Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Rheumatology
Rheumatoid arthritis (RA) is a chronic, inflammatory synovitis-based systemic immune disease of unknown etiology. In addition to joint pathological damage, RA has been linked to neuropsychiatric comorbidities, including depression, schizophrenia, and anxiety, increasing the risk of neurodegenerative diseases in life.
- rheumatoid arthritis
- affective disturbance
1. Psychiatric Comorbidities
Compared with the general population, rheumatoid arthritis (RA) patients are known to endure a higher chance of developing psychiatric comorbidities including depression [11] and anxiety, mood, and psychotic disturbances [12], which greatly reduce the quality of life and physical and mental health. Compared with people without physical defects or recurring pain [13], mental health disorders in RA patients are associated with harmful effects such as pain, fatigue, impaired sleep quality, increased mental health-related distress, and passive pain-coping strategies [14,15]. Psychiatric comorbidities also adversely affect multiple outcomes in RA patients [16], including poor medication adherence and treatment response (Figure 1) [17]. For example, RA patients with depression are associated with an inferior response to biological therapy [18].
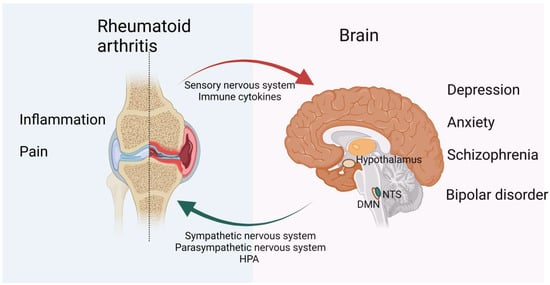
Figure 1. Bidirectional psychological and neurological effects of RA and the brain on each other. Recurrent pain and prolonged inflammation are prominent symptoms of RA and are strongly associated with mental illnesses such as depression and anxiety. In contrast, mental health can influence RA disease activity and is associated with reduced treatment response in RA patients. For example, patients with depression have an increased risk of RA, while antidepressants are reported to have a protective and therefore confounding effect on RA. The CNS and PNS both play a role in inflammation. The vagus nerve is the main efferent pathway that mediates immunosuppression of the CNS. It controls the production of TNF and other proinflammatory cytokines through the splenic nerve. Sensory nerves are activated by proinflammatory cytokines, such as IL-1 and IL-6, and sensory immune information is then sent to regions of the brain and spinal cord to mount an appropriate response. The HPA axis and SNS then carry information from the CNS to the PNS. While the parasympathetic nervous system is anti-inflammatory in the first phase of inflammation, its role in the later phases of chronic inflammation requires further research. Figure created using BioRender (https://biorender.com, accessed on 20 July 2022).
Depression and anxiety disorders are relatively well-recognized and studied psychiatric disorders in RA patients. However, due to many reasons, the estimated prevalence of these two differs rather largely from study to study, the incidence of anxiety and depression in RA patients appears to range from 26% to 46% and 14.8% to 34.2%, respectively [19]. In addition, the etiology behind it has not been adequately studied [20].
2. Depression
Among the related psychiatric disorder in RA, depression is the most closely associated one [21]. However, estimates of the prevalence of depression are influenced by many factors, including differences in measurement methods, recurrence of depressive symptoms, and variances in disease duration [19]. In addition, there are some overlapping diagnostic symptoms existing both in RA and depression, such as fatigue, poor appetite, and sleeping disturbance, thus some studies have removed items that may overlap between the two diseases or adjusted diagnostic thresholds, inevitably affecting the prevalence statistics of RA patients and depression [22].
Nonetheless, the evidence for the negative impacts of depression on the course of RA is convincing. Notably, previous studies have shown that depression accounts for 6.9% of mortality in RA patients [23] and is associated with increased mobility in RA, impaired quality of life, reduced chance of remission and increased arthritis-related complications [24]. The feelings of hopelessness and non-adherence to treatment caused by depression can also further aggravate the disease, which may explain why patients with moderate, severe, or people with chronic depression are less likely to follow medical guidance than people with mild or no depression, regardless of the medical condition [25]. For example, people with rheumatoid arthritis who suffer from chronic depression are less likely to take their doctor’s advice and are less likely to take disease-modifying antirheumatic drugs (DMARDs) as prescribed than patients with milder or subclinical levels of depression. According to the inflammatory hypothesis, depression may also be responsible for the increase in inflammation and disease activity in RA [26].
