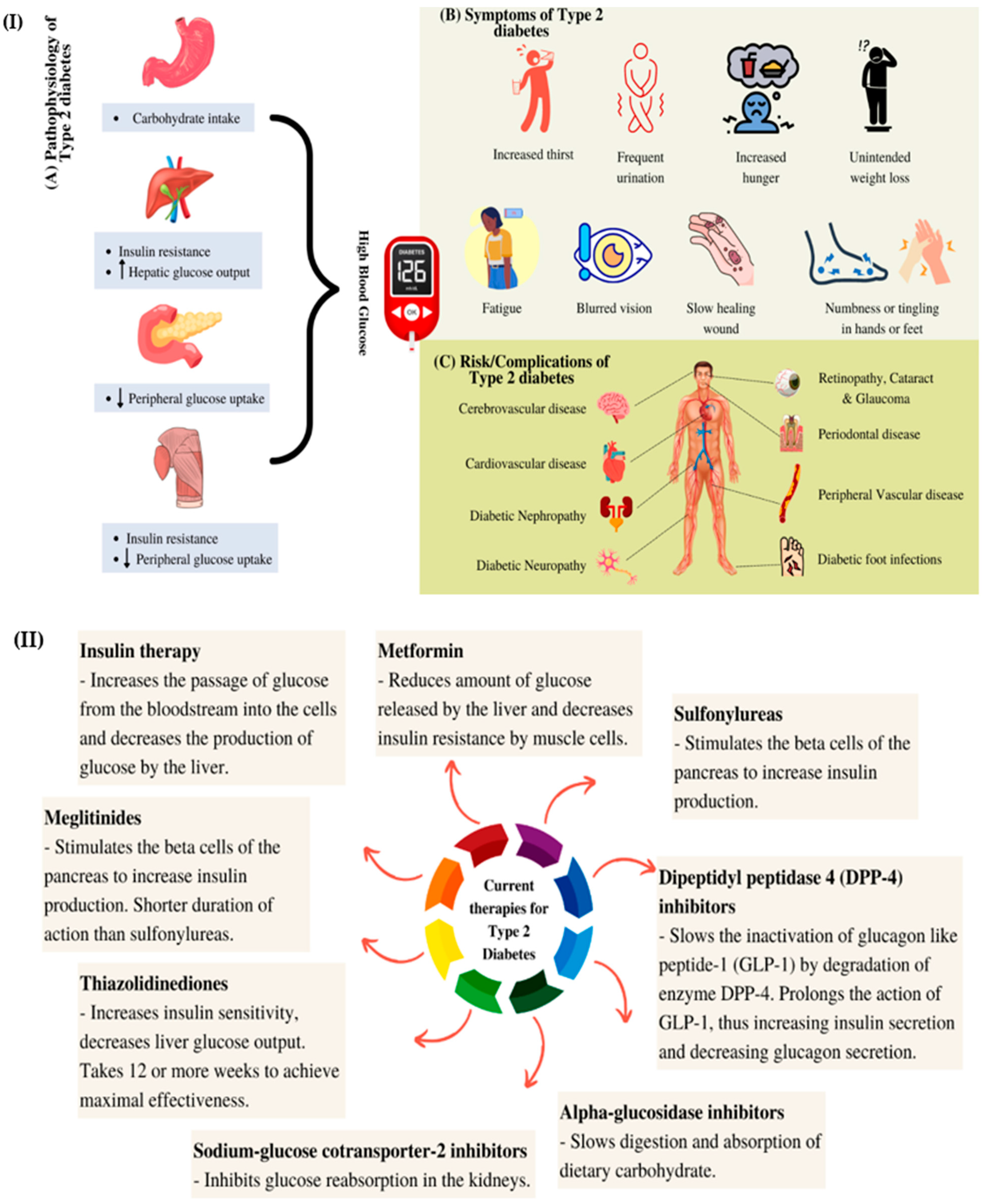
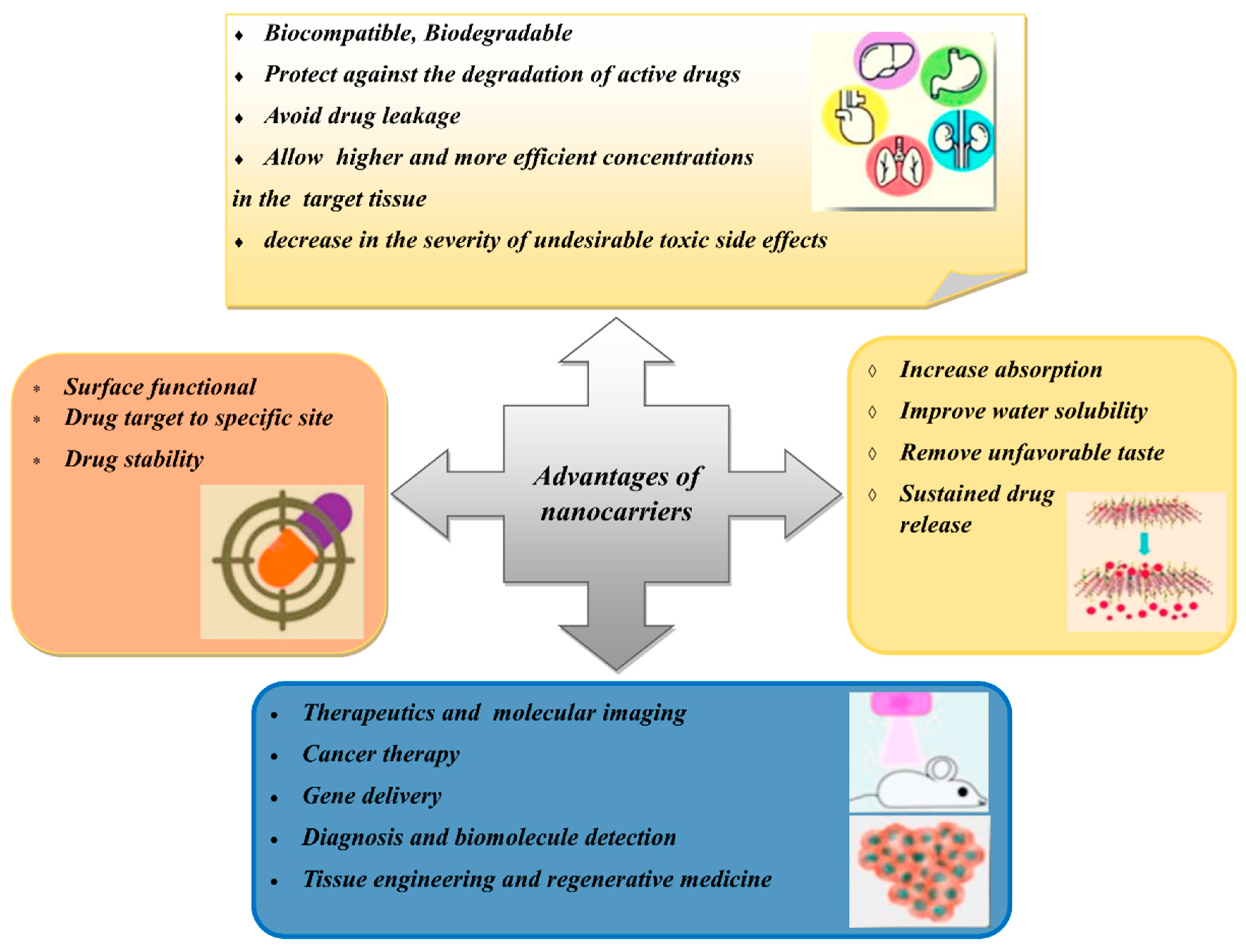
Diabetes mellitus is a prevalent metabolic syndrome that is associated with high blood glucose levels. The number of diabetic patients is increasing every year and the total number of cases is expected to reach more than 600 million worldwide by 2045. Modern antidiabetic drugs alleviate hyperglycaemia and complications that are caused by high blood glucose levels. Due to the side effects of these drugs, plant extracts and bioactive compounds with antidiabetic properties have been gaining attention as alternative treatments for diabetes. Natural products are biocompatible, cheaper and expected to cause fewer side effects than the current antidiabetic drugs. Various nanocarrier systems are discussed, such as liposomes, niosomes, polymeric nanoparticles, nanoemulsions, solid lipid nanoparticles and metallic nanoparticles. These systems have been applied to overcome the limitations of the current drugs and simultaneously improve the efficacy of plant-based antidiabetic drugs. The main challenges in the formulation of plant-based nanocarriers are the loading capacity of the plant extracts and the stability of the carriers. Lipid nanocarriers and the amphipathic properties of phospholipids and liposomes that encapsulate hydrophilic, hydrophobic and amphiphilic drugs is also described. A special emphasis is placed on metallic nanoparticles, with their advantages and associated complications being reported to highlight their effectiveness for treating hyperglycaemia.
- antidiabetic
- plant extract
- nanocarriers
1. Introduction
2. Natural Active Agents in Nanocarriers
| Plant Part | Scientific Name | Common Name | Antidiabetic and Other Biological Activities | Ref. |
|---|---|---|---|---|
| Bark | Pterocarpus marsupium | Indian kino tree | Antidiabetic and hypoglycaemic | [20] |
| Fruit | Momordica charantia | Bitter melon | Antidiabetic and hypoglycaemic | [21] |
| Leaf | Gymnema sylvestre | Gurmar | Hypoglycaemic and hypolipidemic | [22] |
| Catharanthus roseus | Nayantara | Hypoglycaemic | [23] | |
| Azadirachta indica | Neem | Hypoglycaemic | [23] | |
| Ocimum sanctum | Holy basil | Antidiabetic and hypoglycaemic | [20] | |
| Aloe vera | Aloe vera | Antidiabetic, antihypercholesterolemic and antioxidative | [24] | |
| Rhizome | Curcuma longa | Turmeric | Antidiabetic, antioxidant and anticholinesterase | [25] |
| Seed | Allium sativum | Garlic | Hypoglycaemic | [23] |
