Patent foramen ovale (PFO) is a cardiac congenital anomaly with high prevalence in the general population (20–30%) and often represents an incidental finding. PFO can be implicated in the pathogenesis of several medical conditions, so called PFO-associated syndromes, including cryptogenic thromboembolism, decompression sickness, migraine, and arterial deoxygenation syndromes. In 1975, King and Mills performed for the first time a percutaneous atrial septal defect closure in humans by using an automatically opening “umbrella-like” device, further refined to the clamshell double-umbrella device, which had the advantage of being recapturable or removable up to the end of the procedure.
- patent foramen ovale (PFO)
- transesophageal echocardiography (TEE)
1. Brief Introduction of Percutaneous Closure of Percutaneous Patent Foramen Ovale (PFO) by Traditional Devices
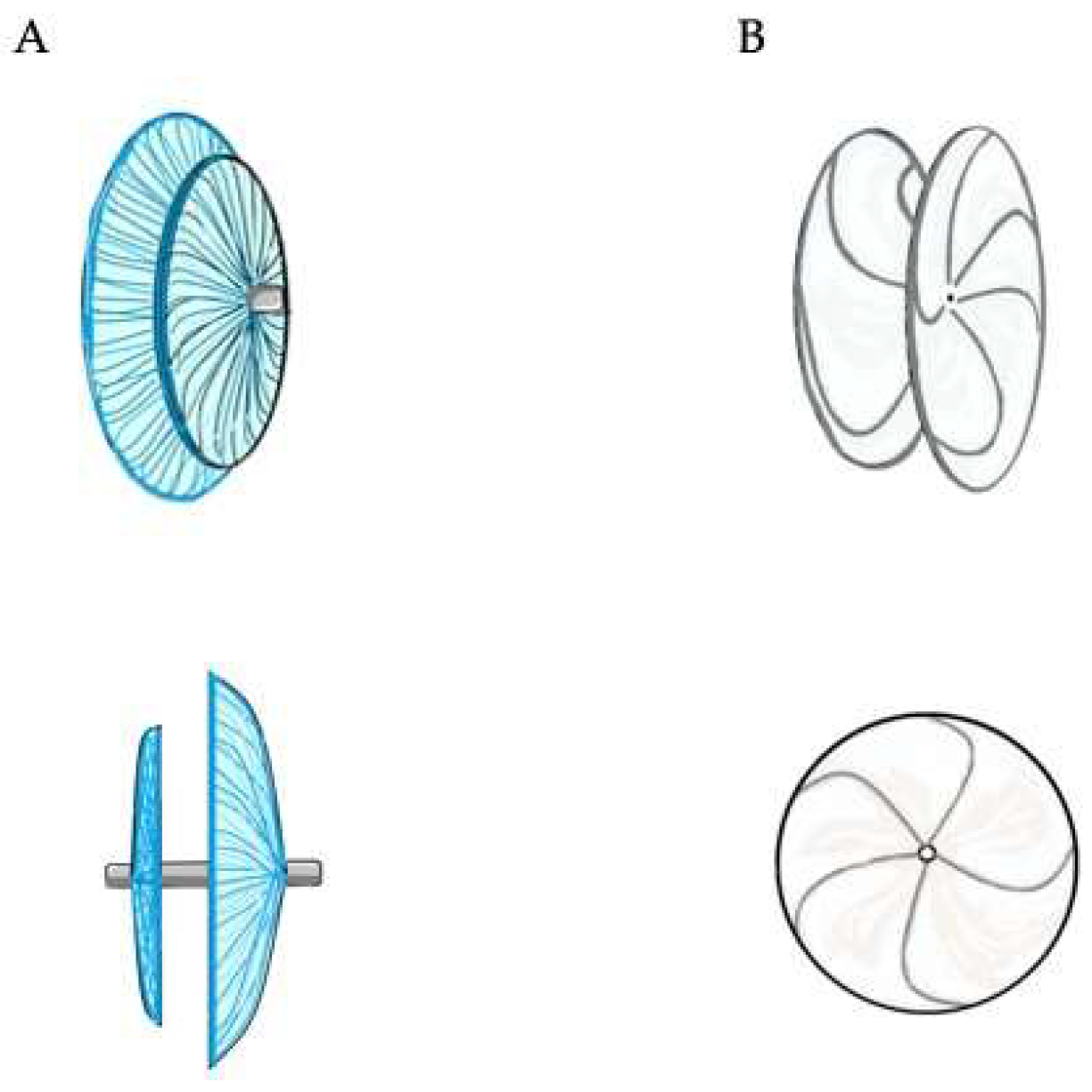
2. Double Disc Devices
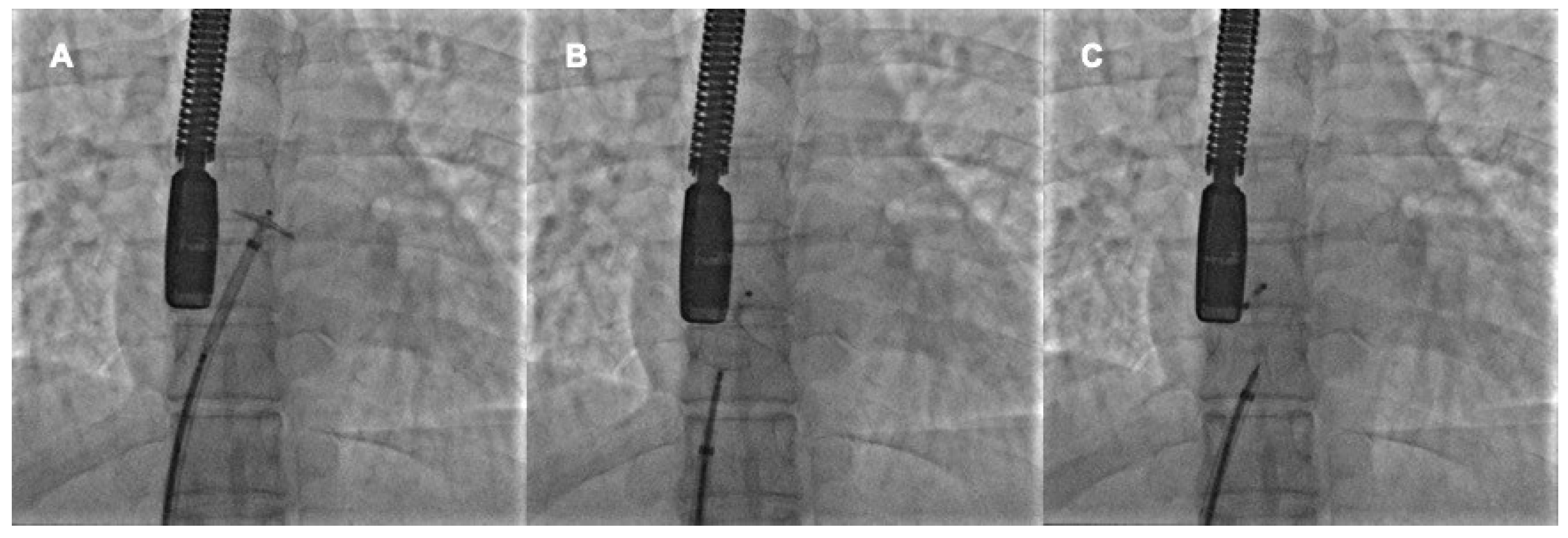
3. Procedural Steps
- -
-
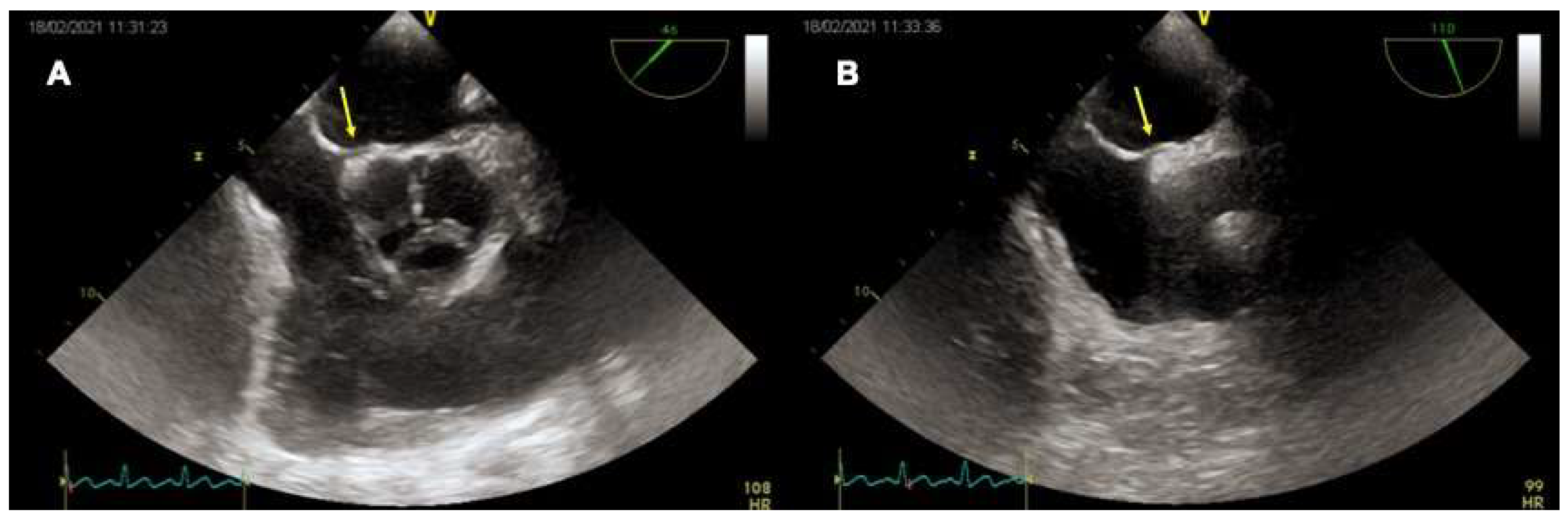
The device has well hugged the septum primum, particularly the septum secundum;
