Biliary atresia (BA) is a progressive fibro-obliterative process with a variable degree of inflammation involving the hepatobiliary system. Its consequences are incalculable for the patients, the affected families, relatives, and the healthcare system. Scientific communities have identified a rate of about 1 case per 10,000–20,000 live births, but the percentage may be higher, considering the late diagnoses. The etiology is heterogeneous. BA, which is considered in half of the causes leading to orthotopic liver transplantation, occurs in primates and non-primates. To consolidate any model, (1) more transport and cell membrane studies are needed to identify the exact mechanism of noxa-related hepatotoxicity; (2) an online platform may be key to share data from pilot projects and new techniques; and (3) the introduction of differentially expressed genes may be useful in investigating the liver metabolism to target the most intricate bilio-toxic effects of pharmaceutical drugs and toxins.
- biliary atresia
- liver
- congenital
- perinatal
- animal model
1. Introduction
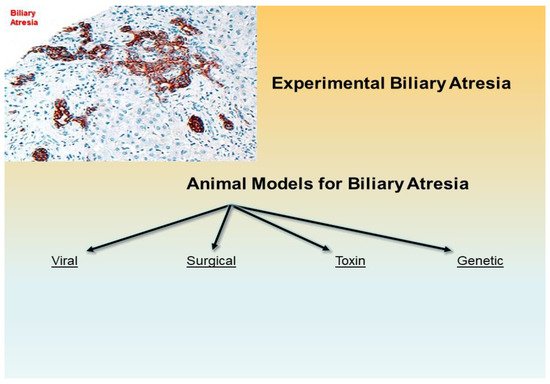
2. Experimental Animal Models Conundrum
3. Non-Human Primates and Non-Primates Occurrence of BA
4. Zebrafish
5. Lamprey
6. Rhesus Monkey
7. Transplantation Model
8. Virus-based Models
| Viral | Surgical | Toxin, Prenatal 1 | Toxin, Postnatal 2 | Genetic |
|---|---|---|---|---|
| gpCMV (Guinea pig): Infection-based => MNI, PC, Ch, F, BDP (Wang et al., 2011 [80]) |
Post natal BDL (Rabbit, lamb, rat, pig, monkey): Surgery-based => MNI, PC, Ch, F, ~ BDP (temp.) (Cameron & Oakley 1932 [81]) (Holder & Ashcraft 1966 [82]) (Morgan et al., 1966) (Spitz 1980 [83]) |
Phalloidin (Wistar rat): IP Administration => Canalicular Ch, ↑ Vol. peri-canalicular actin filaments (Hosoda et al., 1997 [84]) 1,4-phenylene-diisothio- cyanate (Wistar rat) Oral Administration => EHBDD, F, BDP (Ogawa et al., 1983 [85]) Monohydroxy bile acids (NZ white rabbit): IV Administration => BDO (in some offspring) (Jenner 1978 [86]) Biliatresone (BALB/c mouse): IP Administration => EHBD-A, MNI, F, BDP (Yang et al., 2020 [87]) |
Phorbol myristate acetate (Golden hamsters): GB infusion => Peribiliary PMN, F (Schmeling et al., 1991 [88]) |
inv mouse (OVE210 heterozygous invmutant mouse) IHBD-A (periportal), BDP, CBD patent (Shimadera et al., 2007 [89]) |
| RRV/HCR-3/WI-78 (BALB/c mouse): Infection -based => MNI, PC, Ch, ± F, -Atresia (Riepenhoff-Talty et al., 1993 [90]) |
Obliterative micro-Sx (Wistar rat): Microsurgery -based => F, BDP (zones 1 & 2) (Aller et al., 2004 [91][92]) |
Sox17 haploinsufficiency based mouse (C57BL/6 mouse) => Injury of the epithelial cells of the EHBDS, GB hypoplasia, BD stenosis/atresia (Uemura et al., 2013 [93]; Uemura et al., 2020 [54])) |
||
| Reo Virus 3 (mice): Infection-based => MNI, PC, Ch (Phillips et al., 1969 [94]) |
Transplantation (C57BL/6 and B1O.A mice): Graft-based (Fetal/perinatal renal subcapsular allografts in adult congenic mice) => Fibrosclerosis (Schreiber et al., 1992 [79]) |
Pkhd1-Nonobese diabetic (NOD) mouse (NOD.Abd3) => MNI, BDP (Huang et al., 2018 [95]) |
||
| Rotavirus Reassortant–Induced Model (RRRV: TR(VP2,VP4)) (Mouse): Infection-based => F, BDP (Mohanty et al., 2020 [96]) | Organ Culture (Embryonal liver culture) Cell culture-based (BD Induction in embryonic liver) (Petersen et al., 2001 [97]) |
This entry is adapted from the peer-reviewed paper 10.3390/ijms23147838
References
- Sergi, C.; Adam, S.; Kahl, P.; Otto, H.F. The remodeling of the primitive human biliary system. Early Hum. Dev. 2000, 58, 167–178.