| Trigonella foenum-graecum | Fenugreek | Antidiabetic and hypoglycaemic | [20] | |
| Stem | Tinospora cordifolia | Giloy | Hypoglycaemic | [26] |
3. Types of Nanocarriers for Plant-Based Antidiabetic Extracts/Active Agents
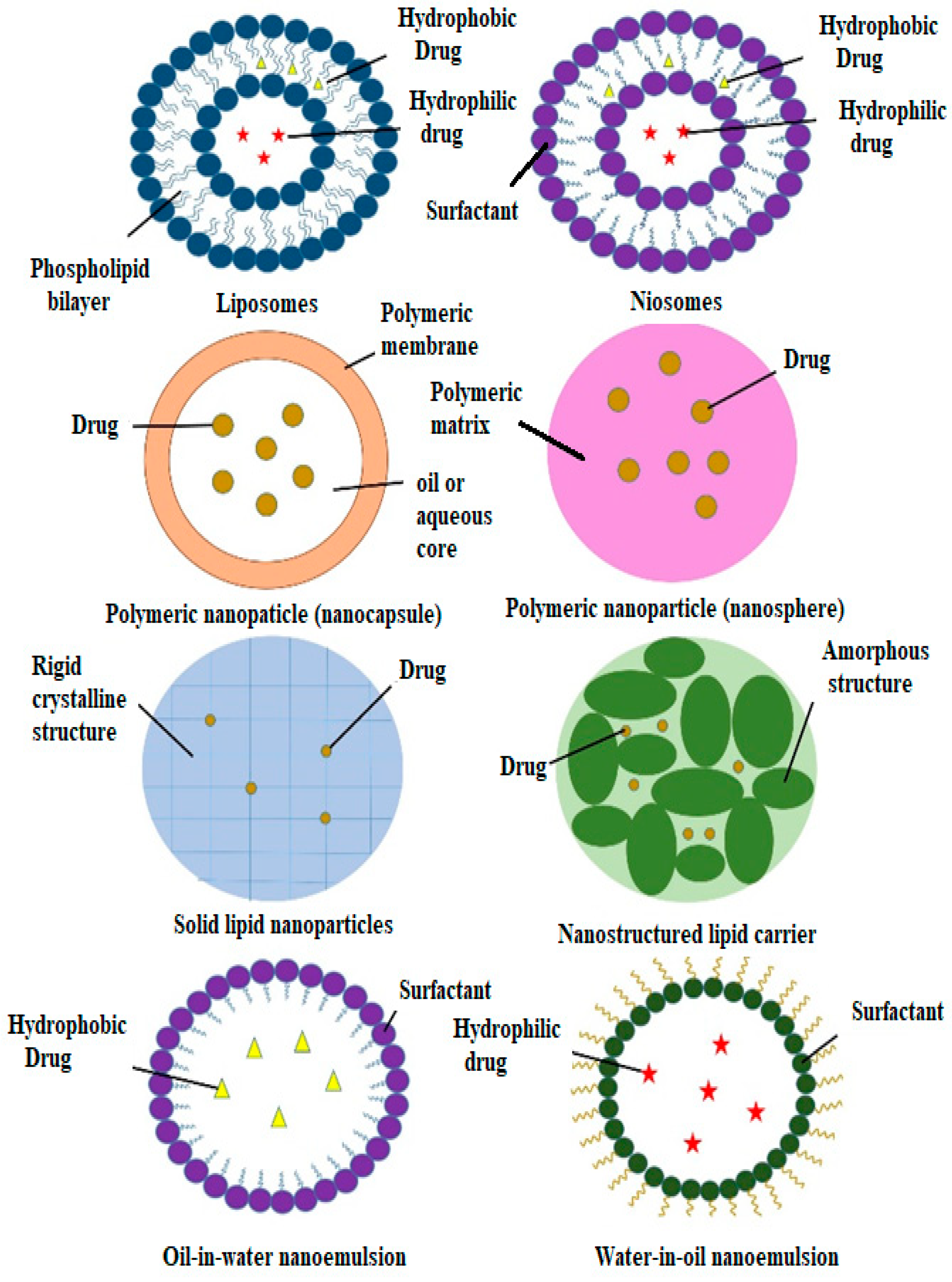
3.1. Liposomes
| Type of Nanocarrier | Formulation (Ratio) | Active Compound | Model | Size Range (nm) | Remark | Ref. |
|---|---|---|---|---|---|---|
| Liposomes | Lecithin | Betanin | Streptozotocin-induced diabetic rats | 40.06 ± 6.21 | Increased hypoglycaemic activity; antihyperlipidemic activity; decreased oxidative stress | [65] |
| DPPC, PEG-2000-DSPE and cholesterol (9.5:0.5:1) | Curcumin | Streptozotocin-induced diabetic rats | 140 | Increased hypoglycaemic activity; hepatoprotective effects; decreased oxidative stress | [66] | |
| Phosphatidylcholine and cholesterol (8:2) | Momordica charantia, Trigonella foenum-graecum and Withania somnifera extracts | Albino Wistar rats | 1176 ± 5.6 | Increased hypoglycaemic activity; antihyperlipidemic activity | [69] | |
| Niosomes | Span 60 and cholesterol (1:1) | Lycopene | Alloxan-induced diabetic rats | 202 ± 41 | Increased hypoglycaemic activity; antihyperlipidemic activity | [70] |
| Span 60, phospholipid 90G and cholesterol (9:4:1) | Embelin | Streptozotocin-induced diabetic rats | 609–734 | Increased hypoglycaemic activity; antioxidant efficacy | [71] | |
| Span 40 and cholesterol (1:2) | Gymnema sylvestre extract | Alloxan-induced diabetic rats | 229.5 ± 30 | Increased hypoglycaemic activity | [72] | |
| Polymeric Nanoparticles |
Poly-(ε-caprolactone) (PCL) and PLGA-PEG-COOH | Fisetin | In vitro assays | 140–200 | Better α-glucosidase inhibition than acarbose; scavenging capacity | [73] |
| Eudragit RS100 | Phoenix dactylifera seed oil | In vitro assays | 207 | α-amylase and α-glucosidase inhibition | [74] | |
| Chitosan | Curcumin | In vitro assays | 74 | Increased GLUT-4 levels | [75] | |
| Chitosan and alginate (3:1) | Naringenin | Streptozotocin-induced diabetic rats | 150–300 | Increased hypoglycaemic activity | [76] | |
| Chitosan and alginate (1:3) | Quercetin | Streptozotocin-induced diabetic rats | 91.58 | Increased hypoglycaemic activity | [77] | |
| Chitosan and gum arabic | Glycyrrhizin | Streptozotocin-induced diabetic rats | 165.3 | Increased hypoglycaemic activity | ||
| Chitosan and tripolyphosphate (4:1) | Ferulic acid | Streptozotocin-induced diabetic rats | 51.2 ± 1.7 | Increased hypoglycaemic activity; increased body weight | [78] | |