- -
-
There is no interference with the atrioventricular valves or the other intracardiac structures
- -
-
There are no patent accessory fenestrations
4. Role of TEE
4.1. TEE before PFO Closure: Characterization of the PFO and Decision Making
|
|
4.2. TEE during PFO Closure: Intra-Procedural Guidance
4.3. TEE after PFO Closure: Post-Procedural Follow-Up
4.4. Intracardiac Echocardiography
This entry is adapted from the peer-reviewed paper 10.3390/jcm11144001
References
- King, T.D. Secundum atrial septal defect. Nonoperative closure during cardiac catheterization. JAMA 1976, 235, 2506–2509.
- Bridges, N.D.; Hellenbrand, W.; Latson, L.; Filiano, J.; Newburger, J.W.; Lock, J.E. Transcatheter closure of patent foramen ovale after presumed paradoxical embolism. Circulation 1992, 86, 1902–1908.
- Sharafuddin, M.J.A.; Gu, X.; Titus, J.L.; Urness, M.; Cervera-Ceballos, J.J.; Amplatz, K. Transvenous Closure of Secundum Atrial Septal Defects. Circulation 1997, 95, 2162–2168.
- Meier, B. Closure of patent foramen ovale: Technique, pitfalls, complications, and follow up. Heart 2005, 91, 444–448.