- Amella, C.; Cappello, F.; Kahl, P.; Fritsch, H.; Lozanoff, S.; Sergi, C. Spatial and temporal dynamics of innervation during the development of fetal human pancreas. Neuroscience 2008, 154, 1477–1487.
- Sergi, C.M. The Paucity of Interlobular Bile Ducts. In Liver Diseases: A Multidisciplinary Textbook; Radu-Ionita, F., Pyrsopoulos, N.T., Jinga, M., Tintoiu, I.C., Sun, Z., Bontas, E., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 261–272.
- Dorn, L.; Menezes, L.F.; Mikuz, G.; Otto, H.F.; Onuchic, L.F.; Sergi, C. Immunohistochemical detection of polyductin and co-localization with liver progenitor cell markers during normal and abnormal development of the intrahepatic biliary system and in adult hepatobiliary carcinomas. J. Cell. Mol. Med. 2009, 13, 1279–1290.
- Sergi, C.; Kahl, P.; Otto, H.F. Contribution of apoptosis and apoptosis-related proteins to the malformation of the primitive intrahepatic biliary system in Meckel syndrome. Am. J. Pathol. 2000, 156, 1589–1598.
- Sergi, C.; Adam, S.; Kahl, P.; Otto, H.F. Study of the malformation of ductal plate of the liver in Meckel syndrome and review of other syndromes presenting with this anomaly. Pediatr. Dev. Pathol. 2000, 3, 568–583.
- Sergi, C.; Benstz, J.; Feist, D.; Nutzenadel, W.; Otto, H.F.; Hofmann, W.J. Bile duct to portal space ratio and ductal plate remnants in liver disease of infants aged less than 1 year. Pathology 2008, 40, 260–267.
- Russo, P.; Magee, J.C.; Anders, R.A.; Bove, K.E.; Chung, C.; Cummings, O.W.; Finegold, M.J.; Finn, L.S.; Kim, G.E.; Lovell, M.A.; et al. Key Histopathologic Features of Liver Biopsies That Distinguish Biliary Atresia from Other Causes of Infantile Cholestasis and Their Correlation with Outcome: A Multicenter Study. Am. J. Surg. Pathol. 2016, 40, 1601–1615.
- Sergi, C.M.; Gilmour, S. Biliary Atresia: A Complex Hepatobiliary Disease with Variable Gene Involvement, Diagnostic Procedures, and Prognosis. Diagnostics 2022, 12, 330.
- Sergi, C.M. Genetics of Biliary Atresia: A Work in Progress for a Disease with an Unavoidable Sequela into Liver Cirrhosis following Failure of Hepatic Portoenterostomy. In Liver Cirrhosis-Debates and Current Challenges; Tsoulfas, G., Ed.; IntechOpen: London, UK, 2019.
