion were found [
110]. However, Cadenaro et al. [
111] demonstrated that, although the degree of conversion was not affected by the incorporation of 1% or 5% CHX into the adhesive resins, the elastic modulus was significantly decreased. Furthermore, bond strength was preserved for 12 months without affecting the ultimate tensile strength, solubility, DC, and water sorption after the incorporation of CHX in Etch and Rinse adhesives [
112]. Da Silva et al. [
113] incorporated Galardin, Batimastat, GM1489, and CHX as enzyme inhibitors in Etch and Rinse adhesives and found similar results in CHX and GM1489.
2.1.2. Quaternary Ammonium Methacrylates Compounds (QAMS)
The mechanism of action of quaternary ammonium compounds is similar to CHX, as both are positively charged. The most prominent and already tested MMP inhibitor in the quaternary ammonium compounds is benzalkonium chloride (BAC). BAC consists of various alkyl chains and is a combination of alkylbenzyl-dimethylammonium chlorides. These compounds showed favorable bond strength results over time in comparison to CHX, as they strongly bind to demineralized dentine [
114,
115,
116]. To evaluate the mechanical properties of the unfilled resins after incorporating quaternary ammonium methacrylates, Hoshika et al. [
117] found that the degree of conversion of these resins was improved, but wet toughness and ultimate tensile strength were decreased by the addition of 10% QAMs, whereas when 15% QAMs were added, it decreased the mechanical properties of the resins significantly [
117]. Therefore, it was documented that, although the degree of cure will be increased, the ultimate tensile strength and Young’s modulus were decreased in QAM containing adhesive [
117]. 12-meth-acryloyl-oxydodecyl-pyridinium bromide (MDPB) is a quaternary ammonium methacrylate QAM and has been incorporated into several contemporary adhesive systems. It is well-known for its antimicrobial properties in the adhesive resins, MDBP polymerize with methacrylate; therefore, leaching of this compound was restricted and can serve as a microbe [
118]. It has an excellent capability of preventing MMP activity [
118,
119,
120,
121]. Further research is needed to demonstrate that adhesives based on QAM compounds increase the strength of the resin-dentine interface by effectively inhibiting MMPs at the resin dentine interface and also to focus on the development of quaternary ammonium functionalities [
122].
2.2. Ethylene Diamine Tetra Acetic Acid (EDTA)
For decades, due to the chelating properties, ethylene-diamine tetra acetic acid (EDTA) has been used in endodontics. EDTA binds to Zn2+ ions from the catalytic site of the MMPs and removes the Ca2+ from the collagen matrices [123,124]. However, a long application time and the reversibility caused by water solubility are the main drawbacks [125].
2.3. Bisphosphonates
Bisphosphonates are proteases inhibitors that act by chelating zinc and calcium ions from several enzymes [
126]. In particular, good instant outcomes were observed with polyvinylphosphonic acid (PVPA), but with uncertain durability [
127]. Tezvergil-Mulutuay et al. [
127] used polyvinylphosphonic acid (PVPA) on recombinant MMP-9 and found that it efficiently inhibited this gene with less hydroxyproline release. The bonding between PVPA and collagen is electrostatics. PVPA can become trapped in collagen through 1-ethyl-3-(3-dimethyl aminopropyl) carbodiimide (EDC) [
128]. This phenomenon makes PVPA more advantageous in terms of bond durability when compared with CHX. All these outcomes suggested that, to enhance the durability and longevity of resin dentine bonds, PVPA can be incorporated. However, there is a dearth of literature about bisphosphonates as MMP inhibitors; thus, future work should be performed.
2.4. Tetracycline
Tetracyclines along with their analogues doxycycline and minocycline are broad-spectrum antibiotics used as effective MMP inhibitors, having cationic chelating properties. [
129,
130]. Doxycycline decreases dentine matrix degradation intensely [
131]. Chemically-modified tetracyclines (CMT-3, Metastat) are exceptionally efficient in reducing MMPs in dentine caries and can retain their MMP-inhibiting capacity, although the antimicrobial activity is not ideal [
132]. They act on enzymes by inhibiting their activity and secretions. In addition, they are also involved in calcium chelation [
133]. However, improvements in the dentine-resin bond by the tetracycline have not yet been evaluated. These compounds need further investigation due to their potent MMP inhibiting potential. Though, during photo-oxidation, these compounds can induce the purple stain of teeth and are therefore not considered suitable for clinical use.