- Meier, B. Percutaneous Closure of Patent Foramen Ovale in Cryptogenic Embolism. N. Engl. J. Med. 2013, 368, 1083–1091.
- Carroll, J.D.; Saver, J.L.; Thaler, D.E.; Smalling, R.W.; Berry, S.; MacDonald, L.A.; Marks, D.S.; Tirschwell, D.L. Closure of Patent Foramen Ovale versus Medical Therapy after Cryptogenic Stroke. N. Engl. J. Med. 2013, 368, 1092–1100.
- Stortecky, S.; da Costa, B.R.; Mattle, H.P.; Carroll, J.; Hornung, M.; Sievert, H.; Trelle, S.; Windecker, S.; Meier, B.; Jüni, P. Percutaneous closure of patent foramen ovale in patients with cryptogenic embolism: A network meta-analysis. Eur. Heart J. 2015, 36, 120–128.
- Saver, J.L.; Carroll, J.D.; Thaler, D.E.; Smalling, R.W.; MacDonald, L.A.; Marks, D.S.; Tirschwell, D.L. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N. Engl. J. Med. 2017, 377, 1022–1032.
- Søndergaard, L.; Kasner, S.E.; Rhodes, J.F.; Andersen, G.; Iversen, H.K.; Nielsen-Kudsk, J.E.; Settergren, M.; Sjöstrand, C.; Roine, R.O.; Hildick-Smith, D.; et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N. Engl. J. Med. 2017, 377, 1033–1042.
