Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
It has been argued that effective action towards addressing a complex concern such as suicide requires a combination of evidence-based strategies. While these complex public health approaches have recently gained importance, little is known about their characteristics and what contributes to their complexity.
- complex interventions
- suicide research
- suicide prevention
- multilevel
- implementation
- definitions
1. Introduction
Suicidal behavior is complex and determined by several intertwined factors. Contributions of individual as well as population level risk factors highlight the heterogeneity in its etiology. These risk factors further vary in strength and patterns of association across gender, age, culture, location, and individual history [1]. There is now an emerging evidence base for a range of interventions to prevent as well as treat suicidal behavior. For example, it has been found that interventions such as training primary care physicians in depression recognition and treatment, educating youths on depression and suicidal behavior, as well as active outreach to psychiatric patients after discharge help prevent suicide [2]. The effectiveness of interventions across a spectrum of universal, selective, and indicated interventions is variable [2], with each intervention holding its relevance and importance across different contexts. However, the heterogeneity in suicidal behavior makes it difficult to develop an all-encompassing model of suicide risk or a single prevention and/or intervention pathway [1].
It has been acknowledged that no single strategy stands above others in addressing such a complex multifaceted concern [3]. Instead, there is strong support for a broader public health approach that seeks to tap into synergies between various evidence-based strategies to simultaneously address a range of risk factors for greater impact [2][3][4][5]. This public health approach is necessarily population-based, and prevention-focused, involving multiple avenues and levels of prevention [6]. Within the realm of suicide prevention research, there has been recent attention on suicide prevention strategies that simultaneously implement multiple forms of evidence-based interventions. Evidence related to the effectiveness of such approaches has emerged from high-income countries across the world [7][8][9]. In a systematic review and meta-analysis, Hofstra et al. [10] found that multilevel interventions were more effective than single-level interventions and, further, that effect sizes were significantly higher with the number of levels involved.
2. The Complexity in Defining Complex Interventions
A public health intervention can be defined as any action or program intended to deliver a net benefit to the community as well as individuals [11]. To address suicidal behavior, a public health intervention should involve actions targeted at different communities. These can include a range of interventions such as programs (e.g., cognitive behavior therapy), practices (e.g., training of primary care physicians), procedures (e.g., screening for depression), policies (e.g., restriction of access to means), principles (e.g., prevention before treatment), and products (e.g., self-help applications), as well as medication [12]. Characteristics such as the setting of the intervention, the target of change, resources used, and the agent of change can be used to describe different kinds of interventions [13]. McLeroy and colleagues [13] also distinguish between the level—the position in the social ecology (individual, health care system, community) and target—and the entity of focus of interventions. This is to further suggest that they may be implemented at one level but target multiple levels of behaviors/communities/systems. This forms an important premise to understand complex interventions and the intricacies surrounding its definition.
Defining complex interventions is somewhat challenging. While the term intervention is relatively easy to define as intentional actions to improve health outcomes, the term complex is harder to define. One approach could be to define what it is not—that is, a simple intervention. However, this too is not clear-cut. For instance, distributing pamphlets with information on suicide helplines and support services to a community of youth may at first sound like a simple intervention. Even though the messaging may be consistent, different youth may perceive it differently and pamphlets may not reach or be accessible to all kinds of youth if diversity is not taken into consideration. Furthermore, pamphlets may not be adequate and acceptable for a population reliant on digital media and/or populations with low literacy. Implementing this intervention in real-life settings is hardly simple. A simple intervention may have unintended ramifications due to inherent complexities in its implementation, the context, or the way it is perceived. Thomas and colleagues [14] argue that interventions as such cannot be simple because when implemented in real life, researchers need to consider one or more aspects of complexity in its design and implementation. Hence, they refer to intervention complexity rather than complex intervention.
In real life, interventions do not fit into either/or, simple, or complex categories. It has been argued that the way an intervention is defined depends on its characteristics, the research questions involved, and the complexity of analysis and impact [15]. According to this logic, all interventions can be either complex or simple depending on the pragmatic perspective adopted by the researcher to better understand the intervention in question. Characteristics of simplicity and complexity have also been conceived as existing on a spectrum [16].