| Chitosan, gum Arabic and Tween 60 | Glycyrrhizin | Streptozotocin- and nicotinamide-induced diabetic rats | 181.4 | Increased hypoglycaemic activity; reduced body weight and lipid levels | [79] | |
| Polyvinyl alcohol (PVA), Tween 80, gum-rosin polymer and oleic acid | Thymoquinone | Streptozotocin- and nicotinamide-induced diabetic rats | 70.21 | Increased hypoglycaemic activity; reduced body weight and lipid levels | [80] | |
| Gum rosin, PVA and lecithin | Thymoquinone | Streptozotocin-induced diabetic rats | 36.83 ± 0.32 | Increased hypoglycaemic activity | [81] | |
| PLGA | Quercetin | Streptozotocin-induced diabetic rats | 179.9 ± 11.2 | Increased hypoglycaemic activity; increased levels of catalase and superoxide dismutase | [82] | |
| PLGA | Pelargonidin | Streptozotocin-induced diabetic rats | 91.47 ± 2.89 | Increased hypoglycaemic activity; antihyperlipidemic activity | [83] | |
| PLGA, Pluronic F-127 and chitosan | Silybin | Streptozotocin-induced diabetic rats | 184.6 | Increased hypoglycaemic activity | [84] | |
| PLGA and PVA | Ethyl acetate | In vitro assays | 365.7 | α-amylase and α-glucosidase inhibition | [85] | |
| Tween 20 and propylene glycol | Foeniculum vulgare Mill. essential oil | Streptozotocin-induced diabetic rats | 44–105 | Increased hypoglycaemic activity | [86] | |
| Nanoemulsions | Tween 20 and polyethylene (PEG) 400 | Ipomoea reptans extract | - | 15.5 ± 0.8 | - | [87] |
| Lecithin | Resveratrol | Streptozotocin + nicotinamide-induced diabetic rats | 248 | Increased hypoglycaemic activity; prevention of weight loss | [88] | |
| Solid Lipid Nanoparticles | Compritol, Tween 80 and Span 20 | Myricitrin | Streptozotocin + nicotinamide-induced diabetic rats | 76.1 | Increased hypoglycaemic activity; antioxidant and anti-apoptotic effects | [89] |
| Glycerol tripalmitate and soybean phospholipid | Berberine | Male rats | 76.8 | Increased hypoglycaemic activity; prevention of weight gain | [90] | |
| Nanostructured Lipid Carriers | Precirol and miglyol (5:2) | Baicalin | Streptozotocin-induced diabetic rats | 92 ± 3.1 | Increased hypoglycaemic activity | [91] |
3.2. Niosomes
This entry is adapted from the peer-reviewed paper 10.3390/polym14152991
References
- Chaudhury, A.; Duvoor, C.; Dendi, V.S.R.; Kraleti, S.; Chada, A.; Ravilla, R.; Marco, A.; Shekhawat, N.S.; Montales, M.T.; Kuriakose, K.; et al. Clinical review of antidiabetic drugs: Implications for type 2 diabetes mellitus management. Front. Endocrinol. 2017, 8, 6.
