Iron deficiency is a significant comorbidity of heart failure (HF), defined as the inability of the myocardium to provide sufficient blood flow. However, iron deficiency remains insufficiently detected. Iron-deficiency anemia, defined as a decrease in hemoglobin caused by iron deficiency, is a late consequence of iron deficiency, and the symptoms of iron deficiency, which are not specific, are often confused with those of HF or comorbidities. HF patients with iron deficiency are often rehospitalized and present reduced survival. The correction of iron deficiency in HF patients is associated with improved functional capacity, quality of life, and rehospitalization rates. Because of the inflammation associated with chronic HF, which complicates the picture of nutritional deficiency, only the parenteral route can bypass the tissue sequestration of iron and the inhibition of intestinal iron absorption. Given the negative impact of iron deficiency on HF progression, the frequency and financial implications of rehospitalizations due to decompensation episodes, and the efficacy of this supplementation, screening for this frequent comorbidity should be part of routine testing in all HF patients.
- iron deficiency
- heart failure
- transferrin saturation coefficient
- serum ferritin
- ferric carboxymaltose
1. Introduction
2. Iron Deficiency, the Most Common Comorbidity of Heart Failure
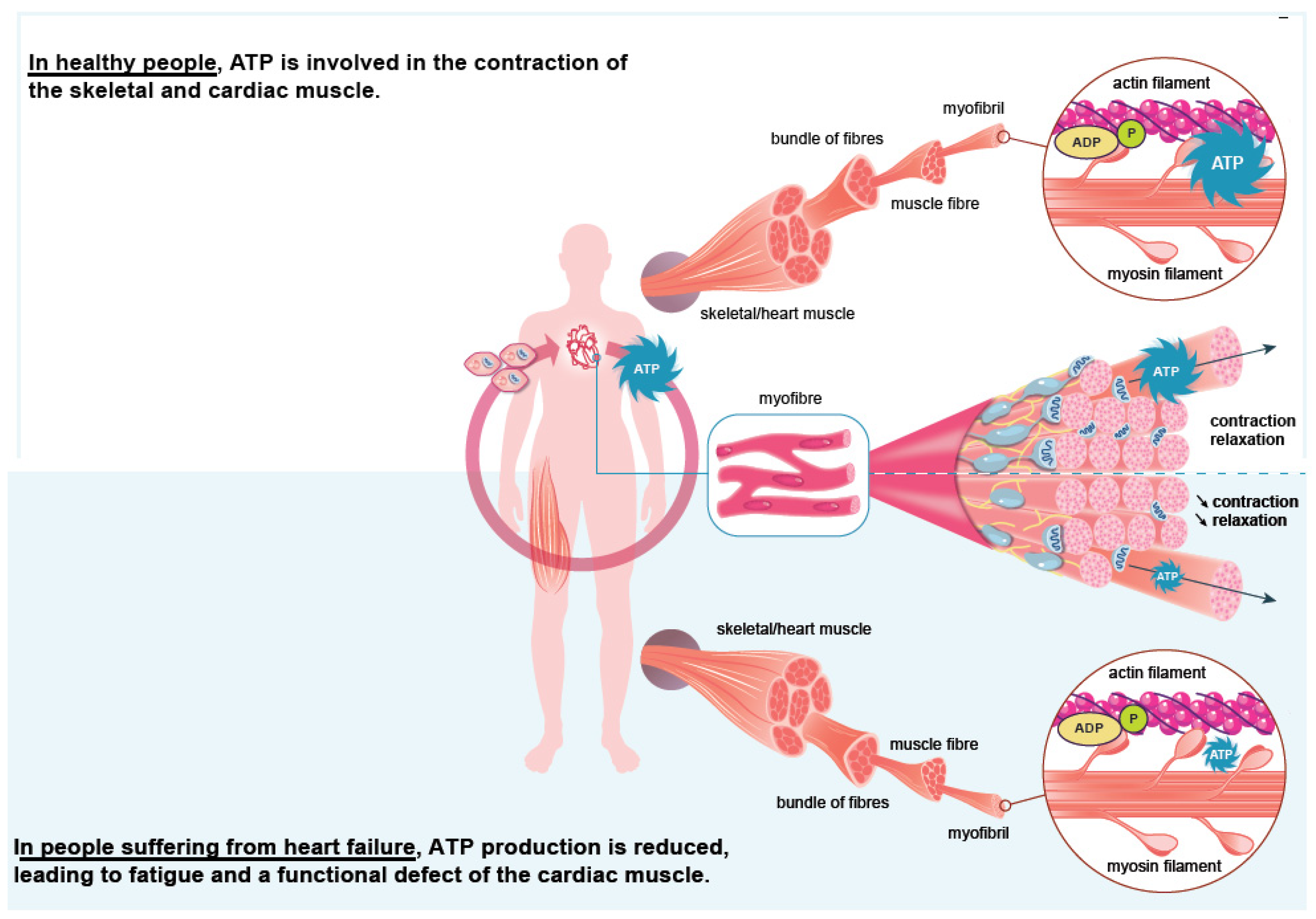
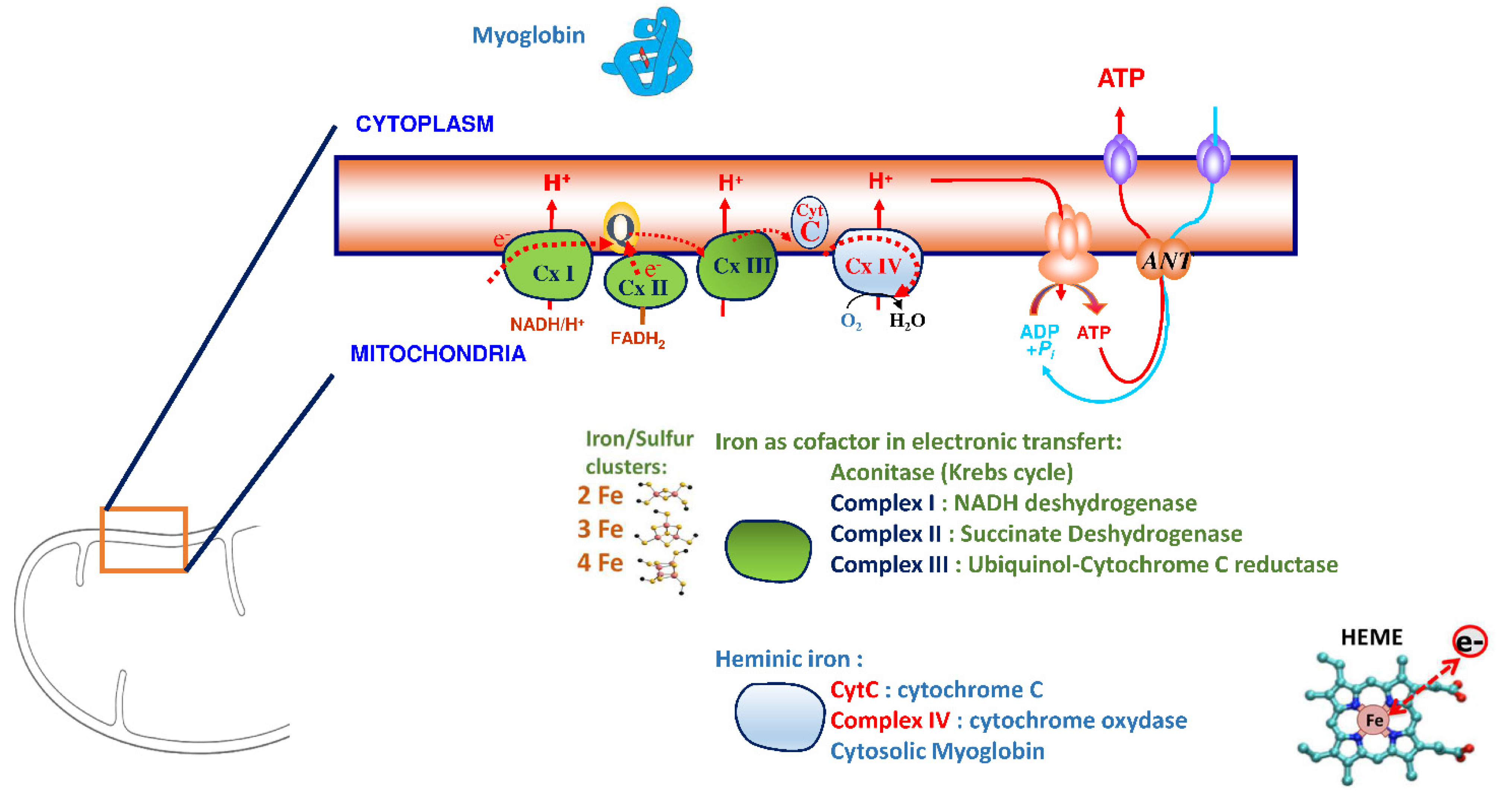
3. Iron Is an Essential Element for the Correct Functioning of the Heart Muscle
4. Iron Supplementation in Heart Failure
This entry is adapted from the peer-reviewed paper 10.3390/nu14153214
References
- Gibelin, P. Insuffisance Cardiaque: Aspects Épidémiologiques, Cliniques et Pronostiques. EMC Cardiol. 2018, 13, 11-024-A-10.