Despite these difficulties, there have been attempts to define complex interventions. Richards et al. [17] present an overview of definitions based on different characteristics of complexity—the intervention components, implementation, evaluation complexity, and the context. From the perspective of intervention components, complex interventions have been described as comprising multiple components with a unique, complex, and interacting relationship [18]. Anderson et al. [19] argue for the application of a more precise and consistent language to distinguish between conceptually distinct characteristics of complexity. This includes considering the intervention and its characteristics, the varying characteristics of the implementation process, variant properties of the setting or the context, and the variant characteristics of the participant responses. Skivington et al. [20] contend that:
An intervention might be considered complex because of properties of the intervention itself, such as the number of components involved; the range of behaviours targeted; expertise and skills required by those delivering and receiving the intervention; the number of groups, settings, or levels targeted; or the permitted level of flexibility of the intervention or its components (p. 2).
Another view of complexity focuses on the role of complex adaptive systems and not the characteristics of the intervention per se [21]. A complex adaptive system involves an interplay between agents such as professionals, consumers, and organizational systems. The interaction between these agents following simple rules further gives rise to a complex system that is continually adapting to sustain itself [22]. Paradoxically, due to the continually evolving interaction between these agents in the system, it can never be fully resolved or understood [23].
Historically, there has been a tension between developing a better understanding of complex interventions and the perils of over-defining them. Complex interventions are difficult to define considering the active and moving components of the intervention and their unique ways of interacting with one another [16]. There is fluidity, such that it is difficult to arrive at its exact definition. One approach is to break down the intervention into its constituent components to better understand what it comprises [20]. However, such an approach can lead to “an irretrievable loss of what the complex system used to be” [24] (p. 1561) and an oversimplification of what the intervention does to the system. A complex intervention is hence argued to be more than the sum of its parts [24].
While the fluidity and complexity of real-world interventions embraces diverse characteristics, it also creates challenges for suicide prevention researchers, particularly around terminology. Frequently the term complex is used in a haphazard way to ambiguously to describe interventions. However, it is not always clear (and indeed it is unlikely) whether the same meaning is consistently used and applied across the literature. More specifically, complexity is more often used to describe interventions as complicated, difficult to do and unclear which are different concepts [21]. As a result, several terms and definitions are used to denote complex interventions. There is a need for the field to address this confusion and uncertainty around interrelated terms.
3. Terms and Definitions
Several interchangeable terms have been used in the literature to connote complex interventions. Some of these commonly found interrelated terms are multilevel, multicomponent, systems approach, community-based, multimodal, and integrated interventions.
A characteristic feature of complex interventions is its multilevel approach. Complex and multilevel are two terms that are often used synonymously to describe interventions with a socio-ecological lens or approach. Such an approach looks at human behavior as influenced by various levels within an ecosystem [25]. The approach provides a multilevel conceptualization of the determinants of health and human behavior. Each layer of the ecosystem has multiple actors (such as the individual, healthcare, workplace, school, laws, policies, etc.), which then become targets and/or key actors in the delivery of an intervention. Such interventions aim to create change at different levels—individual and community levels, based on the assumption that the linkage between interventions will create a compounded effect on individual behavior [26]. Hence, such an approach leverages the bidirectionality of relationships between systems. Multilevel interventions have also been defined by Trickett and Beehler [27] as: “… interventions with multiple components designed to affect factors in two or more levels of the local ecology that contribute to wellness and illness, with the goal of effecting changes within and between different levels” (p. 2).
In suicide research, two other approaches have been used [28] to define a multilevel approach. The first is the staged traditional prevention approach which comprises three levels: primary (to prevent onset), secondary (to detect and treat), and tertiary (to reduce relapses and recurrence) [29]. The second is a more recent suicide prevention-specific approach, which focuses on the effectiveness of interventions [2][3][4]. Effective interventions are aligned with suicide risk factors and classified into three levels of prevention—universal (for the whole population), selective (aimed at high-risk groups), and indicated (focused on high-risk individuals with history) [30][31]. In this context, a multilevel intervention would involve strategies at different levels of prevention, involving the general population or specific sub-groups and individuals.