- Bove, K.E.; Thrasher, A.D.; Anders, R.; Chung, C.T.; Cummings, O.W.; Finegold, M.J.; Finn, L.; Ranganathan, S.; Kim, G.E.; Lovell, M.; et al. Inflammation, Active Fibroplasia, and End-stage Fibrosis in 172 Biliary Atresia Remnants Correlate Poorly with Age at Kasai Portoenterostomy, Visceral Heterotaxy, and Outcome. Am. J. Surg. Pathol. 2018, 42, 1625–1635.
- Sergi, C.M.; Chiu, B. Targeting NLRP3 inflammasome in an animal model for Coronavirus Disease 2019 (COVID-19) caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). J. Med. Virol. 2021, 93, 669–670.
- Boaru, S.G.; Borkham-Kamphorst, E.; Tihaa, L.; Haas, U.; Weiskirchen, R. Expression analysis of inflammasomes in experimental models of inflammatory and fibrotic liver disease. J. Inflamm. 2012, 9, 49.
- Longo, L.; Tonin Ferrari, J.; Rampelotto, P.H.; Hirata Dellavia, G.; Pasqualotto, A.C.P.O.; Thadeu Schmidt Cerski, C.; Reverbel da Silveira, T.; Uribe-Cruz, C.; Alvares-da-Silva, M.R. Gut Dysbiosis and Increased Intestinal Permeability Drive microRNAs, NLRP-3 Inflammasome and Liver Fibrosis in a Nutritional Model of Non-Alcoholic Steatohepatitis in Adult Male Sprague Dawley Rats. Clin. Exp. Gastroenterol. 2020, 13, 351–368.
- Berauer, J.P.; Mezina, A.I.; Okou, D.T.; Sabo, A.; Muzny, D.M.; Gibbs, R.A.; Hegde, M.R.; Chopra, P.; Cutler, D.J.; Perlmutter, D.H.; et al. Identification of PKD1L1 Gene Variants in Children with the Biliary Atresia Splenic Malformation Syndrome. Hepatology 2019, 70, 899–910.
- Nio, M.; Wada, M.; Sasaki, H.; Tanaka, H.; Watanabe, T. Long-term outcomes of biliary atresia with splenic malformation. J. Pediatr. Surg. 2015, 50, 2124–2127.
- Goel, A.; Chaudhari, S.; Sutar, J.; Bhonde, G.; Bhatnagar, S.; Patel, V.; Bhor, V.; Shah, I. Detection of Cytomegalovirus in Liver Tissue by Polymerase Chain Reaction in Infants with Neonatal Cholestasis. Pediatr. Infect. Dis. J. 2018, 37, 632–636.
- Zani, A.; Quaglia, A.; Hadzic, N.; Zuckerman, M.; Davenport, M. Cytomegalovirus-associated biliary atresia: An aetiological and prognostic subgroup. J. Pediatr. Surg. 2015, 50, 1739–1745.
- Brindley, S.M.; Lanham, A.M.; Karrer, F.M.; Tucker, R.M.; Fontenot, A.P.; Mack, C.L. Cytomegalovirus-specific T-cell reactivity in biliary atresia at the time of diagnosis is associated with deficits in regulatory T cells. Hepatology 2012, 55, 1130–1138.
- Domiati-Saad, R.; Dawson, D.B.; Margraf, L.R.; Finegold, M.J.; Weinberg, A.G.; Rogers, B.B. Cytomegalovirus and human herpesvirus 6, but not human papillomavirus, are present in neonatal giant cell hepatitis and extrahepatic biliary atresia. Pediatr. Dev. Pathol. 2000, 3, 367–373.
- Saito, T.; Terui, K.; Mitsunaga, T.; Nakata, M.; Ono, S.; Mise, N.; Yoshida, H. Evidence for viral infection as a causative factor of human biliary atresia. J. Pediatr. Surg. 2015, 50, 1398–1404.
- Saito, T.; Shinozaki, K.; Matsunaga, T.; Ogawa, T.; Etoh, T.; Muramatsu, T.; Kawamura, K.; Yoshida, H.; Ohnuma, N.; Shirasawa, H. Lack of evidence for reovirus infection in tissues from patients with biliary atresia and congenital dilatation of the bile duct. J. Hepatol. 2004, 40, 203–211.
