Recently, various drug and gene delivery systems employing physical energy, such as ultrasound, magnetic force, electric force, and light, have been developed. Ultrasound-mediated delivery has particularly attracted interest due to its safety and low costs. Ultrasound exposure increases cell membrane permeability and facilitates the delivery of drugs or genes into cells. Its delivery effects are also enhanced when combined with microbubbles or nanobubbles that entrap an ultrasound contrast gas. Furthermore, ultrasound-mediated nucleic acid delivery could be performed only in ultrasound exposed area.
- ultrasound
- microbubble
- nanobubble
1. Introduction
Gene therapies are expected to be effective therapeutic strategies for intractable diseases such as cancers as well as genetic and inflammatory diseases. In recent years, the number of gene therapy targeted diseases has been increasing, and neurodegenerative and cardiovascular diseases that demonstrate an increased risk due to aging have also been attracting considerable attention as probable targets. For instance, gene therapies for Parkinson’s disease, Alzheimer’s disease, and ischemic disease are actively being studied. However, the safe and efficient delivery of nucleic acids is a major obstacle in their development. In particular, for RNAi-based gene therapies, it is important to avoid degradation by nuclease and their rapid removal from circulation. Various technologies, such as chemical modifications of RNA and nanoparticle-based delivery systems, have been proposed [1,2,3,4,5]. Recently, methods of RNA delivery with external stimuli, including light, ultrasound, electrical fields, and magnetic fields, have been investigated and are expected to improve transfection and therapeutic efficiencies [6,7]. Nanomaterials have been widely used with external stimuli to amplify energy, induce release from carriers, and transfer to target site. These methods show little effect until stimulated with external energy and are thought to be safe for nontarget tissues without stimuli. Furthermore, the development of theranostic (a term for combining therapeutics and diagnostics) nanoparticles has gained attention. Various combinations of nanoparticles with external stimuli are reported to facilitate not only nucleic acid delivery, but also optical imaging, magnetic resonance imaging, nuclear imaging, and computed tomography [8,9,10,11] (Figure 1). Ultrasound imaging is used frequently in clinical settings and valuable for the early detection or follow-up of chronic diseases that increase with age. Furthermore, as it is convenient and non-invasive, ultrasound technology is expected to be a useful theranostic tool. Contrast agents, called microbubbles, are often used in combination with ultrasound to improve the resolution and sensitivity of the imaging. In recent years, nanoscale contrast agents have been developed. Furthermore, micro- or nanobubbles have previously been investigated as site-specific drug or gene delivery tools [12,13,14,15,16,17]. To exploit the combination of ultrasound and bubbles both for diagnosis and therapeutics as a theranostic system, various types of bubbles valuable for systemic administration have been well documented in recent years.
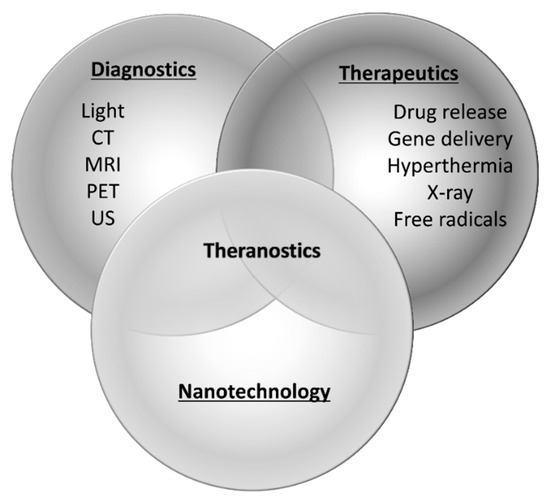
Figure 1. Paradigm of theranostics. CT; computed tomography, MRI; magnetic resonance imaging, PET; positron emission tomography, US; ultrasound.
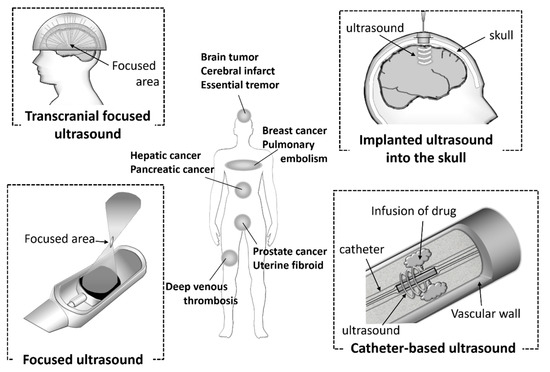
2. Various Ultrasound Devices and Ultrasound Delivery in Clinical Use
3. Concluding
The mechanisms of aging and the onset of many diseases have been identified at the genetic level. Furthermore, the elucidation of gene regulatory networks and the development of technologies for nucleic acid synthesis are also progressing rapidly. In these situations, novel therapies with nucleic acids have become increasingly important. The delivery of nucleic acids by a combination of ultrasound and micro- or nano-bubbles, has been shown to be effective in the treatment of diseases such as cardiovascular disease, CNS disease, and tumors. Low power ultrasound technology, which is used for imaging, is well known to be noninvasive and can be used repeatedly. Whereas, high power ultrasound already used clinically, for instance in the ablation of cancer, could cause undesirable bioeffects due to its high intensity [32]. Therefore, high power therapeutic ultrasound is used, paying careful attention to the safety of patients. Unfortunately, it is not obvious the bioeffects by ultrasound for micro- or nanobubbles-based gene therapies. For the realization of clinical application, more detailed information about safety is required, and it is essential to establish appropriate ultrasound conditions which can also be used repeatedly. Owing to the possibility of repeated use and device miniaturization, it is particularly advantageous in elderly patients, particularly for in home care which will continue growing in the near future. However, the development of bubbles which is useful both for diagnosis and therapy is not sufficient, although various ultrasound devices are developed remarkably and widely spread in clinical settings. As the development of useful bubble formulations progresses, the combination of bubbles and ultrasound is highly valuable for the assembly of a theranostic system in the diagnosis and therapy of diseases that increase in risk due to aging.
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics12100964
