Itching can decrease quality of life and exacerbate skin symptoms due to scratching. Itching not only contributes to disease progression but also triggers complications such as skin infections and eye symptoms. Therefore, controlling itching is very important in therapeutic management. In addition to the well-known histamine, IL-31, IL-4 and IL-13 have recently been reported as factors that induce itching. Histamine-dependent itching is literally itching caused by histamine. It acts on the “sensory nerve” that perceives pain and itching, and the stimulus is transmitted to the brain as itching, as well as to the nerve endings, causing the release of neurotransmitters called neuropeptides. This neuropeptide then stimulates mast cells to secrete histamine and other substances.
1. Histamine as an Itch-Inducing Substance
Controlling itching is important in therapeutic management because it not only contributes to disease progression by decreasing quality of life and exacerbating skin symptoms due to scratching but also triggers complications such as skin infections and ocular symptoms. In addition to the well-known histamine, IL-31, IL-4 and IL-13 have recently been reported as factors that induce itching. It has been shown that IL-31 induces acute itch by acting on IL-31RA in sensory nerves, while IL-4 and IL-13 induce chronic itch by acting on sensory nerves and lowering the response threshold to pruritogenic factors
[1]. Factors other than histamine can cause itching, but at this time, the extent to which these factors are involved in each disease is unknown. Although the degree of involvement may vary from person to person, antihistamines are still widely used as treatment for itching and are often effective, suggesting that histamine is involved to a greater or lesser extent in itchy diseases. This review discusses antihistamines in terms of ligands and receptors.
2. Actions of Histamine on Skin and Central Nervous System
The main points of action of histamine are in the skin and brain. Because histamine has a different point of action in the skin and in the brain, histamine’s action in each is also different. In skin, histamine is primarily released from mast cells and then binds to histamine H1 receptors (“H1 receptors”) on microvascular endothelial cells. The result is itching along with wheals and erythema, such as urticaria. Histamine in the brain, on the other hand, is released from activated neurons (histamine neurons). Free histamine acts on H1 receptors in the cerebrum, cerebellum, and spinal cord as a neurotransmitter, and it induces the following major physiological functions: maintenance of arousal level, increase in spontaneous locomotion, enhancement of memory and learning functions, suppression of feeding behavior, and suppression of seizures.
3. Histamine-Mediated Skin Diseases
Urticaria is a skin disease in which histamine is directly involved. Atopic dermatitis, like urticaria, also presents itching, but reports on the association with histamine are conflicting. Such peripheral itching is divided into histamine-dependent and histamine-independent itching, depending on clinical sensitivity to antihistamines. Although the ratio of each in each disease has not been clarified, because histamine-dependent itching is thought to be involved in urticaria, atopic dermatitis, and eczema, in which itching is observed, antihistamines are relatively commonly used for these skin diseases in Japan.
Histamine-dependent itching is literally itching caused by histamine. It acts on the “sensory nerve” that perceives pain and itching, and the stimulus is transmitted to the brain as itching, as well as to the nerve endings, causing the release of neurotransmitters called neuropeptides. This neuropeptide then stimulates mast cells to secrete histamine and other substances. Stimuli such as “itching and scratching” stimulate the sensory nerves in sensitive skin, causing the release of neuropeptides, which in turn stimulate the secretion of the itching substance histamine. It is believed that this phenomenon causes the itching to spread more and more.
In itchy skin, inflammation is often present, and several inflammatory cytokines have been reported to bind directly to receptors on neurons and trigger itch signals. IL-31 is produced primarily by Th2 cells
[2]. Receptors for IL-31 are also expressed on neurons and are thought to be mediators that play a central role in the itching that occurs especially in patients with atopic dermatitis and pruritus.
Receptors for IL-4 and IL-13, also cytokines produced by Th2 cells, are also expressed on nerve endings and directly cause itching
[1]. IL-31 has been implicated in the acute phase of inflammation, while IL-4 and IL-13 are involved in the chronic phase of inflammatory itching. Suppression of IL-4 and IL-13 directly affects not only the suppression of inflammation, but also the suppression of itching.
In addition, IL-17, which plays an important role in the pathogenesis of psoriasis, is also known to be a mediator that can directly activate the itch nerve
[3]. Thymic stromal lymphopoietin (TSLP), produced by epidermal keratinocytes, is another known mediator of itch
[4]. PAR2, a receptor on the plasma membrane that recognizes proteases and is expressed on epidermal keratinocytes and neurons, is also implicated in itching. Various foreign antigens such as pollen and mite antigens have protease activity, and when PAR2 is activated, Th2-type inflammation is induced. Substance P is a neuropeptide secreted from nerve terminals. Activation of histamine receptors and PAR2 on neurons results in secondary secretion of Substance P from neurons. The receptor for Substance P (NK1-R) is expressed on epidermal keratinocytes, vascular endothelium, mast cells, and even neurons, and it is known to amplify dermatitis and itching. Therefore, it is thought to act as an enhancer rather than an initiator of itch signals.
MRGPR is associated with histamine-independent itching in atopic dermatitis and other conditions. MRGPR is a receptor on the plasma membrane and is selectively expressed on mast cells and neurons. Chloroquine is known as a ligand, but the details of the endogenous ligand are unknown. Mast cells express both IgE receptors and MRGPRs, but the nature of the itch caused when each is activated is different
[5]. When IgE receptors are activated, histamine is secreted by mast cells, causing a fast-rising, short-duration itch. On the other hand, when MRGPRB2 on mast cells is activated, tryptase and other enzymes are secreted, which in turn activate MRGPRA3 and MRGPRD on neurons, causing itching. Itching at this time is considered to be a slow-rising, persistent itch. Thus, itching is caused by various substances other than histamine, and histamine and its receptors are discussed below.