- Verma, S.; Gupta, M.; Popli, H.; Aggarwal, G. Diabetes mellitus treatment using herbal drugs. Int. J. Phytomedicine 2018, 10, 1–10.
- Roden, M.; Shulman, G.I. The integrative biology of type 2 diabetes. Nature 2019, 576, 51–60.
- Chatterjee, S.; Khunti, K.; Davies, M.J. Type 2 diabetes. Lancet 2017, 389, 2239–2251.
- Saberzadeh-Ardestani, B.; Karamzadeh, R.; Basiri, M.; Hajizadeh-Saffar, E.; Farhadi, A.; Shapiro, A.M.J.; Tahamtani, Y.; Baharvand, H. Type 1 diabetes mellitus: Cellular and molecular pathophysiology at a glance. Cell J. 2018, 20, 294–301.
- Galicia-Garcia, U.; Benito-Vicente, A.; Jebari, S.; Larrea-Sebal, A.; Siddiqi, H.; Uribe, K.B.; Ostolaza, H.; Martín, C. Pathophysiology of type 2 diabetes mellitus. Int. J. Mol. Sci. 2020, 21, 6275.
- Ozougwu, J.C.; Obimba, K.C.; Belonwu, C.D.; Unakalamba, C.B. The pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. J. Physiol. Pathophysiol. 2013, 4, 46–57.
- Lotfy, M.; Adeghate, J.; Kalasz, H.; Singh, J.; Adeghate, E. Chronic complications of diabetes mellitus: A mini review. Curr. Diabetes Rev. 2017, 13, 3–10.
- Feingold, K.R.; Anawalt, B.; Boyce, A.; Chrousos, G.; de Herder, W.W.; Dungan, K.; Grossman, A.; Hershman, J.M.; Hofland, H.J.; Kaltsas, G.; et al. Approach to the Patient with Dyslipidemia. In Endotext; Feingold, K.R., Ed.; MDText.com, Inc.: South Dartmouth, MA, USA, 2020.
- Choudhury, H.; Pandey, M.; Hua, C.K.; Mun, C.S.; Jing, J.K.; Kong, L.; Ern, L.Y.; Ashraf, N.A.; Kit, S.W.; Yee, T.S.; et al. An update on natural compounds in the remedy of diabetes mellitus: A systematic review. J. Tradit. Complement. Med. 2018, 8, 361–376.
- Lai, W.F. Development of hydrogels with self-healing properties for delivery of bioactive agents. Mol. Pharm. 2021, 18, 1833–1841.
- Obireddy, S.R.; Lai, W.F. Multi-component hydrogel beads incorporated with reduced graphene oxide for ph-responsive and controlled co-delivery of multiple agents. Pharmaceutics 2021, 13, 313.
- Khan, M.S.A.; Ahmad, I.; Khan, M.S.A.; Ahmad, I.; Chattopadhyay, D. New Look to Phytomedicine, 1st ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 3–13.
- Rashrash, M.; Schommer, J.C.; Brown, L.M. Prevalence and predictors of herbal medicine use among adults in the United States. J. Patient Exp. 2017, 4, 108–113.
- Nooreen, Z.; Rai, V.K.; Yadav, N.P. Phytopharmaceuticals: A new class of drug in India. Ann. Phytomed. 2018, 7, 27–37.
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharm. 2014, 4, 177.
- Bonifácio, B.V.; da Silva, P.B.; Ramos, M.A.D.S.; Negri, K.M.S.; Bauab, T.M.; Chorilli, M. Nanotechnology-based drug delivery systems and herbal medicines: A review. Int. J. Nanomed. 2014, 9, 1–15.
- Tran, N.; Pham, B.; Le, L. Bioactive compounds in anti-diabetic plants: From herbal medicine to modern drug discovery. Biology 2020, 9, 252.
- William, T.C.; Jianping, Y.; Zhong, Q.W. Efficacy of Dietary Supplementation with Botanicals on Carbohydrate Metabolism in Humans. Endocr. Metab. Immune Disord Drug Targets 2008, 8, 78–81.
- Vats, V.; Grover, J.K.; Rathi, S.S. Evaluation of anti-hyperglycemic and hypoglycemic effect of Trigonella foenum-graecum Linn, Ocimum sanctum Linn and Pterocarpus marsupium Linn in normal and alloxanized diabetic rats. J. Ethnopharmacol. 2002, 79, 95–100.