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.F.; Kozhuharov, N.; Coats, A.J.S.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology Practical Guidance on the Use of Natriuretic Peptide Concentrations. Eur. J. Heart Fail. 2019, 21, 715–731.
- Shiba, N.; Shimokawa, H. Chronic Kidney Disease and Heart Failure--Bidirectional Close Link and Common Therapeutic Goal. J. Cardiol. 2011, 57, 8–17.
- Komajda, M. Diabète et Insuffisance Cardiaque: Données Épidémiologiques et Implications Thérapeutiques. Bull Acad. Natl. Med. 2018, 202, 909–916.
- Rutten, F.H.; Cramer, M.J.; Grobbee, D.E.; Sachs, A.P.; Kirkels, J.H.; Lammers, J.W.; Hoes, A.W. Unrecognized Heart Failure in Elderly Patients with Stable Chronic Obstructive Pulmonary Disease. Eur. Heart J. 2005, 26, 1887–1894.
- Anand, I.S.; Gupta, P. Anemia and Iron Deficiency in Heart Failure: Current Concepts and Emerging Therapies. Circulation 2018, 138, 80–98.
- Chopra, V.K.; Anker, S.D. Anaemia, Iron Deficiency and Heart Failure in 2020: Facts and Numbers. ESC Heart Fail. 2020, 7, 2007–2011.
- Haute Autorité de Santé. Guide Du Parcours de Soins. Insuffisance Cardiaque. Available online: https://www.has-sante.fr/jcms/c_1242988/fr/guide-parcours-de-soins-insuffisance-cardiaque (accessed on 24 July 2014).
- Cappellini, M.D.; Comin-Colet, J.; de Francisco, A.; Dignass, A.; Doehner, W.; Lam, C.S.; Macdougall, I.C.; Rogler, G.; Camaschella, C.; Kadir, R.; et al. Iron Deficiency across Chronic Inflammatory Conditions: International Expert Opinion on Definition, Diagnosis, and Management. Am. J. Hematol. 2017, 92, 1068–1078.
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron Deficiency Anaemia. Lancet 2016, 387, 907–916.
- Peyrin-Biroulet, L.; Williet, N.; Cacoub, P. Guidelines on the Diagnosis and Treatment of Iron Deficiency across Indications: A Systematic Review. Am. J. Clin. Nutr. 2015, 102, 1585–1594.
- Klip, I.T.; Comin-Colet, J.; Voors, A.A.; Ponikowski, P.; Enjuanes, C.; Banasiak, W.; Lok, D.J.; Rosentryt, P.; Torrens, A.; Polonski, L.; et al. Iron Deficiency in Chronic Heart Failure: An International Pooled Analysis. Am. Heart J. 2013, 165, 575–582.e3.
- Cohen, L.A.; Gutierrez, L.; Weiss, A.; Leichtmann-Bardoogo, Y.; Zhang, D.; Crooks, D.R.; Sougrat, R.; Morgenstern, A.; Galy, B.; Hentze, M.W.; et al. Serum Ferritin Is Derived Primarily from Macrophages through a Nonclassical Secretory Pathway. Blood 2010, 116, 1574–1584.
- Nikolaou, M.; Chrysohoou, C.; Georgilas, T.A.; Giamouzis, G.; Giannakoulas, G.; Karavidas, A.; Papadopoulos, C.; Patsilinakos, S.; Tziakas, D.; Parissis, J. Management of Iron Deficiency in Chronic Heart Failure: Practical Considerations for Clinical Use and Future Directions. Eur. J. Intern. Med. 2019, 65, 17–25.