4. Regulation of the Function and Distribution of Histamine Receptors as G Protein-Coupled Receptors—Desensitization Therapy—
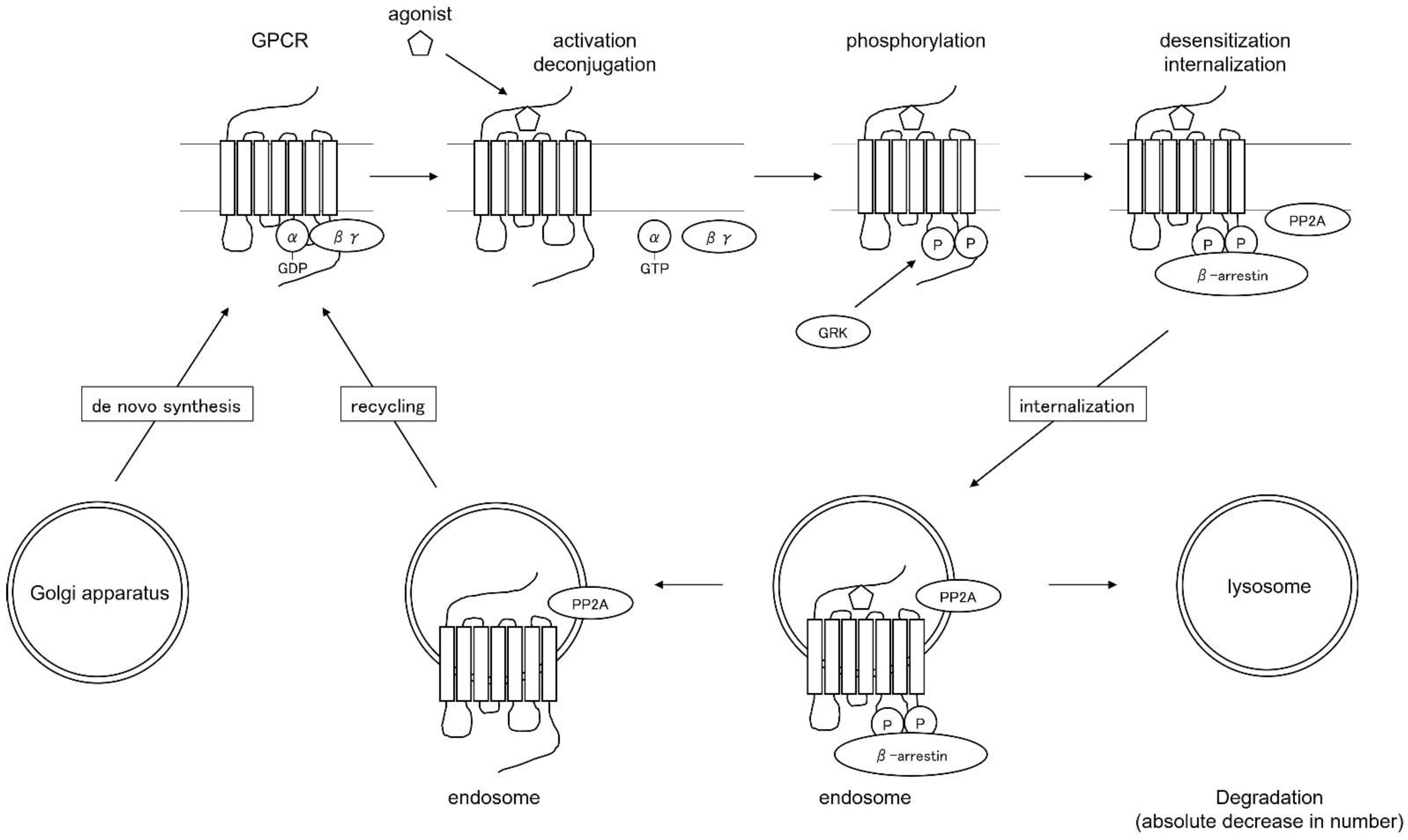
The H1 receptor is a Gq protein-coupled receptor with a seven-transmembrane structure. G protein-coupled receptors (GPCRs) are activated when stimulated by agonists, which activate G proteins for signaling and at the same time serve as substrates for G-protein-coupled receptor kinase (GRK), which is phosphorylated. The phosphorylated receptor binds to β-arrestin and the receptor and G proteins are no longer able to bind (deconjugation). β-arrestins are coated with clathrin and transport receptors into the cell. Receptors that have migrated into the cell are resensitized and recycled to the plasma membrane as normal receptors. Some of the receptors transported into the cell are degraded by lysosomes, resulting in a decrease in the absolute number of receptors (Figure 1). The function and distribution of GPCRs are regulated by these mechanisms.
Figure 1. Regulation of function and distribution of G-protein-coupled receptors.
There are three major types of changes in the number and function of H1 receptors on the cell surface: changes in “absolute number” due to the balance between new synthesis and degradation, changes in “distribution” due to intracellular translocation and recycling to the plasma membrane, and changes in “function” due to changes in receptor ligand affinity and deconjugation with G proteins. Functional changes are caused by changes in receptor ligand affinity and deconjugation with G proteins. This mechanism of desensitization has been applied to drugs for multiple sclerosis and LH-RH-like drugs. It has been reported that H1 receptor expression is elevated in diseases associated with itching, such as atopic dermatitis and urticaria
[6], suggesting the possibility of therapeutic application to these diseases.
This entry is adapted from the peer-reviewed paper 10.3390/ijms23126579