- Glaser, J.H.; Morecki, R. Reovirus type 3 and neonatal cholestasis. Semin. Liver Dis. 1987, 7, 100–107.
- Hertel, P.M.; Estes, M.K. Rotavirus and biliary atresia: Can causation be proven? Curr. Opin. Gastroenterol. 2012, 28, 10–17.
- Mahjoub, F.; Shahsiah, R.; Ardalan, F.A.; Iravanloo, G.; Sani, M.N.; Zarei, A.; Monajemzadeh, M.; Farahmand, F.; Mamishi, S. Detection of Epstein Barr virus by chromogenic in situ hybridization in cases of extra-hepatic biliary atresia. Diagn. Pathol. 2008, 3, 19.
- Fjaer, R.B.; Bruu, A.L.; Nordbo, S.A. Extrahepatic bile duct atresia and viral involvement. Pediatr. Transplant. 2005, 9, 68–73.
- Muraji, T.; Ohtani, H.; Ieiri, S. Unique manifestations of biliary atresia provide new immunological insight into its etiopathogenesis. Pediatr. Surg. Int. 2017, 33, 1249–1253.
- Chen, G.; Xue, P.; Zheng, S.; Chen, L.; Ma, Y. A pathological scoring system in the diagnosis and judgment of prognosis of biliary atresia. J. Pediatr. Surg. 2015, 50, 2119–2123.
- Safwan, M.; Ramachandran, P.; Vij, M.; Shanmugam, N.; Rela, M. Impact of ductal plate malformation on survival with native liver in children with biliary atresia. Pediatr. Surg. Int. 2015, 31, 837–843.
- Czubkowski, P.; Cielecka-Kuszyk, J.; Rurarz, M.; Kaminska, D.; Markiewicz-Kijewska, M.; Pawlowska, J. The limited prognostic value of liver histology in children with biliary atresia. Ann. Hepatol. 2015, 14, 902–909.
- Mukhopadhyay, S.G.; Roy, P.; Chatterjee, U.; Datta, C.; Banerjee, M.; Banerjee, S.; Basu, A.K.; Ganguli, M. A histopathological study of liver and biliary remnants in the long-term survivors (>10 years) of cases of biliary atresia. Indian J. Pathol. Microbiol. 2014, 57, 380–385.
- Vukovic, J.; Grizelj, R.; Bojanic, K.; Coric, M.; Luetic, T.; Batinica, S.; Kujundzic-Tiljak, M.; Schroeder, D.R.; Sprung, J. Ductal plate malformation in patients with biliary atresia. Eur. J. Pediatr. 2012, 171, 1799–1804.
- Yamaguti, D.C.; Patricio, F.R. Morphometrical and immunohistochemical study of intrahepatic bile ducts in biliary atresia. Eur. J. Gastroenterol. Hepatol. 2011, 23, 759–765.
- Roy, P.; Chatterjee, U.; Ganguli, M.; Banerjee, S.; Chatterjee, S.K.; Basu, A.K. A histopathological study of liver and biliary remnants with clinical outcome in cases of extrahepatic biliary atresia. Indian J. Pathol. Microbiol. 2010, 53, 101–105.
- Nakanuma, Y.; Harada, K.; Sato, Y.; Ikeda, H. Recent progress in the etiopathogenesis of pediatric biliary disease, particularly Caroli’s disease with congenital hepatic fibrosis and biliary atresia. Histol. Histopathol. 2010, 25, 223–235.
- Campos-Sanchez, J.C.; Esteban, M.A. Review of inflammation in fish and value of the zebrafish model. J. Fish Dis. 2021, 44, 123–139.
- Kent, M.L.; Sanders, J.L.; Spagnoli, S.; Al-Samarrie, C.E.; Murray, K.N. Review of diseases and health management in zebrafish Danio rerio (Hamilton 1822) in research facilities. J. Fish Dis. 2020, 43, 637–650.