- Leung, L.; Birtwhistle, R.; Kotecha, J.; Hannah, S.; Cuthbertson, S. Anti-diabetic and hypoglycaemic effects of Momordica charantia (bitter melon): A mini review. Br. J. Nutr. 2009, 102, 1703–1708.
- Mall, G.K.; Mishra, P.K.; Prakash, V. Antidiabetic and hypolipidemic activity of Gymnema sylvestre in alloxan induced diabetic rats. Glob. J. Biotechnol. Biochem. 2009, 4, 37–42.
- Mostofa, M.; Choudhury, M.E.; Hossain, M.A.; Islam, M.Z.; Islam, M.S.; Sumon, M.H. Effects of Catharanthus roseus, Azadirachta indica, Allium sativum and glimepride in experimentally diabetic induced rat. Bangladesh J. Vet. Med. 2007, 5, 99–102.
- Mohamed, E.A.K. Antidiabetic, antihypercholestermic and antioxidative effect of Aloe vera gel extract in alloxan induced diabetic rats. Aust. J. Basic Appl. Sci. 2011, 5, 1321–1327.
- Kalaycıoğlu, Z.; Gazioğlu, I.; Erim, F.B. Comparison of antioxidant, anticholinesterase, and antidiabetic activities of three curcuminoids isolated from Curcuma longa L. Nat. Prod. Res. 2017, 31, 2914–2917.
- Patel, M.B.; Mishra, S. Hypoglycemic activity of alkaloidal fraction of Tinospora cordifolia. Phytomedicine 2011, 18, 1045–1052.
- Harwansh, R.K.; Deshmukh, R.; Rahman, M.A. Nanoemulsion: Promising nanocarrier system for delivery of herbal bioactives. J. Drug Deliv. Sci. Technol. 2019, 51, 224–233.
- Shishir, M.R.I.; Karim, N.; Gowd, V.; Zheng, X.; Chen, W. Liposomal delivery of natural product: A promising approach in health research. Trends Food Sci. Technol. 2019, 85, 177–200.
- Gondim, B.L.C.; Oshiro-Júnior, J.A.; Fernanandes, F.H.A.; Nóbrega, F.P.; Castellano, L.R.C.; Medeiros, A.C.D. Plant extracts loaded in nanostructured drug delivery systems for treating parasitic and antimicrobial diseases. Curr. Pharm. Des. 2019, 25, 1604–1615.
- Bilia, A.R.; Bergonzi, M.C.; Guccione, C.; Manconi, M.; Fadda, A.M.; Sinico, C.J. Vesicles and micelles: Two versatile vectors for the delivery of natural products. Drug Deliv. Sci. Technol. 2016, 32, 241–255.
- Da Silva, F.L.O.; Marques, M.B.D.F.; Kato, K.C.; Carneiro, G. Nanonization techniques to overcome poor water-solubility with drugs. Expert Opin. Drug Discov. 2020, 15, 853–864.
- Coimbra, M.; Isacchi, B.; van Bloois, L.; Torano, J.S.; Ket, A.; Wu, X.; Broere, F.; Metselaar, J.M.; Rijcken, C.J.F.; Storm, G.; et al. Improving solubility and chemical stability of natural compounds for medicinal use by incorporation into liposomes. Int. J. Pharm. 2011, 416, 433–442.
- Singh, S.; Pandey, V.K.; Tewari, R.P.; Agarwal, V. Nanoparticle based drug delivery system: Advantages and applications. Nanoparticle based drug delivery system: Advantages and applications. Indian J. Sci. Technol. 2011, 4, 177–180.
- Subramanian, A.P.; Jaganathan, S.K.; Manikandan, A.; Pandiaraj, K.N.; Gomathi, N.; Upriyanto, E. Recent trends in nano-based drug delivery systems for efficient delivery of phytochemicals in chemotherapy. RSC Adv. 2016, 6, 48294–48314.
- Dewanjee, S.; Chakraborty, P.; Mukherjee, B.; De Feo, V. Plant-based antidiabetic nanoformulations: The emerging paradigm for effective therapy. Int. J. Mol. Sci. 2020, 21, 2217.
- Li, M.; Du, C.; Guo, N.; Teng, Y.; Meng, X.; Sun, H.; Li, S.; Yu, P.; Galons, H. Composition design and medical application of liposomes. Eur. J. Med. Chem. 2019, 164, 640–653.
- Pandey, H.; Rani, R.; Agarwal, V.; Pandey, H.; Rani, R.; Agarwal, V. Liposome and Their Applications in Cancer Therapy. Braz. Arch. Biol. Technol. 2016, 59, 1–10.
- He, H.; Lu, Y.; Qi, J.; Zhu, Q.; Chen, Z.; Wu, W. Adapting liposomes for oral drug delivery. Acta. Pharm. Sin. B 2019, 9, 36–48.
- Pattni, B.S.; Chupin, V.V.; Torchilin, V.P. New developments in liposomal drug delivery. Chem. Rev. 2015, 115, 10938–10966.
- Hua, S.; Wu, S.Y. The use of lipid-based nanocarriers for targeted pain therapies. Front. Pharm. 2013, 4, 143.
- Sharma, V.K.; Sarwa, K.K.; Mazumder, B.J. Fluidity enhancement: A critical factor for performance of liposomal transdermal drug delivery system. Liposome Res. 2014, 24, 83–89.
- Alavi, M.; Karimi, N.; Safaei, M. Application of various types of liposomes in drug delivery systems. Adv. Pharm. Bull. 2017, 7, 3–9.
- Valenzuela, S.M. Liposome Techniques for Synthesis of Biomimetic Lipid Membranes. In Nanobiotechnology of Biomimetic Membranes; Martin, D.K., Ed.; Springer: Boston, MA, USA, 2007; pp. 75–87.
- Greish, K. Enhanced permeability and retention effect for selective targeting of anticancer nanomedicine: Are we there yet? Drug Discov. Today Technol. 2012, 9, e161–e166.
- de Assis, L.M.; da Rosa Zavareze, E.; Prentice-Hernández, C.; de Souza-Soares, L.A. Revisão: Características de nanopartículas e potenciais aplicações em alimentos. Braz. J. Food Technol. 2012, 15, 99–109.