Similarly, the systems approach is based on the understanding that everything is interrelated and interdependent. The system can be any cohesive group—a school, community, healthcare setting, family, etc.—which comprises different components or parts. These parts are interdependent, comprise multiple feedback processes and interconnections, and incorporate multiple perspectives [32]. A systemic intervention or one that employs a systems approach involves a purposeful action or an intervention to create change in cognizance with the interdependencies of a system [33]. Hence, such an approach involves multiple levels and targets. In the context of suicide prevention, a systems-based approach has often referred to the implementation of multifaceted interventions, simultaneously within a region [34].
To add further to the complexity, another commonly used term to denote complexity is multicomponent. Public health interventions can vary according to the type and scale of action. Some consist of single strategies and others consist of a combination of strategies or components for population impact on health. As the name suggests, multicomponent interventions comprise different components, targeted at the same level or multiple levels of a system. In practice, it is difficult to clearly delineate the intervention units or components within an intervention [35]. This further makes the definition of multicomponent problematic. A few scholars have attempted to address this challenge by operationalizing the term components—those that play a functional role in the theorized change process [36]; those that are theoretically important to the intervention [37]; and active ingredients [38]. Others such as Hawe [36] contend that the functional role of components within an intervention and how they create the intended effect is more important to define than just characteristic features of the component itself. For example, if a component is a suicide awareness media campaign, it is more important to describe how the campaign works and contributes to change rather than what the campaign is, per se.
The term community-based is also used to imply complexity and has a wide range of meanings [13]. It often refers to the setting in which interventions are implemented. Such interventions may be implemented in a variety of community settings such as schools, health care facilities, neighborhoods, organizations, and other settings. For instance, school-based universal prevention program for suicide could be called a community-based intervention. Such interventions may also target community change, in creating health community environments through systemic change. For instance, the Zero Suicide Framework [39] aims to reform healthcare settings and hence uses the healthcare community as the target of change. Community-based interventions may also use communities as a resource in terms of building community ownership and partnership. For instance, working with the media to spread awareness about depression and suicide. Closely linked to this idea, is the use of the community as an agent. This involves leveraging the existing capacities of communities for change. An example is gatekeeper training with community stakeholders to enhance their capacity to identify those at risk of suicide. Principles of equity, participation, and collaboration to build community capacity and accomplish community-level change is a complex endeavor.
Other less commonly used terms to denote complexity are multimodal and integrated. These terms carry many connotations. While a multimodal intervention is one that is characterized by different modes of activity or occurrence, integrated interventions refer to linkage and intersectoral collaborations.
By their very definition, the terms represent distinct yet overlapping aspects or characteristics of a complex intervention. Some interactions between these terms have been noted in the literature. For instance, the Medical Research Council’s [40] framework for the design and evaluation of complex interventions suggests that multiple components are the building blocks of a complex intervention, which are interacting and impact multiple levels of an ecosystem. Terms such as multilevel, multicomponent, multimodal, systemic, community-based, multimodal, and integrated interventions can be understood to be different characteristic types of complex interventions. Complex intervention can, hence, be defined as an umbrella term encompassing all these characteristics, among many others as can be seen in Figure 1.