- Martens, P.; Dupont, M.; Dauw, J.; Nijst, P.; Herbots, L.; Dendale, P.; Vandervoort, P.; Bruckers, L.; Tang, W.H.W.; Mullens, W. The Effect of Intravenous Ferric Carboxymaltose on Cardiac Reverse Remodelling Following Cardiac Resynchronization Therapy-the IRON-CRT Trial. Eur. Heart J. 2021, 42, 4905–4914.
- Jankowska, E.A.; Rozentryt, P.; Witkowska, A.; Nowak, J.; Hartmann, O.; Ponikowska, B.; Borodulin-Nadzieja, L.; Banasiak, W.; Polonski, L.; Filippatos, G.; et al. Iron Deficiency: An Ominous Sign in Patients with Systolic Chronic Heart Failure. Eur. Heart J. 2010, 31, 1872–1880.
- Okonko, D.O.; Mandal, A.K.; Missouris, C.G.; Poole-Wilson, P.A. Disordered Iron Homeostasis in Chronic Heart Failure: Prevalence, Predictors, and Relation to Anemia, Exercise Capacity, and Survival. J. Am. Coll Cardiol. 2011, 58, 1241–1251.
- Cairo, G.; Bernuzzi, F.; Recalcati, S. A Precious Metal: Iron, an Essential Nutrient for All Cells. Genes Nutr. 2006, 1, 25–39.
- Loncar, G.; Obradovic, D.; Thiele, H.; Haehling, S.; Lainscak, M. Iron Deficiency in Heart Failure. ESC Heart Fail. 2021, 8, 2368–2379.
- Brown, D.A.; Perry, J.B.; Allen, M.E.; Sabbah, H.N.; Stauffer, B.L.; Shaikh, S.R.; Cleland, J.G.; Colucci, W.S.; Butler, J.; Voors, A.A.; et al. Expert Consensus Document: Mitochondrial Function as a Therapeutic Target in Heart Failure. Nat. Rev. Cardiol. 2017, 14, 238–250.
- Xu, W.; Barrientos, T.; Mao, L.; Rockman, H.A.; Sauve, A.A.; Andrews, N.C. Lethal Cardiomyopathy in Mice Lacking Transferrin Receptor in the Heart. Cell Rep. 2015, 13, 533–545.
- Hoes, M.F.; Grote Beverborg, N.; Kijlstra, J.D.; Kuipers, J.; Swinkels, D.W.; Giepmans, B.N.G.; Rodenburg, R.J.; van Veldhuisen, D.J.; de Boer, R.A.; van der Meer, P. Iron Deficiency Impairs Contractility of Human Cardiomyocytes through Decreased Mitochondrial Function. Eur. J. Heart Fail. 2018, 20, 910–919.
- Rineau, E.; Gaillard, T.; Gueguen, N.; Procaccio, V.; Henrion, D.; Prunier, F.; Lasocki, S. Iron Deficiency without Anemia Is Responsible for Decreased Left Ventricular Function and Reduced Mitochondrial Complex I Activity in a Mouse Model. Int. J. Cardiol. 2018, 266, 206–212.
- Lacour, P.; Dang, P.L.; Morris, D.A.; Parwani, A.S.; Doehner, W.; Schuessler, F.; Hohendanner, F.; Heinzel, F.R.; Stroux, A.; Tschoepe, C.; et al. The Effect of Iron Deficiency on Cardiac Resynchronization Therapy: Results from the RIDE-CRT Study. ESC Heart Fail. 2020, 7, 1072–1084.
- Martens, P.; Nijst, P.; Verbrugge, F.H.; Smeets, K.; Dupont, M.; Mullens, W. Impact of Iron Deficiency on Exercise Capacity and Outcome in Heart Failure with Reduced, Mid-Range and Preserved Ejection Fraction. Acta Cardiol. 2018, 73, 115–123.
- van Veldhuisen, D.J.; Anker, S.D.; Ponikowski, P.; Macdougall, I.C. Anemia and Iron Deficiency in Heart Failure: Mechanisms and Therapeutic Approaches. Nat. Rev. Cardiol. 2011, 8, 485–493.