- Babazadeh, A.; Ghanbarzadeh, B.; Hamishehkar, H.J. Phosphatidylcholine-rutin complex as a potential nanocarrier for food applications. Funct. Foods 2017, 33, 134–141.
- Camilo, C.J.J.; Leite, D.O.D.; Silva, A.R.A.; Menezes, I.R.A.; Coutinho, H.D.M.; Costa, J.G.M. Lipid vesicles: Applications, principal components and methods used in their formulations. A review. Acta Biol. Colomb. 2020, 25, 339–352.
- Li, J.; Wang, X.; Zhang, T.; Wang, C.; Huang, Z.; Luo, X.; Deng, Y. A review on phospholipids and their main applications in drug delivery systems. Asian J. Pharm. Sci. 2015, 10, 81–98.
- Hu, S.; Niu, M.; Hu, F.; Lu, Y.; Qi, J.; Yin, Z.; Wu, W. Integrity and stability of oral liposomes containing bile salts studied in simulated and ex vivo gastrointestinal media. Int. J. Pharm. 2013, 441, 693–700.
- Antimisiaris, S.G.; Marazioti, A.; Kannavou, M.; Natsaridis, E.; Gkartziou, F.; Kogkos, G.; Mourtas, S. Overcoming barriers by local drug delivery with liposomes. Adv. Drug Deliv. Rev. 2021, 174, 53–86.
- Barea, M.J.; Jenkins, M.J.; Gaber, M.H.; Bridson, R.H. Evaluation of liposomes coated with a pH responsive polymer. Int. J. Pharm. 2010, 402, 89–94.
- Hosny, K.M.; Ahmed, O.A.A.; Al-Abdali, R.T. Enteric-coated alendronate sodium nanoliposomes: A novel formula to overcome barriers for the treatment of osteoporosis. Expert Opin. Drug Deliv. 2013, 10, 741–746.
- Kazakov, S. Liposome-nanogel structures for future pharmaceutical applications: An updated review. Curr. Pharm. Des. 2016, 22, 1391–1413.
- Klemetsrud, T.; Jonassen, H.; Hiorth, M.; Kjøniksen, A.-L.; Smistad, G. Studies on pectin-coated liposomes and their interaction with mucin. Colloids Surf. B. Biointerfaces 2013, 103, 158–165.
- Parmentier, J.; Hofhaus, G.; Thomas, S.; Cuesta, L.C.; Gropp, F.; Schröder, R.; Hartmann, K.; Fricker, G.J. Improved oral bioavailability of human growth hormone by a combination of liposomes containing bio-enhancers and tetraether lipids and omeprazole. Pharm. Sci. 2014, 103, 3985–3993.
- Pons, M.; Lizondo, M.; Gallardo, M.J. Enrofloxacin loaded liposomes obtained by high speed dispersion method. Chem. Pharm. Bull. 1995, 43, 983–987.
- Schneider, T.; Sachse, A.; Röbling, G.; Brandl, M. Large-scale production of liposomes of defined size by a new continuous high pressure extrusion device. Drug Dev. Ind. Pharm. 1994, 20, 2787–2807.
- Shi, M.; Loftus, H.; McAinch, A.J.; Su, X.Q. Blueberry as a source of bioactive compounds for the treatment of obesity, type 2 diabetes and chronic inflammation. J. Funct. Foods 2017, 30, 16–29.
- Amjadi, S.; Hamishehkar, H.; Ghorbani, M. A novel smart PEGylated gelatin nanoparticle for co-delivery of doxorubicin and betanin: A strategy for enhancing the therapeutic efficacy of chemotherapy. Mater. Sci. Eng. C 2019, 97, 833–841.
- Dhananjayan, I.; Kathiroli, S.; Subramani, S.; Veerasamy, V. Ameliorating effect of betanin, a natural chromoalkaloid by modulating hepatic carbohydrate metabolic enzyme activities and glycogen content in streptozotocin-nicotinamide induced experimental rats. Biomed. Pharmacother. 2017, 88, 1069–1079.
- Tan, D.; Wang, Y.; Bai, B.; Yang, X.; Han, J. Betanin attenuates oxidative stress and inflammatory reaction in kidney of paraquat-treated rat. Food Chem. Toxicol. 2015, 78, 141–146.
- Amjadi, S.; Ghorbani, M.; Hamishehkar, H.; Roufegarinejad, L. Improvement in the stability of betanin by liposomal nanocarriers: Its application in gummy candy as a food model. Food Chem. 2018, 256, 156–162.
- Khan, M.I. Stabilization of betalains: A review. Food Chem. 2016, 197, 1280–1285.
- Selig, M.J.; Celli, G.B.; Tan, C.; La, E.; Mills, E.; Webley, A.-D.; Padilla-Zakour, O.I.; Abbaspourrad, A. High pressure processing of beet extract complexed with anionic polysaccharides enhances red color thermal stability at low pH. Food Hydrocoll. 2018, 80, 292–297.
- Amjadi, S.; Abbasi, M.M.; Shokouhi, B.; Ghorbani, M.; Hamishehkar, H.J. Enhancement of therapeutic efficacy of betanin for diabetes treatment by liposomal nanocarriers. Funct. Foods. 2019, 59, 119–128.
- Bulboacă, A.E.; Porfire, A.S.; Tefas, L.R.; Boarescu, P.M.; Bolboacă, S.D.; Stănescu, I.C.; Bulboacă, A.C.; Dogaru, G. Liposomal curcumin is better than curcumin to alleviate complications in experimental diabetic mellitus. Molecules 2019, 24, 846.
- Kadoglou, N.P.; Daskalopoulou, S.S.; Perrea, D.; Liapis, C.D. Matrix metalloproteinases and diabetic vascular complications. Angiology 2005, 56, 173–189.
- Singh, D.; Srivastava, S.K.; Chaudhuri, T.K.; Upadhyay, G. Multifaceted role of matrix metalloproteinases (MMPs). Front. Mol. Biosci. 2015, 2, 19.
- Gauttam, V.K.; Kalia, A.N. Development of polyherbal antidiabetic formulation encapsulated in the phospholipids vesicle system. J. Adv. Pharm. Technol. Res. 2013, 4, 108–117.