2.5. Collagen Cross Linkers
In dentine, collagen matrix cross-linking is not only a natural mechanism used to increase the mechanical properties of dentine, but it also is used to make dentine less susceptible to enzymatic and hydrolytic degradation [
134,
135]. Several studies, therefore, have reported the incorporation of numerous chemical constituents that have cross-linking properties in dental adhesives [
134,
135]. Cross-linking agents stabilize the collagen structure and make it more resilient to enzymatic degradation by attaching to the amino-carbonyl groups of the collagen [
134,
135]. These cross-linkers prevent the hybrid layer degradation through several mechanisms, as mentioned below:
These mechanisms could be evading the cysteine switch oxidation, which in the substrate cleavage sites will be hidden by these cross-linkers, and the dysregulation of endogenous protease expression, within collagen protection of cleavage sites, by cross-linkers and the inactivation/silencing of proteases activity [
136].
2.6. Residual or Unbound Water Removal within the Hybrid Layer
One of the greatest challenges of highly cross-linked resin polymers is that they undergo phase changes due to their poor solubility in water [
64]. Therefore, manufacturers prepare commercial adhesive systems in a variety of solvents such as ethanol to warrant the single phase of resin adhesives during clinical application. When adhesives containing solvent are applied on moist acid-etched dentine, microscopic phase changes are observed in the adhesives. Pashley et al. [
167] demonstrated the solution to this problem by replacing the water rinse with ethanol in the wet-bonding technique, which resulted in dentine saturation by ethanol, not with water. Similarly, Tay et al. [
168] reported that, when bis-GMA was applied to ethanol-saturated dentine, excellent resin–dentine bonding was achieved. The danger of phase separation can be avoided completely by using ethanol containing adhesives to dentine treated with ethanol by reducing the residual water at the dentine-resin interface [
169]. Due to water absence in the hybrid layer, the collagen matrix may not be cleaved by matrix proteases. However, in the water-wet bonding approach, hydrophobic infiltration of resin adhesives is much less than in ethanol wet-bonding [
20,
170]. It is well documented that demineralized dentine and ethanol can replace and remove unbound water [
171]. Jee et al. [
98] determined in their study whether bound water can be replaced by collagen matrices and found that the tightly bound first layer and the second layer of water cannot be replaced by ethanol in collagen, although most of the bound water in the outermost layer was substituted by ethanol.
2.7. Calcium-Chelation Dry Bonding
The acid etchant (37% phosphoric acid) used during the adhesive process completely demineralized the collagen fibrils because of its molecular weight, which is around 100 Da, which can easily pervade throughout collagen fibrils [
172,
173]. Molecules with a molecular weight smaller than 600 Da can enter collagen fibrils easily, and all molecules with a molecular weight larger than 40 KDa cannot permeate into collagen fibrils easily [
169,
170]. Keeping this point in mind, studies have used calcium chelator (sodium polyacrylate) instead of phosphoric acid [
172,
173]. They used 15 wt.% calcium chelators with a molecular weight of about 225,000 Da, which is large enough to permeate collagen. After 30 s of chelation, water rinsing and air-drying were carried out, due to which the reaction was stopped. This will lead to the preservation of inter-fibrillar gaps for monomer diffusion inward and those absorbed into the hybrid layer, and only apatite mineral was removed from the extrafibrillar space [
174]. In this approach, collagen fibrils remained too stiff to shrink or collapse even after the removal of residual water, as the collagen fibrils remained completely mineralized [
174].
2.8. Biomodification of Dentine
To enhance the physical and mechanical properties of dental hard tissue, advancements in biomodification have been made by modifying the biochemistry of these dental hard tissues by incorporating or inducing physical agents [
134]. One of the most significant physical agents used as biomodification is photo-oxidative techniques [
134]. This technique utilized ultraviolet light, which requires the most reactive and unstable type of oxygen singlet for activation. This type of oxygen singlet can be provided by vitamin B2 (riboflavin). Cross-linking occurs between the proline and hydroxyproline of side chains (carbonyl groups) and the glycine of a collagen chain (amino group). These oxygen singlets form covalent bonds when activated by ultraviolet light [
134].