- Stevens, C.H.; Reed, B.T.; Hawkins, P. Enrichment for Laboratory Zebrafish-A Review of the Evidence and the Challenges. Animals 2021, 11, 698.
- Lorent, K.; Yeo, S.Y.; Oda, T.; Chandrasekharappa, S.; Chitnis, A.; Matthews, R.P.; Pack, M. Inhibition of Jagged-mediated Notch signaling disrupts zebrafish biliary development and generates multi-organ defects compatible with an Alagille syndrome phenocopy. Development 2004, 131, 5753–5766.
- Cui, S.; Eauclaire, S.F.; Matthews, R.P. Interferon-gamma directly mediates developmental biliary defects. Zebrafish 2013, 10, 177–183.
- Cui, S.; Erlichman, J.; Russo, P.; Haber, B.A.; Matthews, R.P. Intrahepatic biliary anomalies in a patient with Mowat-Wilson syndrome uncover a role for the zinc finger homeobox gene zfhx1b in vertebrate biliary development. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 339–344.
- Cui, S.; Capecci, L.M.; Matthews, R.P. Disruption of planar cell polarity activity leads to developmental biliary defects. Dev. Biol. 2011, 351, 229–241.
- Tian, L.; Ye, Z.; Kafka, K.; Stewart, D.; Anders, R.; Schwarz, K.B.; Jang, Y.Y. Biliary Atresia Relevant Human Induced Pluripotent Stem Cells Recapitulate Key Disease Features in a Dish. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 56–63.
- Tang, V.; Cofer, Z.C.; Cui, S.; Sapp, V.; Loomes, K.M.; Matthews, R.P. Loss of a Candidate Biliary Atresia Susceptibility Gene, add3a, Causes Biliary Developmental Defects in Zebrafish. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 524–530.
- Ke, J.; Zeng, S.; Mao, J.; Wang, J.; Lou, J.; Li, J.; Chen, X.; Liu, C.; Huang, L.M.; Wang, B.; et al. Common genetic variants of GPC1 gene reduce risk of biliary atresia in a Chinese population. J. Pediatr. Surg. 2016, 51, 1661–1664.
- Ningappa, M.; Min, J.; Higgs, B.W.; Ashokkumar, C.; Ranganathan, S.; Sindhi, R. Genome-wide association studies in biliary atresia. Wiley Interdiscip. Rev. Syst. Biol. Med. 2015, 7, 267–273.
- Smith, K. Biliary tract: GPC1 genetic risk further links Hedgehog signalling with pathogenesis of biliary atresia. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 127.
- Cui, S.; Leyva-Vega, M.; Tsai, E.A.; EauClaire, S.F.; Glessner, J.T.; Hakonarson, H.; Devoto, M.; Haber, B.A.; Spinner, N.B.; Matthews, R.P. Evidence from human and zebrafish that GPC1 is a biliary atresia susceptibility gene. Gastroenterology 2013, 144, 1107–1115.e1103.
- Filmus, J.; Capurro, M.; Rast, J. Glypicans. Genome Biol. 2008, 9, 224.
- Cheung, Y.; Wu, Z.; Garcia-Barcelo, M.M.; Tam, P.K.H.; Ma, A.C.H.; Lui, V.C.H. Deletion of interleukin enhancer binding factor 2 (ILF2) resulted in defective biliary development and bile flow blockage. J. Pediatr. Surg. 2021, 56, 352–359.
- Soini, T.; Pihlajoki, M.; Andersson, N.; Lohi, J.; Huppert, K.A.; Rudnick, D.A.; Huppert, S.S.; Wilson, D.B.; Pakarinen, M.P.; Heikinheimo, M. Transcription factor GATA6: A novel marker and putative inducer of ductal metaplasia in biliary atresia. Am. J. Physiol. Gastrointest. Liver Physiol. 2018, 314, G547–G558.