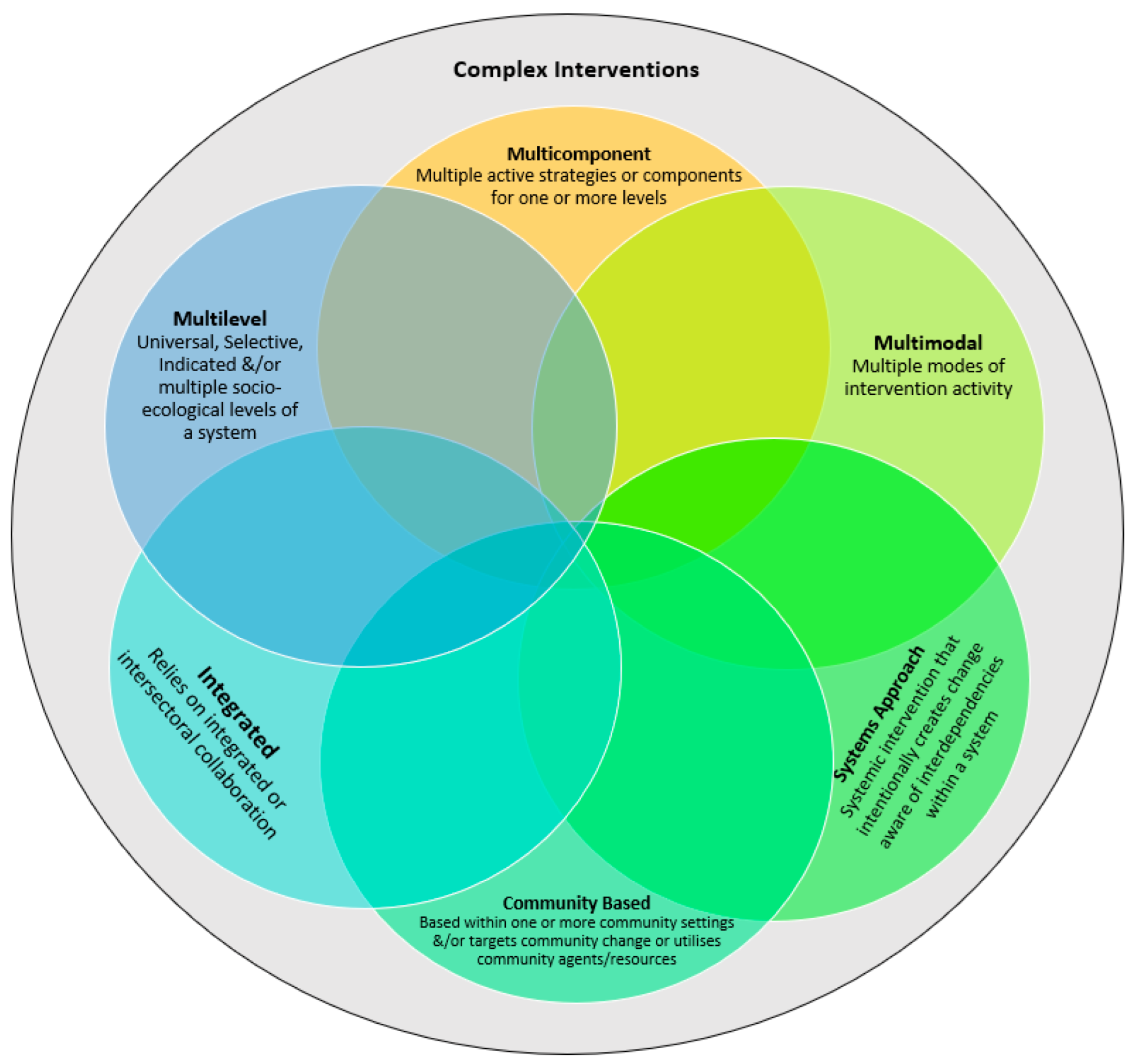
Figure 1. Characteristics of complex interventions.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph19148591
References
- Turecki, G.; Brent, D.A. Suicide and Suicidal Behaviour. Lancet 2016, 387, 1227–1239.
- Mann, J.J.; Michel, C.A.; Auerbach, R.P. Improving Suicide Prevention through Evidence-Based Strategies: A Systematic Review. Am. J. Psychiatry 2021, 178, 611–624.
- Zalsman, G.; Hawton, K.; Wasserman, D.; van Heeringen, K.; Arensman, E.; Sarchiapone, M.; Carli, V.; Höschl, C.; Barzilay, R.; Balazs, J.; et al. Suicide Prevention Strategies Revisited: 10-Year Systematic Review. Lancet Psychiatry 2016, 3, 646–659.
- Van der Feltz-Cornelis, C.M.; Sarchiapone, M.; Postuvan, V.; Volker, D.; Roskar, S.; Grum, A.T.; Carli, V.; McDaid, D.; O’Connor, R.; Maxwell, M.; et al. Best Practice Elements of Multilevel Suicide Prevention Strategies. Crisis 2011, 32, 319–333.