- Lee, P.H.; Song, J.-K.; Kim, J.S.; Heo, R.; Lee, S.; Kim, D.-H.; Song, J.-M.; Kang, D.-H.; Kwon, S.U.; Kang, D.-W.; et al. Cryptogenic Stroke and High-Risk Patent Foramen Ovale. J. Am. Coll. Cardiol. 2018, 71, 2335–2342.
- Mattle, H.P.; Evers, S.; Hildick-Smith, D.; Becker, W.J.; Baumgartner, H.; Chataway, J.; Gawel, M.; Göbel, H.; Heinze, A.; Horlick, E.; et al. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur. Heart J. 2016, 37, 2029–2036.
- Dowson, A.; Mullen, M.J.; Peatfield, R.; Muir, K.; Khan, A.A.; Wells, C.; Lipscombe, S.L.; Rees, T.; De Giovanni, J.V.; Morrison, W.L.; et al. Migraine Intervention With STARFlex Technology (MIST) trial: A prospective, multicenter, double-blind, sham-controlled trial to evaluate the effectiveness of patent foramen ovale closure with STARFlex septal repair implant to resolve refractory migraine headache. Circulation 2008, 117, 1397–1404.
- Furlan, A.J.; Reisman, M.; Massaro, J.; Mauri, L.; Adams, H.; Albers, G.W.; Felberg, R.; Herrmann, H.; Kar, S.; Landzberg, M.; et al. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N. Engl. J. Med. 2012, 366, 991–999.
- Tobis, J.M.; Charles, A.; Silberstein, S.D.; Sorensen, S.; Maini, B.; Horwitz, P.A.; Gurley, J.C. Percutaneous Closure of Patent Foramen Ovale in Patients With Migraine: The PREMIUM Trial. J. Am. Coll Cardiol. 2017, 70, 2766–2774.
- Slavin, L.; Tobis, J.M.; Rangarajan, K.; Dao, C.; Krivokapich, J.; Liebeskind, D.S. Five-year experience with percutaneous closure of patent foramen ovale. Am. J. Cardiol. 2007, 99, 1316–1320.
- Harms, V.; Reisman, M.; Fuller, C.J.; Spencer, M.P.; Olsen, J.V.; Krabill, K.A.; Gray, W.A.; Jesurum, J.T. Outcomes after transcatheter closure of patent foramen ovale in patients with paradoxical embolism. Am. J. Cardiol. 2007, 99, 1312–1315.
- Van den Branden, B.J.; Luermans, J.G.; Post, M.C.; Plokker, H.W.; Ten Berg, J.M.; Suttorp, M.J. The BioSTAR(r) device versus the CardioSEAL(r) device in patent foramen ovale closure: Comparison of mid-term efficacy and safety. EuroIntervention 2010, 6, 498–504.
- Baglini, R.; Baldari, D.; Amaducci, A.; D’Ancona, G. The new patent foramen ovale occluder FIGULLA in complex septal anatomy: A case series. Ther. Adv. Cardiovasc. Dis. 2013, 7, 21–26.
- Krizanic, F.; Sievert, H.; Pfeiffer, D.; Konorza, T.; Ferrari, M.; Figulla, H.R. Clinical evaluation of a novel occluder device (Occlutech) for percutaneous transcatheter closure of patent foramen ovale (PFO). Clin. Res. Cardiol. 2008, 97, 872–877.
- Ruygrok, P.N. The Coherex FlatStent: An advance in patent foramen ovale closure. Expert Rev. Med. Devices 2010, 7, 193–199.
- Pristipino, C.; Sievert, H.; D’Ascenzo, F.; Mas, J.L.; Meier, B.; Scacciatella, P.; Hildick-Smith, D.; Gaita, F.; Toni, D.; Kyrle, P.; et al. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur. Heart J. 2019, 40, 3182–3195.
- Tobis, J.M. Patent foramen ovale: What cardiologists and neurologists need to know. Catheter. Cardiovasc. Interv. 2019, 93, 1085–1086.
- Abaci, A.; Unlu, S.; Alsancak, Y.; Kaya, U.; Sezenoz, B. Short and long term complications of device closure of atrial septal defect and patent foramen ovale: Meta-analysis of 28,142 patients from 203 studies. Catheter. Cardiovasc. Interv. 2013, 82, 1123–1138.