- Tolkien, Z.; Stecher, L.; Mander, A.P.; Pereira, D.I.A.; Powell, J.J. Ferrous Sulfate Supplementation Causes Significant Gastrointestinal Side-Effects in Adults: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0117383.
- DeLoughery, T.G. Safety of Oral and Intravenous Iron. Acta Haematol. 2019, 142, 8–12.
- Auerbach, M.; Rodgers, G.M. Intravenous Iron. N. Engl. J. Med. 2007, 357, 93–94.
- Avni, T.; Bieber, A.; Grossman, A.; Green, H.; Leibovici, L.; Gafter-Gvili, A. The Safety of Intravenous Iron Preparations. Mayo Clin. Proc. 2015, 90, 12–23.
- Lewis, G.D.; Malhotra, R.; Hernandez, A.F.; McNulty, S.E.; Smith, A.; Felker, G.M.; Tang, W.H.W.; LaRue, S.J.; Redfield, M.M.; Semigran, M.J.; et al. Effect of Oral Iron Repletion on Exercise Capacity in Patients With Heart Failure With Reduced Ejection Fraction and Iron Deficiency: The IRONOUT HF Randomized Clinical Trial. JAMA 2017, 317, 1958–1966.
- Anker, S.D.; Comin Colet, J.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Luscher, T.F.; Bart, B.; Banasiak, W.; Niegowska, J.; et al. Ferric Carboxymaltose in Patients with Heart Failure and Iron Deficiency. N. Engl. J. Med. 2009, 361, 2436–2448.
- Ponikowski, P.; van Veldhuisen, D.J.; Comin-Colet, J.; Ertl, G.; Komajda, M.; Mareev, V.; McDonagh, T.; Parkhomenko, A.; Tavazzi, L.; Levesque, V.; et al. Beneficial Effects of Long-Term Intravenous Iron Therapy with Ferric Carboxymaltose in Patients with Symptomatic Heart Failure and Iron Deficiency. Eur. Heart J. 2015, 36, 657–668.
- Okonko, D.O.; Grzeslo, A.; Witkowski, T.; Mandal, A.K.; Slater, R.M.; Roughton, M.; Foldes, G.; Thum, T.; Majda, J.; Banasiak, W.; et al. Effect of Intravenous Iron Sucrose on Exercise Tolerance in Anemic and Nonanemic Patients with Symptomatic Chronic Heart Failure and Iron Deficiency FERRIC-HF: A Randomized, Controlled, Observer-Blinded Trial. J. Am. Coll Cardiol. 2008, 51, 103–112.
- van Veldhuisen, D.J.; Ponikowski, P.; van der Meer, P.; Metra, M.; Bohm, M.; Doletsky, A.; Voors, A.A.; Macdougall, I.C.; Anker, S.D.; Roubert, B.; et al. Effect of Ferric Carboxymaltose on Exercise Capacity in Patients With Chronic Heart Failure and Iron Deficiency. Circulation 2017, 136, 1374–1383.
- Anker, S.D.; Kirwan, B.A.; van Veldhuisen, D.J.; Filippatos, G.; Comin-Colet, J.; Ruschitzka, F.; Luscher, T.F.; Arutyunov, G.P.; Motro, M.; Mori, C.; et al. Effects of Ferric Carboxymaltose on Hospitalisations and Mortality Rates in Iron-Deficient Heart Failure Patients: An Individual Patient Data Meta-Analysis. Eur. J. Heart Fail. 2018, 20, 125–133.
- Anker, S.D.; Colet, J.C.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Luscher, T.F.; Mori, C.; von Eisenhart Rothe, B.; Pocock, S.; et al. Rationale and Design of Ferinject Assessment in Patients with IRon Deficiency and Chronic Heart Failure (FAIR-HF) Study: A Randomized, Placebo-Controlled Study of Intravenous Iron Supplementation in Patients with and without Anaemia. Eur. J. Heart Fail. 2009, 11, 1084–1091.
- Arutyunov, G.; Bylova, N.; Ivleva, A.; Kobalava, Z. The Safety of Intravenous (IV) Ferric Carboxymaltose versus IV Iron Sucrose on Patients with Chronic Heart Failure (CHF) and Chronic Kidney Disease (CKD) with Iron Deficincy (ID). Eur. J. Heart Fail. 2009, 8, ii71.
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M.; et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J. Card. Fail. 2017, 23, 628–651.
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726.