- Bai, M.R.; Niu, W.B.; Zhou, Y.; Gong, Y.M.; Lu, Y.J.; Yu, X.X.; Wei, Z.L.; Wu, W.; Song, H.L.; Yu, W.W.; et al. Association of common variation in ADD3 and GPC1 with biliary atresia susceptibility. Aging 2020, 12, 7163–7182.
- Ningappa, M.; So, J.; Glessner, J.; Ashokkumar, C.; Ranganathan, S.; Min, J.; Higgs, B.W.; Sun, Q.; Haberman, K.; Schmitt, L.; et al. The Role of ARF6 in Biliary Atresia. PLoS ONE 2015, 10, e0138381.
- Uemura, M.; Higashi, M.; Pattarapanawan, M.; Takami, S.; Ichikawa, N.; Higashiyama, H.; Furukawa, T.; Fujishiro, J.; Fukumura, Y.; Yao, T.; et al. Gallbladder wall abnormality in biliary atresia of mouse Sox17 (+/-) neonates and human infants. Dis. Models Mech. 2020, 13, dmm042119.
- Pattarapanawan, M.; Uemura, M.; Miyazaki, N.; Takami, S.; Tomiyasu, H.; Tsunekawa, N.; Hirate, Y.; Fujishiro, J.; Kurohmaru, M.; Kanai-Azuma, M.; et al. Anatomical and histological characteristics of the hepatobiliary system in adult Sox17 heterozygote mice. Anat. Rec. 2020, 303, 3096–3107.
- Higashiyama, H.; Ozawa, A.; Sumitomo, H.; Uemura, M.; Fujino, K.; Igarashi, H.; Imaimatsu, K.; Tsunekawa, N.; Hirate, Y.; Kurohmaru, M.; et al. Embryonic cholecystitis and defective gallbladder contraction in the Sox17-haploinsufficient mouse model of biliary atresia. Development 2017, 144, 1906–1917.
- Yang, Y.; Jin, Z.; Dong, R.; Zheng, C.; Huang, Y.; Zheng, Y.; Shen, Z.; Chen, G.; Luo, X.; Zheng, S. MicroRNA-29b/142-5p contribute to the pathogenesis of biliary atresia by regulating the IFN-gamma gene. Cell Death Dis. 2018, 9, 545.
- Dong, R.; Zhao, R.; Zheng, S. Changes in epigenetic regulation of CD4+ T lymphocytesin biliary atresia. Pediatr. Res. 2011, 70, 555–559.
- Zhu, Y.G.; Li, J.; Pang, Y.; Li, Q.W. Lamprey: An important animal model of evolution and disease research. Yi Chuan 2020, 42, 847–857.
- York, J.R.; McCauley, D.W. Functional genetic analysis in a jawless vertebrate, the sea lamprey: Insights into the developmental evolution of early vertebrates. J. Exp. Biol. 2020, 223, jeb206433.
- Xu, Y.; Zhu, S.W.; Li, Q.W. Lamprey: A model for vertebrate evolutionary research. Zool. Res. 2016, 37, 263–269.
- Kuraku, S. Palaeophylogenomics of the vertebrate ancestor--impact of hidden paralogy on hagfish and lamprey gene phylogeny. Integr. Comp. Biol. 2010, 50, 124–129.
- Osorio, J.; Retaux, S. The lamprey in evolutionary studies. Dev. Genes Evol. 2008, 218, 221–235.
- Davenport, M. Biliary atresia: From Australia to the zebrafish. J. Pediatr. Surg. 2016, 51, 200–205.
- Chung-Davidson, Y.W.; Yeh, C.Y.; Li, W. The Sea Lamprey as an Etiological Model for Biliary Atresia. Biomed Res. Int. 2015, 2015, 832943.
- Youson, J.H. Biliary atresia in lampreys. Adv. Vet. Sci. Comp. Med. 1993, 37, 197–255.
- Raveenthiran, V. Long-Term Survival of Biliary Atresia without any Surgery: Lessons Learnt from Lamprey. J. Neonatal Surg. 2014, 3, 19.