- Krysinska, K.; Batterham, P.J.; Tye, M.; Shand, F.; Calear, A.L.; Cockayne, N.; Christensen, H. Best Strategies for Reducing the Suicide Rate in Australia. Aust. N. Z. J. Psychiatry 2016, 50, 115–118.
- Yip, P.S.F.; Tang, L. Public Health Approach to Suicide Research. In Advancing Suicide Research; Kõllves, K., Sisask, M., Värnik, P., Värnik, A., Leo, D.D., Eds.; Hogrefe Publishing: Gottingen, Germany, 2021.
- Hegerl, U.; Wittmann, M.; Arensman, E.; van Audenhove, C.; Bouleau, J.-H.; van der Feltz-Cornelis, C.; Gusmao, R.; Kopp, M.; Löhr, C.; Maxwell, M.; et al. The ‘European Alliance Against Depression (EAAD)’: A Multifaceted, Community-Based Action Programme against Depression and Suicidality. World J. Biol. Psychiatry 2008, 9, 51–58.
- Knox, K.L.; Pflanz, S.; Talcott, G.W.; Campise, R.L.; Lavigne, J.E.; Bajorska, A.; Tu, X.; Caine, E.D. The US Air Force Suicide Prevention Program: Implications for Public Health Policy. Am. J. Public Health 2010, 100, 2457–2463.
- Motohashi, Y.; Kaneko, Y.; Sasaki, H.; Yamaji, M. A Decrease in Suicide Rates in Japanese Rural Towns after Community-Based Intervention by the Health Promotion Approach. Suicide Life-Threat. Behav. 2007, 37, 593–599.
- Hofstra, E.; van Nieuwenhuizen, C.; Bakker, M.; Özgül, D.; Elfeddali, I.; de Jong, S.J.; van der Feltz-Cornelis, C.M. Effectiveness of Suicide Prevention Interventions: A Systematic Review and Meta-Analysis. Gen. Hosp. Psychiatry 2020, 63, 127–140.
- Rychetnik, L.; Hawe, P.; Waters, E.; Barratt, A.; Frommer, M. A Glossary for Evidence Based Public Health. J. Epidemiol. Community Health 2004, 58, 538–545.
- Brown, C.H.; Curran, G.; Palinkas, L.A.; Aarons, G.A.; Wells, K.B.; Jones, L.; Collins, L.M.; Duan, N.; Mittman, B.S.; Wallace, A.; et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu. Rev. Public Health 2017, 38, 1–22.
- McLeroy, K.R.; Norton, B.L.; Kegler, M.C.; Burdine, J.N.; Sumaya, C.V. Community-Based Interventions. Am. J. Public Health 2003, 93, 529–533.
- Thomas, J.; Petticrew, M.; Noyes, J.; Chandler, J.; Rehfuess, E.; Tugwell, P.; Welch, V.A. Chapter 17: Intervention complexity. In Cochrane Handbook for Systematic Reviews of Interventions; Version 6.3; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 8 May 2022).
- Petticrew, M. When Are Complex Interventions “Complex”? When Are Simple Interventions “Simple”? Eur. J. Public Health 2011, 21, 397–398.
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. BMJ 2008, 337, a1655.
- Richards, D.A. The Complex Interventions Framework. In Complex Interventions in Health: An Overview of Research Methods; Richards, D.A., Hallberg, I.R., Eds.; Taylor & Francis Group: Abingdon, UK, 2015; p. 15.
- Rabin, B.A.; Brownson, R.C. Terminology for Dissemination and Implementation Research. In Dissemination and Implementation Research in Health: Translating Science to Practice; Brownson, R.C., Colditz, G.A., Proctor, E.K., Eds.; Oxford University Press: New York, NY, USA, 2017.
- Anderson, L.M.; Petticrew, M.; Chandler, J.; Grimshaw, J.; Tugwell, P.; O’Neill, J.; Welch, V.; Squires, J.; Churchill, R.; Shemilt, I. Introducing a Series of Methodological Articles on Considering Complexity in Systematic Reviews of Interventions. J. Clin. Epidemiol. 2013, 66, 1205–1208.
