Encouraging results of EPO from basic research support the possibility of integrating its therapeutic effects in glaucomatous optic neuropathy, optic neuritis, non-arteritic anterior ischemic optic neuropathy (NAION), and traumatic optic neuropathy (TON).
Glaucomatous optic neuropathy, a neurodegenerative disease, is characterized by progressive loss of RGCs. Elevated intraocular pressure (IOP) is considered the most important risk factor of glaucomatous optic neuropathy. However, some patients experienced continued RGCs loss despite good intraocular pressure control, suggesting the presence of other complicated mechanisms stimulating RGC death. Multifactorial mechanisms have been postulated for glaucomatous optic neuropathy, including vascular insufficiency, inflammation [
66,
67], excitotoxicity [
68] and neurotrophic factor withdrawal [
69]. Due to the complex pathogenesis of glaucoma, EPO was developed to prevent the IOP-independent RGCs loss. Several studies have reported that the EPO level in the aqueous humor increased in patients with glaucoma [
70]. The cause of the elevated aqueous EPO in glaucomatous eyes might be related to the ischemia, hypoxia, or elevated ROS caused by glaucomatous damage [
71]. The increase in EPO is identified as a compensatory response due to the presence of glutamate, nitric oxide and the free radicals after the glaucomatous damage [
72]. EPO is found to have neuroprotective effects regardless of the EPO administration methods. However, the discussion of EPO in the treatment of glaucoma is limited to animal studies. In humans, there are only a few observational studies investigating the correlation between EPO and glaucoma, especially neovascular glaucoma [
79,
80,
81]. To date, human studies using EPO for the treatment of glaucoma are still lacking. Future studies could focus the application of EPO in patients with primary open-angle glaucoma to see if EPO exhibits the same neuroprotective effects in animal experiments.
Optic neuritis is another high occurring disease among the world population. For optic neuritis, methylprednisolone is the standard treatment in clinical practices. Although steroid treatment could accelerate visual acuity recovery, recent study demonstrates that steroids could not influence the visual outcome or atrophy of the optic nerve [
82]. An animal study even demonstrated that methylprednisolone could increase RGCs degeneration by inhibiting the neurotrophin pathway [
83]. Since EPO has shown multiple neurotrophin-like properties in various neuronal disorders, the efficacy of EPO is evaluated as an add-on therapy to methylprednisolone in autoimmune optic neuritis by investigators. In an experimental autoimmune encephalomyelitis (EAE) rat model, intraperitoneal injection of EPO (5000 U/kg) significantly increased the survivability and functionality of RGCs in rats afflicted with myelin oligodendrocyte glycoprotein (MOG)-induced optic neuritis [
84]. In the model of MOG-EAE, Sättler et al. concluded that the PI3-K/Akt pathway plays an important role in RGCs survivability under systemic treatment with EPO [
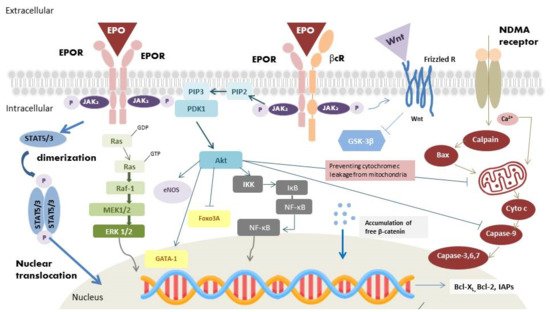
84]. Establishment of potentially relevant intracellular conduction pathways might make the application of EPO more feasible in MOG-EAE. Human studies have been performed, but the results were not conclusive.
For
traumatic optic neuropathy, indirect TON is the more common type. The shearing force could lead to small vessel and neuron axon injury around the optic nerve by inducing ischemia, inflammation, and oxidative stress, all of which result in ganglion cell death. Currently, the common treatments are observation, corticosteroids and optic canal decompression. However, none of these managements are proven to be effective. Since EPO has shown to be neuroprotective, EPO might play a role in treating indirect TON. Intravenous EPO was first commenced in patients with indirect TON by Kashkouli et al. in 2011 [
92]. Indirect TON patients with intravenous EPO (10,000 IU in 3 days) were compared to indirect TON patients without treatment. They found that the EPO-treated group has higher BCVA than that in the observation group. They advocated intravenous EPO may be a new effective and safe treatment in patients with indirect TON [
92].
5. Advances in EPO Derivatives
Epoetin alfa (Epogen), a type of ESA medicine, has been the standard of care for patients with kidney disease and cancer-related anemia. Epoetin alfa-epbx (RetacritTM) shares the same amino acid sequence and similar carbohydrate composition as epoetin alfa (EpogenTM). In 2018, the protein was approved by the FDA, making it the first biosimilar EPO molecules approved in the USA [97]. Darbepoetin alfa (DA, Aranesp), an alternative agent of Epoetin alfa and a hyperglycosylated EPO analog, is a novel ESA with two additional N-glycosylation sites accompanied by 22 sialic acid moieties. In the attempt to extend the molecule’s half-life by three-fold longer than EPO in vivo, glycoengineering was conducted to increase the structure’s resistance to degradation. Darbepoetin alfa was approved for treating anemia resulting from renal diseases and cancer chemotherapy. The treatment protocol only requires a once-per-week visit and is accompanied by lower clinical costs [98,99]. C.E.R.A. (continuous erythropoietin receptor activator), a third-generation ESA, is an EPO (~34 kDa) integrated with methoxypolyethylene glycol (PEG, 30 kDa). Compared with other EPO derivatives, C.E.R.A. has a unique pharmacological profile with the longest half-life and slowest clearance rate. These unique pharmacological properties exist because of methoxypolyethylene glycol (PEG) integration into EPO. Notably, EPO pegylation (the process of connecting a hydrophilic polymer to EPO) significantly prolongs the duration of EPO action, and enhances proteolytic resistance in cell-free plasma [100].