In recent years, several studies have also found a bidirectional relationship between depression and rheumatoid arthritis. Notably, in addition to the high incidence of depression in RA patients, people with depression are at greater risk of developing rheumatoid arthritis than the general population [27], and antidepressants are reported to have a protective and therefore confounding effect on RA [28]. In addition, excessive activation of the hypothalamic-pituitary-adrenal (HPA) axis due to cytokine activity has also been associated with depression [29].
3. Anxiety
The prevalence of psychological comorbidities in RA patients has been extensively researched, particularly depression and anxiety [20]. Several studies have noted that anxiety is more common than depression in people with rheumatoid arthritis [30]. The prevalence of anxiety in RA patients, however, differs across research from 20% to 26% of patients classified as having obvious anxiety disorders or anxiety-like symptoms [31,32]. In addition, depressed RA patients are more likely to experience symptoms of anxiety compared with general RA patients or age-matched individuals [20].
Anxiety in RA patients is related to multiple factors, such as age, sex, socioeconomic status, pain, marital status, and disease activity [32,33,34]. Anxiety symptoms in RA patients are linked to a lower quality of life [35] and poor therapeutic response, which are similar to depression. For example, persistent anxiety in RA patients can reduce treatment response to prednisolone by 50% [36].
Research on anxiety shares common problems with depression, such as small populations with various prevalence estimates [19] and overlapping diagnostic symptoms. Regarding the impact of RA on patient anxiety, studies have reported that c-reactive protein (CRP) levels may be correlated with anxiety and depression levels in RA patients [34]. However, it is still unclear if RA increases the prevalence of anxiety independently or if this association is confounded by the anxiety tendencies that are already existed [37], and thus more research is needed.
4. Schizophrenia
In comparison to the general population, patients with RA have a rather low prevalence of schizophrenia, according to clinical and epidemiological studies [38]. The risk of RA in schizophrenic patients is estimated to be 30–50% of the control [39]. One common theory to explain this is the abnormal inflammatory cytokine profile in schizophrenia patients, which includes circulating proinflammatory cytokines [40], elevated levels of soluble IL-2 receptor, aberrant tryptophan metabolism, prostaglandin insufficiency, and therapy side effects that are linked to RA-schizophrenia [41]. As noted previously, high blood concentrations of IL-1 receptor antagonists may have protective effects against RA in schizophrenic patients [42].
Genetics is another important factor in both diseases. Notably, based on the well-studied human leucocyte antigen (HLA) system [43], HLADRB1*0101, HLA-DRB1*04 (*0401, *0403, *0405, and *0406), and HLA class II antigens and alleles have been implicated in the regulation of antibody-mediated immune responses [44]. HLA-DRB1, including HLA-DR4 serotypes, positively correlated with RA incidence and negatively correlated with schizophrenia levels [45]. Therefore, it could be assumed that the negative genetic correlation between RA and schizophrenia may be due to the different roles of variants in immune response pathways in different tissues and/or in response to different challenges [41].
5. Bipolar Disorder
Although autoimmune diseases are associated with psychiatric disorders, especially depression and anxiety, little research has been done on the relationship between rheumatoid arthritis and bipolar disorder [46]. In addition, asthma, cirrhosis, and alcoholism are important risk factors for developing bipolar disorder [47].
Research has also suggested that peripheral chronic inflammation is a key factor in the pathophysiology of CNS inflammation in bipolar disorder [48]. Thus, RA is a disease characterized by long-term chronic inflammation, and the process of inflammatory immune response activated by RA may affect the prognosis and development of bipolar disorder.
Sex-related characteristics have also been found to play a key role in developing bipolar disorder in RA patients. Bipolar disorder is equally prevalent in men and women, according to epidemiological studies [49]. Female RA patients are more likely to acquire bipolar disorder compared to women without RA. This may be due to sex steroid hormones, which play an important regulatory role in immune responses; specifically, estrogen-induced immune stimulation in RA may be more likely to trigger inflammation [50]. However, further clinical and basic research is needed on the relationship between RA and bipolar disorder.
This entry is adapted from the peer-reviewed paper 10.3390/ijms23158158
This entry is offline, you can click here to edit this entry!