- Chung-Davidson, Y.W.; Davidson, P.J.; Scott, A.M.; Walaszczyk, E.J.; Brant, C.O.; Buchinger, T.; Johnson, N.S.; Li, W. A new clarification method to visualize biliary degeneration during liver metamorphosis in Sea Lamprey (Petromyzon marinus). J. Vis. Exp. 2014, 88, 51648.
- Suchy, F.J. Biliary atresia in sea lampreys. What can it tell us about the disorder in human infants? Hepatology 2013, 57, 2114–2116.
- Cai, S.Y.; Lionarons, D.A.; Hagey, L.; Soroka, C.J.; Mennone, A.; Boyer, J.L. Adult sea lamprey tolerates biliary atresia by altering bile salt composition and renal excretion. Hepatology 2013, 57, 2418–2426.
- Yeh, C.Y.; Chung-Davidson, Y.W.; Wang, H.; Li, K.; Li, W. Intestinal synthesis and secretion of bile salts as an adaptation to developmental biliary atresia in the sea lamprey. Proc. Natl. Acad. Sci. USA 2012, 109, 11419–11424.
- Boomer, L.A.; Bellister, S.A.; Stephenson, L.L.; Hillyard, S.D.; Khoury, J.D.; Youson, J.H.; Gosche, J.R. Cholangiocyte apoptosis is an early event during induced metamorphosis in the sea lamprey, Petromyzon marinus L. J. Pediatr. Surg. 2010, 45, 114–120.
- Savina, M.V.; Emel’yanova, L.V.; Korotkov, S.M.; Brailovskaya, I.V.; Nadeev, A.D. Bioenergetics of mitochondria of the liver with biliary atresia during prolonged starvation. Dokl. Biochem. Biophys. 2009, 425, 80–83.
- Youson, J.H.; Sidon, E.W. Lamprey biliary atresia: First model system for the human condition? Experientia 1978, 34, 1084–1086.
- Chung-Davidson, Y.W.; Yeh, C.Y.; Bussy, U.; Li, K.; Davidson, P.J.; Nanlohy, K.G.; Brown, C.T.; Whyard, S.; Li, W. Hsp90 and hepatobiliary transformation during sea lamprey metamorphosis. BMC Dev. Biol. 2015, 15, 47.
- Zhao, R.; Dong, R.; Yang, Y.; Wang, Y.; Ma, J.; Wang, J.; Li, H.; Zheng, S. MicroRNA-155 modulates bile duct inflammation by targeting the suppressor of cytokine signaling 1 in biliary atresia. Pediatr. Res. 2017, 82, 1007–1016.
- Cornelius, C.E.; Rosenberg, D.P. Neonatal biliary atresia. Am. J. Pathol. 1985, 118, 168–171.
- Szavay, P.O.; Leonhardt, J.; Czech-Schmidt, G.; Petersen, C. The role of reovirus type 3 infection in an established murine model for biliary atresia. Eur. J. Pediatr. Surg. 2002, 12, 248–250.
- Schreiber, R.A.; Kleinman, R.E.; Barksdale, E.M., Jr.; Maganaro, T.F.; Donahoe, P.K. Rejection of murine congenic bile ducts: A model for immune-mediated bile duct disease. Gastroenterology 1992, 102, 924–930.
- Wang, W.; Zheng, S.; Shong, Z.; Zhao, R. Development of a guinea pig model of perinatal cytomegalovirus-induced hepatobiliary injury. Fetal Pediatr. Pathol. 2011, 30, 301–311.
- Cameron, G.R.; Oakley, C.L. Ligation of the common bile duct. J. Pathol. Bacteriol. 1932, 35, 769–798.
- Holder, T.M.; Ashcraft, K.W. Production of experimental biliary atresia by ligation of the common bile duct in the fetus. Surg. Forum 1966, 17, 356–357.
- Spitz, L. Ligation of the common bile duct in the fetal lamb: An experimental model for the study of biliary atresia. Pediatr. Res. 1980, 14, 740–748.