2.9. Ethanol Wet Bonding
The prime factor involved in the adhesive bond strength durability is the hydrolytic degradation of adhesives. Hydrophilic and ionic monomers have been added to these adhesives to ensure the proper hybridization of wet collagen matrix [
8,
175,
176]. Mechanical properties of these hydrophilic adhesives were found to be compromised, as these polymers contain ester linkages and they are susceptible to water sorption and/or hydrolysis [
8,
175,
176]. A 12-month in vivo study conducted by Brackett et al. [
177] concluded that, despite preserving the adhesives with CHX, water-related loss of nano-fillers was observed. In a few studies, loss of bond strength was found despite containing CHX and other enzyme inhibitors [
8,
175,
176]. This loss of strength in adhesive resins might be due to polymerized hydrophilic adhesives, water sorption, or adhesive monomer degradation. These studies concluded that if water is eliminated from the bonded interface, then water hydrolysis of peptide bonds in collagen and ester-bonds in adhesive polymers might possibly be reduced. This has been the main objective of introducing the concept of ethanol-wet bonding [
177]. The phenomenon behind this concept is that acid-etched demineralized dentine matrices that were dehydrated by the ethanol aided the penetration of higher hydrophobic monomers into the interfacial dentine and reduced the collagen hydrophilicity [
177]. Ethanol-wet bonding wheedles the infiltration of hydrophobic monomers to demineralize collagen with restricted matrix shrinkage [
167]. Water sorption/solubility and resin plasticization decrease because of the infiltration of hydrophobic monomers. In addition, it has been suggested that improved durability of the resin bond occurs, resulting in decreased enzyme-catalyzed hydrolytic collagen degradation because of the elimination of residual water [
35,
178], and the hybrid layer generated with ethanol-wet bonding also resulted in outstanding durability of resin bond strength and an almost complete absence of nano-leakage [
179].
2.10. Resin Matrix Reinforcement with Remineralizing Fillers
As in the previous section, it was discussed that not only enzymatic degradation will degrade the hybrid layer, but chemical degradation also played a significant role in the degradation of adhesive durability. Fillers and nanoparticles are included in the top priority list to use as reinforcing adhesives materials [
180]. Several studies have demonstrated an increased bond strength and enhanced mechanical and physical properties of the adhesives after the incorporation of copper [
180], carboxylic acid-functionalized titanium dioxide [
181], silver micro-fillers [
182], and zinc oxide [
183] nanoparticles. To improve the bond strength of the commercial three-step etch-and-rinse adhesive system (Scotchbond™ 3M ESPE, St Paul, MN, USA), Zirconia nanoparticles were incorporated by Lohbauer et al. [
184] into the primer or adhesive. The incorporation of these particles resulted in improved resistance to the hydrolytic process, which might increase the durability of the dentine-resin bond. The rate of the bond degradation will reduce when hydrolysis is diminished due to the reduced water uptake that retarded the proteases activity, leading to the formation of a stronger hybrid layer [
161]. Nanotubes are a hexagonal network of carbon atoms that are extremely strong and stiff and have excellent thermal and electrical properties, and they were also incorporated as fillers to resin-based restorative materials to reinforce the resin matrix [
185] and thus the resin-dentine bond strength [
186,
187]. The incorporation up to 20 wt.% of nanotubes in the etch-and-rinse adhesive system and up to 10 wt.% in Self Etch adhesives system have resulted in increased bond strength [
183]. The most fascinating quality of nanotubes is the possibility of expanding the cylindrical hollow structure as a medium for the encapsulation of therapeutic molecules as well as protease inhibitors [
188]. Feitosa et al. [
188] reported that an inhibitor of MMPs (doxycycline) was encapsulated into nanotubes and then incorporated into an adhesive resin, and it was able to inhibit MMP-1 activity without compromising bond strength results. Similarly, nanotubes can be used as a vehicle for the encapsulation of biomimetic agents to prevent bond degradation due to the release of MMP inhibitors, antioxidants, and collagen crosslinkers [
188]. Although dental adhesive reinforcement with nanoparticles is an excellent strategy, the beneficial effects due to nanoparticle incorporation are very vulnerable due to agglomeration or the inhomogeneous dispersion of nanofillers in the resin phase, which may reduce the bond strength and physical stability of the adhesive materials [
188]. Usually, there is a threshold for filler loading into adhesives, and it depends on the composition of the adhesives and filler type [
189].