- Lattanzi, S.; Brigo, F.; Cagnetti, C.; Di Napoli, M.; Silvestrini, M. Patent Foramen Ovale and Cryptogenic Stroke or Transient Ischemic Attack: To Close or Not to Close? A Systematic Review and Meta-Analysis. Cerebrovasc. Dis. 2018, 45, 193–203.
- Akobeng, A.K.; Abdelgadir, I.; Boudjemline, Y.; Hijazi, Z.M. Patent foramen ovale (PFO) closure versus medical therapy for prevention of recurrent stroke in patients with prior cryptogenic stroke: A systematic review and meta-analysis of randomized controlled trials. Catheter. Cardiovasc. Interv. 2018, 92, 165–173.
- Windecker, S.; Wahl, A.; Chatterjee, T.; Garachemani, A.; Eberli, F.R.; Seiler, C.; Meier, B. Percutaneous closure of patent foramen ovale in patients with paradoxical embolism: Long-term risk of recurrent thromboembolic events. Circulation 2000, 101, 893–898.
- Schwerzmann, M.; Windecker, S.; Wahl, A.; Nedeltchev, K.; Mattle, H.P.; Seiler, C.; Meier, B. Implantation of a second closure device in patients with residual shunt after percutaneous closure of patent foramen ovale. Catheter. Cardiovasc. Interv. 2004, 63, 490–495.
- Susuri, N.; Obeid, S.; Ulmi, M.; Siontis, G.; Wahl, A.; Windecker, S.; Nietlispach, F.; Meier, B.; Praz, F.; Njomeza, S.; et al. Second transcatheter closure for residual shunt following percutaneous closure of patent foramen ovale. EuroIntervention 2017, 13, 858–866.
- Elgendy, A.Y.; Elgendy, I.Y.; Mojadidi, M.K.; Mahmoud, A.N.; Barry, J.S.; Jneid, H.; Wayangankar, S.A.; Tobis, J.M.; Meier, B. New-onset atrial fibrillation following percutaneous patent foramen ovale closure: A systematic review and meta-analysis of randomised trials. EuroIntervention 2019, 14, 1788–1790.
- Oliva, L.; Huszti, E.; Hall, R.; Abrahamyan, L.; Horlick, E. Incidence of new-onset atrial fibrillation after transcatheter patent foramen ovale closure using 15 years of Ontario administrative health data. Heart Rhythm 2022.
- Hascoet, S.; Fraisse, A.; Elbaz, M. Successful percutaneous transcatheter patent foramen ovale closure through the right internal jugular vein using a steerable catheter. Catheter. Cardiovasc. Interv. 2013, 82, E598–E602.
- Carter, L.I.; Cavendish, J.J. Percutaneous closure of a patent foramen ovale via left axillary vein approach with the Amplatzer Cribriform septal occluder. J. Interv. Cardiol. 2008, 21, 28–31.
- Stehli, J.; Michail, M.; McGaw, D.; Harper, R. “Liver or Let Die”: Percutaneous PFO Closure Through Hepatic Vein Access. Heart Lung Circ. 2019, 28, e134–e136.
- Alibegovic, J.; Bonvini, R.; Sigwart, U.; Dorsaz, P.; Camenzind, E.; Verin, V. The role of the sizing balloon in selection of the patent foramen ovale closure device size. Exp. Clin. Cardiol. 2008, 13, 42–46.
- Meier, B. Pacman sign during device closure of the patent foramen ovale. Catheter. Cardiovasc. Interv. 2003, 60, 221–223.
- Mojadidi, M.K.; Bogush, N.; Caceres, J.D.; Msaouel, P.; Tobis, J.M. Diagnostic accuracy of transesophageal echocardiogram for the detection of patent foramen ovale: A meta-analysis. Echocardiography 2014, 31, 752–758.
- Rodrigues, A.C.; Picard, M.H.; Carbone, A.; Arruda, A.L.; Flores, T.; Klohn, J.; Furtado, M.; Lira-Filho, E.B.; Cerri, G.G.; Andrade, J.L. Importance of adequately performed Valsalva maneuver to detect patent foramen ovale during transesophageal echocardiography. J. Am. Soc. Echocaardiogr. 2013, 26, 1337–1343.
- Johansson, M.C.; Eriksson, P.; Guron, C.W.; Dellborg, M. Pitfalls in diagnosing PFO: Characteristics of false-negative contrast injections during transesophageal echocardiography in patients with patent foramen ovales. J. Am. Soc. Echocardiogr. 2010, 23, 1136–1142.