- Sharma, P.K.; Saxena, P.; Jaswanth, A.; Balasubramaniam, A.J. Anti-diabetic activity of lycopene niosomes: Experimental observation. Pharm. Drug Dev. 2017, 4, 103.
- Alam, M.S.; Ahad, A.; Abidin, L.; Aqil, M.; Mir, S.R.; Mujeeb, M. Embelin-loaded oral niosomes ameliorate streptozotocin-induced diabetes in Wistar rats. Biomed. Pharmacother. 2018, 97, 1514–1520.
- Kamble, B.; Talreja, S.; Gupta, A.; Patil, D.; Pathak, D.; Moothedath, I.; Duraiswamy, B. Development and biological evaluation of Gymnema sylvestre extract-loaded nonionic surfactant-based niosomes. Nanomedicine 2012, 8, 1295–1305.
- Sechi, M.; Syed, D.N.; Pala, N.; Mariani, A.; Marceddu, S.; Brunetti, A.; Mukhtar, H.; Sanna, V. Nanoencapsulation of dietary flavonoid fisetin: Formulation and in vitro antioxidant and α-glucosidase inhibition activities. Mater. Sci. Eng. C 2016, 68, 594–602.
- Lammari, N.; Froiio, F.; Louaer, M.; Cristiano, M.C.; Bensouici, C.; Paolino, D.; Louaer, O.; Meniai, A.H.; Elaissari, A. Poly(ethyl acrylate-co-methyl Methacrylate-co-trimethylammoniethyl methacrylate chloride) (Eudragit RS100) Nanocapsules as Nanovector Carriers for Phoenix dactylifera L. Seeds Oil: A Versatile Antidiabetic Agent. Biomacromolecules 2020, 21, 4442–4456.
- Chauhan, P.; Tamrakar, A.K.; Mahajan, S.; Prasad, G.B.K.S. Chitosan encapsulated nanocurcumin induces GLUT-4 translocation and exhibits enhanced anti-hyperglycemic function. Life Sci. 2018, 213, 226–235.
- Maity, S.; Mukhopadhyay, P.; Kundu, P.P.; Chakraborti, A.S. Alginate coated chitosan core-shell nanoparticles for efficient oral delivery of naringenin in diabetic animals—An in vitro and in vivo approach. Carbohydr. Polym. 2017, 170, 124–132.
- Mukhopadhyay, P.; Maity, S.; Mandal, S.; Chakraborti, A.S.; Prajapati, A.K.; Kundu, P.P. Preparation, characterization and in vivo evaluation of pH sensitive, safe quercetin-succinylated chitosan-alginate core-shell-corona nanoparticle for diabetes treatment. Carbohydr. Polym. 2018, 182, 42–51.
- Rani, R.; Dahiya, S.; Dhingra, D.; Dilbaghi, N.; Kim, K.-H.; Kumar, S. Evaluation of anti-diabetic activity of glycyrrhizin-loaded nanoparticles in nicotinamide-streptozotocin-induced diabetic rats. Eur. J. Pharm. Sci. 2017, 106, 220–230.
- Panwar, R.; Raghuwanshi, N.; Srivastava, A.K.; Sharma, A.K.; Pruthi, V. In-vivo sustained release of nanoencapsulated ferulic acid and its impact in induced diabetes. Mater. Sci. Eng. C 2018, 92, 381–392.
- Rani, R.; Dahiya, S.; Dhingra, D.; Dilbaghi, N.; Kaushik, A.; Kim, K.-H.; Kumar, S. Antidiabetic activity enhancement in streptozotocin+ nicotinamide–induced diabetic rats through combinational polymeric nanoformulation. Int. J. Nanomed. 2019, 14, 4383–4395.
- Rani, R.; Dahiya, S.; Dhingra, D.; Dilbaghi, N.; Kim, K.-H.; Kumar, S. Improvement of antihyperglycemic activity of nano-thymoquinone in rat model of type-2 diabetes. Chem. Biol. Interact. 2018, 295, 119–132.
- Chitkara, D.; Nikalje, S.; Mittal, A.; Chand, M.; Kumar, N. Development of quercetin nanoformulation and in vivo evaluation using streptozotocin induced diabetic rat model. Drug Deliv. Transl. Res. 2012, 2, 112–123.
- Roy, M.; Pal, R.; Chakraborti, A.S. Pelargonidin-PLGA nanoparticles: Fabrication, characterization, and their effect on streptozotocin induced diabetic rats1. Indian J. Exp. Biol. 2017, 55, 819–830.
- Das, S.; Roy, P.; Pal, R.; Auddy, R.G.; Chakraborti, A.S.; Mukherjee, A. Engineered silybin nanoparticles educe efficient control in experimental diabetes. PLoS ONE 2014, 9, e101818.
- Rashid, M.H.A.; Bharadwaj, P.V.P.D.; Mandal, V.; Pal, M.; Mandal, S.C.; Thandavarayan, R.A. Preparation and characterization of PLGA loaded nanoparticles obtained from D. melanoxylon Roxb. leaves for their antiproliferative and antidiabetic activity. Int. J. Green Pharm. 2017, 11, S438–S447.
- Mostafa, D.M.; Abd El-Alim, S.H.; Asfour, M.H.; Al-Okbi, S.Y.; Mohamed, D.A.; Awad, G. Transdermal nanoemulsions of Foeniculum vulgare Mill. essential oil: Preparation, characterization and evaluation of antidiabetic potential. J. Drug Deliv. Sci. Technol. 2015, 29, 99–106.
- Jumaryatno, P.; Chabib, L.; Hayati, F.; Awaluddin, R.J. Stability study of ipomoea reptans extract self-nanoemulsifying drug delivery system (SNEDDS) as anti-diabetic therapy. Appl. Pharm. Sci. 2018, 8, 11–14.
- Mohseni, R.; ArabSadeghabadi, Z.; Ziamajidi, N.; Abbasalipourkabir, R.; RezaeiFarimani, A. Oral administration of resveratrol-loaded solid lipid nanoparticle improves insulin resistance through targeting expression of SNARE proteins in adipose and muscle tissue in rats with type 2 diabetes. Nanoscale Res. Lett. 2019, 14, 227.