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A New Framework for Developing and Evaluating Complex Interventions: Update of Medical Research Council Guidance. BMJ 2021, 374, n2061.
- Shiell, A.; Hawe, P.; Gold, L. Complex Interventions or Complex Systems? Implications for Health Economic Evaluation. BMJ 2008, 336, 1281–1283.
- Braithwaite, J.; Churruca, K.; Long, J.C.; Ellis, L.A.; Herkes, J. When Complexity Science Meets Implementation Science: A Theoretical and Empirical Analysis of Systems Change. BMC Med. 2018, 16, 63.
- Plsek, P.E.; Greenhalgh, T. The Challenge of Complexity in Health Care. BMJ 2001, 323, 625–628.
- Hawe, P.; Shiell, A.; Riley, T. Complex Interventions: How “out of Control” Can a Randomised Controlled Trial Be? BMJ 2004, 328, 1561–1563.
- Bronfenbrenner, U. Toward an Experimental Ecology of Human Development. Am. Psychol. 1977, 32, 513–531.
- Schölmerich, V.L.N.; Kawachi, I. Translating the Socio-Ecological Perspective into Multilevel Interventions: Gaps between Theory and Practice. Health Educ. Behav. 2016, 43, 17–20.
- Trickett, E.J.; Beehler, S. The Ecology of Multilevel Interventions to Reduce Social Inequalities in Health. Am. Behav. Sci. 2013, 57, 1227–1246.
- Sakashita, T.; Oyama, H. Developing a Hypothetical Model for Suicide Progression in Older Adults with Universal, Selective, and Indicated Prevention Strategies. Front. Psychiatry 2019, 10, 161.
- Simeonsson, R.J. Primary, Secondary, and Tertiary Prevention in Early Intervention. J. Early Interv. 1991, 15, 124–134.
- Silverman, M.; Felner, R. Suicide prevention programs: Issues of design, implementation, feasibility, and developmental appropriateness. Suicide Life Threat. Behav. 1995, 25, 92–104.
- Silverman, M.; Maris, R. The prevention of suicidal behaviors: An overview. Suicide Life Threat. Behav. 1995, 25, 10–21.
- Arnold, R.D.; Wade, J.P. A Definition of Systems Thinking: A Systems Approach. Procedia Comput. Sci. 2015, 44, 669–678.
- Midgley, G. Systemic Intervention for Public Health. Am. J. Public Health 2006, 96, 466–472.
- Baker, S.T.; Nicholas, J.; Shand, F.; Green, R.; Christensen, H. A Comparison of Multi-Component Systems Approaches to Suicide Prevention. Australas Psychiatry 2018, 26, 128–131.
- Fortune, N.; Madden, R.; Riley, T.; Short, S. The International Classification of Health Interventions: An ‘Epistemic Hub’ for Use in Public Health. Health Promot. Int. 2021, 36, 1753–1764.
- Hawe, P. Lessons from Complex Interventions to Improve Health. Annu. Rev. Public Health 2015, 36, 307–323.
- Durlak, J.A.; DuPre, E.P. Implementation Matters: A Review of Research on the Influence of Implementation on Program Outcomes and the Factors Affecting Implementation. Am. J. Community Psychol. 2008, 41, 327.
- Brownson, R.C.; Fielding, J.E.; Maylahn, C.M. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu. Rev. Public Health 2009, 30, 175–201.
- Brodsky, B.S.; Spruch-Feiner, A.; Stanley, B. The Zero Suicide Model: Applying Evidence-Based Suicide Prevention Practices to Clinical Care. Front. Psychiatry 2018, 9, 33.
- Campbell, M.; Fitzpatrick, R.; Haines, A.; Kinmonth, A.L.; Sandercock, P.; Spiegelhalter, D.; Tyrer, P. Framework for Design and Evaluation of Complex Interventions to Improve Health. BMJ 2000, 321, 694–696.
This entry is offline, you can click here to edit this entry!