2.11. Laser Treatment Prior to Bonding
For bond strength enhancement, laser irradiation of enamel/dentine has been utilized [
190,
191]. Erbium-doped Yttrium Aluminum Garnet (Er,YAG) [
190,
191] and plasma-based lasers [
192,
193] are the two key sources of lasers that are employed in dentistry. The key factors that contribute to the success of dental bonding are the smear layer removal, organic content, and water evaporation, and an increased surface area was obtained by Er,YAG laser irradiation [
191]. Preceding bonding when dentine is treated with non-thermal atmospheric pressure plasma (NTAPP) laser, it was found that it aided with improved immediate bond strength as well as long-term bond stability after ageing [
192]. This might be because carboxyl and carbonyl groups are grafted by the laser application onto the dentinal substrate, which will enhance the chemical and mechanical interaction of the resin monomers. Moreover, positive effects were found when oxidizing agents were used on the dentine before laser application [
190], and the authors found a greater resin-dentine bond strength when the Er,YAG laser application on dentine was performed after bleaching. It was demonstrated that increased releases of free radicals were found after the laser during bleaching and made the surface of dentine such that it received adhesives monomers in a better tactic. This will increase the durability of the dentine and resin bond strength. Correspondingly, an efficient method to enhance the resin dentine bond strength is utilizing a non-thermal argon plasma laser for 30 s on sodium hypochlorite-treated dentine [
193]. This increase in strength might be due to increased hydrogen bonding interaction between collagen fibrils and adhesive resins after the dentine etching [
193].
6. Biomimetic Remineralization
In recent decades, biomimetic has developed as a multi-disciplinary approach in dentistry. There are several biomimetic approaches utilized in the field of restorative dentistry; an example is a tooth that was restored using bioinspired peptides, bioactive biomaterials, and biomimetic tissue regeneration to achieve remineralization [
194]. To improve the strength properties of adhesive materials, developments in the contemporary adhesive materials and understanding at the nanoscale of biomaterial–tissue interaction are continuously investigated and evaluated [
194]. The most ideal, novel, and exciting approach to prevent the collagen fibrils from degradation is biomimetic remineralization. Biomimetic remineralization involves the leaching of ion-releasing materials that simulate the natural remineralization process [
195,
196]. This process removes the residual water from water-rich regions and intrafibrillar spaces of the hybrid layer by inactivating proteases and reducing collagen degradation. These phenomena increase and restore the strength of the hybrid layer by replacing fibrils with apatite crystallites as well as preserve the durability of the resin-dentine bond interface by preventing the exposed collagen from external challenges [
195,
196]. There are two types of biomimetic remineralization that occur in adhesive dentistry:
- (a)
-
The first approach cannot occur in demineralized dentine where apatite crystals are absent. In this type of remineralization, the remaining mineral crystals act as templates for the regrowth of apatite crystals [
197].
- (b)
-
The second type of biomimetic remineralization involves incorporating polyanions (polyacrylic acid/polyaspartic acid) and apatite nucleation, resulting in biomimetic remineralization [
197].
The carious lesions may lead to the exposure of the collagen fibrils due to the loss of minerals from the dentine. This will lead to the degradation of the collagen fibrils and the deterioration of the mechanical properties of the dentine [
196]. Moreover, during restorative and adhesive procedures, various type of techniques and agents are used, such as acid etching, acidic monomers, and chelating agents, that cause the demineralization of dentine and enamel. In addition, partial infiltration of collagen fibrils with resin monomers will cause the micro-permeability and nano-leakage of hybrid layers, especially in the contemporary adhesive system [
197]. In addition these systems are not able to remove collagen fibrils, further compromising the properties of the polymeric adhesive system. Due to the incomplete or partial infiltration of resin monomers, these hybrid layers consist of numerous water-filled regions [
197]. Insoluble collagen fibrils are slowly solubilized by these that are water-filled. Remineralizing reagents such as nanometer-sized apatite crystallites can be incorporated into these water-filled voids. Polyanions act as templates for specific calcium-binding to promote the nucleation of appetites [
197]. Moreover, intrafibrillar and interfibrillar remineralization of dentin collagen fibrils were very well demonstrated after the application of non-collagenous protein (NCP) analogues [
197].
This entry is adapted from the peer-reviewed paper 10.3390/coatings12081094