- Ahangarpour, A.; Oroojan, A.A.; Khorsandi, L.; Kouchak, M.; Badavi, M. Solid lipid nanoparticles of myricitrin have antioxidant and antidiabetic effects on streptozotocin-nicotinamide-induced diabetic model and myotube cell of male mouse. Oxid. Med. Cell. Longev. 2018, 2018, 7496936.
- Xue, M.; Yang, M.; Zhang, W.; Li, X.; Gao, D.; Ou, Z.; Li, Z.; Liu, S.; Li, X.; Yang, S. Characterization, pharmacokinetics, and hypoglycemic effect of berberine loaded solid lipid nanoparticles. Int. J. Nanomed. 2013, 8, 4677–4687.
- Shi, F.; Wei, Z.; Zhao, Y.; Xu, X. Nanostructured lipid carriers loaded with baicalin: An efficient carrier for enhanced antidiabetic effects. Pharm. Mag. 2016, 12, 198–202.
- Yeo, P.L.; Lim, C.L.; Chye, S.M.; Ling, A.P.K.; Koh, R.Y. Niosomes: A review of their structure, properties, methods of preparation, and medical applications. Asian Biomed. 2018, 11, 301–314.
- Chen, S.; Hanning, S.; Falconer, J.; Locke, M.; Wen, J. Recent advances in non-ionic surfactant vesicles (niosomes): Fabrication, characterization, pharmaceutical and cosmetic applications. Eur. J. Pharm. Biopharm. 2019, 144, 18–39.
- Sharma, R.; Dua, J.S.; Prasad, D.N.; Hira, S.; Monika. Advancement in novel drug delivery system: Niosomes. J. Drug Deliv. Ther. 2019, 9, 995–1001.
- El-Mahdy, M.M.; Hassan, A.S.; El-Badry, M.; El-Gindy, G.E.-D.A. Performance of curcumin in nanosized carriers niosomes and ethosomes as potential anti-inflammatory delivery system for topical application. Bull. Pharm. Sci. 2020, 43, 105–122.
- Ge, X.; Wei, M.; He, S.; Yuan, W.-E. Advances of non-ionic surfactant vesicles (niosomes) and their application in drug delivery. Pharmaceutics 2019, 11, 55.
- Kazi, K.M.; Mandal, A.S.; Biswas, N.; Guha, A.; Chatterjee, S.; Behera, M.; Kuotsu, K. Niosome: A future of targeted drug delivery systems. J. Adv. Pharm. Technol. Res. 2010, 1, 374–380.
- Reddy, B.S.; Padman, J.S.C.; Santosh, V. Niosomes as nanocarrier systems: A review. Int. J. Pharm. Sci. Res. 2012, 3, 1560.
- Abdelkader, H.; Alani, A.W.G.; Alany, R.G. Recent advances in non-ionic surfactant vesicles (niosomes): Self-assembly, fabrication, characterization, drug delivery applications and limitations. Drug Deliv. 2014, 21, 87–100.
- Khan, R.; Irchhaiya, R. Niosomes: A potential tool for novel drug delivery. Int. J. Pharm. Investig. 2016, 46, 195–204.
- Marianecci, C.; Di Marzio, L.; Rinaldi, F.; Celia, C.; Paolino, D.; Alhaique, F.; Esposito, S.; Carafa, M. Niosomes from 80s to present: The state of the art. Adv. Colloid Interface Sci. 2014, 205, 187–206.
- Rao, A.V.; Rao, L. Lycopene and human health. Curr. Top. Nutraceutical Res. 2004, 2, 127–136.
- Lee, M.T.; Chen, B.H. Stability of lycopene during heating and illumination in a model system. Food Chem. 2002, 78, 425–432.
- Pesek, C.A.; Warthesen, J.J. Photodegradation of carotenoids in a vegetable juice system. J. Food Sci. 1987, 52, 744–746.
- Durg, S.; Kumar, B.N.; Vandal, R.; Dhadde, S.B.; Thippeswamy, B.S.; Veerapur, V.P.; Badami, S. Antipsychotic activity of embelin isolated from Embelia ribes: A preliminary study. Biomed. Pharm. 2017, 90, 328–331.
- Rachh, P.R.; Rachh, M.R.; Ghadiya, N.R.; Modi, D.C.; Modi, K.P.; Patel, N.M.; Rupareliya, M.T. Antihyperlipidemic activity of Gymenma sylvestre R. Br. leaf extract on rats fed with high cholesterol diet. Int. J. Pharmacol. 2010, 6, 138–141.
- Nakamura, Y.; Tsumura, Y.; Tonogai, Y.; Shibata, T. Fecal steroid excretion is increased in rats by oral administration of gymnemic acids contained in Gymnema sylvestre leaves. J. Nutr. 1999, 129, 1214–1222.
- Barani, M.; Hajinezhad, M.R.; Sargazi, S.; Rahdar, A.; Shahraki, S.; Lohrasbi-Nejad, A.; Baino, F.J. In vitro and in vivo anticancer effect of pH-responsive paclitaxel-loaded niosomes. Mater. Sci. Mater. Med. 2021, 32, 147.
- Nazari, V.M.; Mahmood, S.; Shah, A.M.; Al-Suede, F.S.R. Suppression of melanoma growth in a murine tumour model using orthosiphon stamineus benth. Extract loaded in ethanolic phospholipid vesicles (spherosome). Curr. Drug Metab. 2022, 23, 317–328.
- Akbarzadeh, I.; Yaraki, M.T.; Ahmadi, S.; Chiani, M.; Nourouzian, D. Folic acid-functionalized niosomal nanoparticles for selective dual-drug delivery into breast cancer cells: An in-vitro investigation. Adv. Powder Technol. 2020, 31, 4064–4071.
- Sivaramakrishna, D.; Prasad, M.D.; Swamy, M.J. A homologous series of apoptosis-inducing N-acylserinols: Thermotropic phase behavior, interaction with cholesterol and characterization of cationic N-myristoylserinol-cholesterol-CTAB niosomes. Biochim. Biophys. Acta Biomembr. 2019, 1861, 504–513.