- Hosoda, Y.; Miyano, T.; Fujimoto, T. Assay of gamma-glutamyl transpeptidase activity in amniotic fluid offers a possible prenatal diagnosis of biliary atresia in the rat model. Prenat. Diagn. 1997, 17, 9–12.
- Ogawa, T.; Suruga, K.; Kojima, Y.; Kitahara, T.; Kuwabara, N. Experimental study of the pathogenesis of infantile obstructive cholangiopathy and its clinical evaluation. J Pediatr Surg. 1983, 18, 131–135.
- Jenner, R.E. New perspectives on biliary atresia. Ann. R. Coll. Surg. Engl. 1978, 60, 367–374.
- Yang, Y.; Wang, J.; Zhan, Y.; Chen, G.; Shen, Z.; Zheng, S.; Dong, R. The synthetic toxin biliatresone causes biliary atresia in mice. Lab. Investig. 2020, 100, 1425–1435.
- Schmeling, D.J.; Oldham, K.T.; Guice, K.S.; Kunkel, R.G.; Johnson, K.J. Experimental obliterative cholangitis. A model for the study of biliary atresia. Ann. Surg. 1991, 213, 350–355.
- Shimadera, S.; Iwai, N.; Deguchi, E.; Kimura, O.; Fumino, S.; Yokoyama, T. The inv mouse as an experimental model of biliary atresia. J. Pediatr. Surg. 2007, 42, 1555–1560.
- Riepenhoff-Talty, M.; Schaekel, K.; Clark, H.F.; Mueller, W.; Uhnoo, I.; Rossi, T.; Fisher, J.; Ogra, P.L. Group A rotaviruses produce extrahepatic biliary obstruction in orally inoculated newborn mice. Pediatr. Res. 1993, 33, 394–399.
- Aller, M.A.; Nava, M.P.; Arias, J.L.; Durán, M.; Prieto, I.; Llamas, M.A.; Arias, J. Microsurgical extrahepatic cholestasis in the rat: A long-term study. J Invest Surg. 2004, 17, 99–104.
- Aller, M.A.; Duran, M.; Ortega, L.; Arias, J.L.; Nava, M.P.; Prieto, I.; Arias, J. Comparative study of macro- and microsurgical extrahepatic cholestasis in the rat. Microsurgery 2004, 24, 442–447.
- Uemura, M.; Ozawa, A.; Nagata, T.; Kurasawa, K.; Tsunekawa, N.; Nobuhisa, I.; Taga, T.; Hara, K.; Kudo, A.; Kawakami, H.; et al. Sox17 haploinsufficiency results in perinatal biliary atresia and hepatitis in C57BL/6 background mice. Development 2013, 140, 639–648.
- Phillips, P.A.; Keast, D.; Papadimitriou, J.M.; Walters, M.N.; Stanley, N.F. Chronic obstructive jaundice induced by Reovirus type 3 in weanling mice. Pathology 1969, 1, 193–203.
- Huang, W.; Rainbow, D.B.; Wu, Y.; Adams, D.; Shivakumar, P.; Kottyan, L.; Karns, R.; Aronow, B.; Bezerra, J.; Gershwin, M.E.; et al. A Novel Pkhd1 Mutation Interacts with the Nonobese Diabetic Genetic Background To Cause Autoimmune Cholangitis. J. Immunol. 2018, 200, 147–162.
- Mohanty, S.K.; Lobeck, I.; Donnelly, B.; Dupree, P.; Walther, A.; Mowery, S.; Coots, A.; Bondoc, A.; Sheridan, R.M.; Poling, H.M.; et al. Rotavirus Reassortant-Induced Murine Model of Liver Fibrosis Parallels Human Biliary Atresia. Hepatology 2020, 71, 1316–1330.
- Petersen, M.; Drews, U.; Schweizer, P. Induction of bile ducts in embryonic liver by mesenchyme: A new perspective for the treatment of biliary atresia? Eur. J. Pediatr. Surg. 2001, 11, 382–390.