Asialerythropoietin (asialoEPO) was evaluated to be a safe drug for clinical treatments. However, asialoEPO’s half-life (t1/2~1.14 min) is much shorter than that of EPO (t1/2~5.6 h). The short half-life gives asialoEPO insufficient persistence time to stimulate hematopoiesis. Based on the above concept, researchers found that chemical modification of the EPO binding sites could abolish erythropoiesis function but retain the tissue-protective effect. Carbamylated EPO (cEpo), a chemically modified derivative of EPO’s lysine residues, was found to act through the heterodimeric EPOR/βcR rather than classical EPOR2 primarily because of the modified structure of cEpo. The study has confirmed that cEpo possesses neuron anti-apoptotic effects similar to EPO but instead does not induce neovascularization [101].
6. Advances in EPO Delivery
6.1. Protein-Based Ocular Delivery
Many EPO studies involve frequent injections of ophthalmic proteins via invasive procedures, which might result in a variety of adverse effects and increase the probability of irreversible damage to the patient’s eye. Topical sustain released formulations are non-invasive drugs, that effectively reaches the posterior segment of the eye. According to Silva et al., mucoadhesive polymers such as chitosan and hyaluronic acid can improve the ocular bioavailability of drugs with the support of nanoparticulate delivery systems [
106]. The formulation was found to be non-cytotoxic toward ARPE-19 and HaCa T cell lines. CS/HA6-rhEPO may be a promising topical formulation after enhancing its bioavailability through different ocular barriers. For the intraocular route of administration, De Julius et al. developed two polymer microparticles, poly (propylene sulfide) (PPS) and poly (lactic-co-glycolic acid) (PLGA), to prolong His-tagged rhEPO-R76E (42kDa) release [
107]. The rhEPO-R76E was loaded into the polymeric microparticles to prolong in vivo release for at least 28 days to resolve the issue involving short half-life of the rhEPO-R76E (t1/2~13 min). PPS-based microparticles platform is especially promising because it is degradable by ROS. The delivery system provides extended neuroprotection and inherent antioxidant benefits, which reinforces its ability in ocular delivery of EPO.
6.2. Gene-Based Ocular Delivery
Under the gene delivery approaches, EPO has significant therapeutic potential in neurodegenerative diseases due to its neuroprotective effects. However, recombinant EPO is limited in clinical treatment of glaucoma patients due to its short half-life. As regards this issue, Bond et al. constructed a viral gene delivery system for EPO-R76E [
108]. Treatment with recombinant adeno-associated virus (rAAV) provides sustainable, long-term delivery of EPO-R76E without a critical rise in hematocrit [
108,
109]. AAV-mediated long-term EPO expression is achievable in animal models with the primary functions of promoting red blood cells proliferation and neuroprotection.
Another challenge in applying gene therapy in humans is the improvement of drug selectivity. For systemically secreted hormone, such as EPO, it is vital to use an inducible genetic delivery system to avoid excess expression and side effects. However, precise expression control is highly desirable when maintaining steady-state red blood cell counts within a narrow therapeutic window. Hines-Beard et al. packaged EPOR76E into a recombinant adeno-associated viral vector under the control of the tetracycline inducible promoter [
110]. In the retina, tetracycline-controlled expression of green fluoresce protein (GFP) in retinal pigmented epithelium and photoreceptor cells becomes apparent in rats following subretinal injections of rAAV-2/2 vector. The outer nuclear layer in the eyes was approximately 8 μm thicker in mice that received doxycycline water as compared to the control groups.
6.3. Surface Receptor-Targeted Ocular Delivery
Through surface receptor-targeted delivery results, most suggest that the tissue-protective effect of EPO and injury response are mediated by the EPOR/βcR heterodimer and not by the EPOR homodimer [
112]. In addition to some well-known derivatives of EPO with better affinity for the EPOR/βcR heterodimer, such as asialoEPO, cEpo and HBSP (see above), traptamers of transmembrane domain (TMD) proteins of EPOR/βcR are also an option. He et al. constructed ELI-3 traptamer that specifically targets the TMD of human EPOR and triggers cooperative JAK/STAT signaling for proliferation and tissue protection [
113].
6.4. Cell-Based Ocular Delivery
Mesenchymal stem cell (MSC) therapy is potential in treating optic neuropathies. MSCs have demonstrated to possess neuroprotective effects in numerous neurodegenerative diseases while maintaining retinal morphology [
114,
115]. They could also regulate inflammatory responses [
116] and increase the secretion of neurotrophic factors [
117]. Furthermore, they could transdifferentiate into retinal progenitor cells [
118]. MSCs could be the vector of EPO because these cells could cross the brain-retinal barrier and localize into the inflamed sites [
121]. The phenomenon emphasizes a mutualistic relationship between MSCs and EPO. Hence, some investigators attempt to evaluate the efficacy of EPO-expressing MSC in treating retinal degenerative diseases. Ding et al. transduced MSCs with lentiviral particles encoding EPO. They found that co-treatment with EPO and MSCs instead of only with MSC could attenuate human retinal neuron apoptosis by restoring the mitochondrial membrane potential and protect human retinal neurons from glutamate neurotoxicity [
122]. The ability for EPO to synchronize with MSCs may become beneficial in producing medical protocols involving the treatment of patients with glaucomatous optic neuropathy. Given their endogenous long-term therapeutic effects, MSCs-based therapy could be the future direction in optic nerve repair.