- Rana, B.S.; Thomas, M.R.; Calvert, P.A.; Monaghan, M.J.; Hildick-Smith, D. Echocardiographic evaluation of patent foramen ovale prior to device closure. JACC Cardiovasc. Imaging 2010, 3, 749–760.
- Davison, P.; Clift, P.F.; Steeds, R.P. The role of echocardiography in diagnosis, monitoring closure and post-procedural assessment of patent foramen ovale. Eur. J. Echocardiogr. 2010, 11, i27–i34.
- Turc, G.; Calvet, D.; Guérin, P.; Sroussi, M.; Chatellier, G.; Mas, J.; The CLOSE Investigators. Closure, Anticoagulation, or Antiplatelet Therapy for Cryptogenic Stroke With Patent Foramen Ovale: Systematic Review of Randomized Trials, Sequential Meta-Analysis, and New Insights From the CLOSE Study. J. Am. Heart Assoc. 2018, 7, e008356.
- Cabanes, L.; Coste, J.; Derumeaux, G.; Jeanrenaud, X.; Lamy, C.; Zuber, M.; Mas, J.-L. Interobserver and intraobserver variability in detection of patent foramen ovale and atrial septal aneurysm with transesophageal echocardiography. J. Am. Soc. Echocardiogr. 2002, 15, 441–446.
- Mas, J.-L.; Arquizan, C.; Lamy, C.; Zuber, M.; Cabanes, L.; Derumeaux, G.; Coste, J. Recurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm, or both. N. Engl. J. Med. 2001, 345, 1740–1746.
- Handke, M.; Harloff, A.; Olschewski, M.; Hetzel, A.; Geibel, A. Patent foramen ovale and cryptogenic stroke in older patients. N. Engl. J. Med. 2007, 357, 2262–2268.
- Schuchlenz, H.W.; Saurer, G.; Weihs, W.; Rehak, P. Persisting eustachian valve in adults: Relation to patent foramen ovale and cerebrovascular events. J. Am. Soc. Echocardiogr. 2004, 17, 231–233.
- Goel, S.S.; Tuzcu, E.M.; Shishehbor, M.H.; de Oliveira, E.I.; Borek, P.P.; Krasuski, R.A.; Rodriguez, L.L.; Kapadia, S.R. Morphology of the patent foramen ovale in asymptomatic versus symptomatic (stroke or transient ischemic attack) patients. Am. J. Cardiol. 2009, 103, 124–129.
- Vitarelli, A. Patent Foramen Ovale: Pivotal Role of Transesophageal Echocardiography in the Indications for Closure, Assessment of Varying Anatomies and Post-procedure Follow-up. Ultrasound Med. Biol. 2019, 45, 1882–1895.
- Schwerzmann, M.; Salehian, O. Hazards of percutaneous PFO closure. Eur. J. Echocardiogr. 2005, 6, 393–395.
- Yared, K.; Baggish, A.L.; Solis, J.; Durst, R.; Passeri, J.J.; Palacios, I.F.; Picard, M.H. Echocardiographic Assessment of Percutaneous Patent Foramen Ovale and Atrial Septal Defect Closure Complications. Circ. Cardiovasc. Imaging 2009, 2, 141–149.
- Krantz, S.B.; Lawton, J.S. Subacute endocarditis of an atrial septal closure device in a patient with a patent foramen ovale. Ann. Thorac. Surg. 2014, 98, 1821–1823.
- Bartel, T.; Konorza, T.; Arjumand, J.; Ebradlidze, T.; Eggebrecht, H.; Caspari, G.; Neudorf, U.; Erbel, R. Intracardiac echocardiography is superior to conventional monitoring for guiding device closure of interatrial communications. Circulation 2003, 107, 795–797.
- Ren, J.-F.; Marchlinski, F.E.; Callans, D.J.; Herrmann, H.C. Clinical use of AcuNav diagnostic ultrasound catheter imaging during left heart radiofrequency ablation and transcatheter closure procedures. J. Am. Soc. Echocardiogr. 2002, 15 Pt 2, 1301–1308.
- Han, K.-N.; Ma, X.-T.; Yang, S.-W.; Zhou, Y.-J. Intracardiac echocardiography in the diagnosis and closure of patent foramen ovale. J. Geriatr. Cardiol. 2021, 18, 697–701.
