Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Orthopedics
Avascular necrosis (AVN) of the femoral head is caused by disruption of the blood supply to the proximal femur. The alterations in the blood supply may occur following a traumatic event or result from a non-traumatic cause. Femoral neck fracture and hip dislocation and associated surgical procedures, corticosteroid therapy, and alcohol abuse frequently lead to AVN development.
- implants
- avascular necrosis
- femoral head
1. Introduction
Avascular necrosis (AVN) of the femoral head is a type of aseptic osteonecrosis, which is caused disruption of the blood supply to the proximal femur, which results in osteocyte death. AVN may occur due to ischemia developing on a traumatic or non-traumatic background [1,2]. The most common etiological factors include treatment with corticosteroids, fractures, dislocation of the hip joint, and alcohol abuse [3]. It typically affects physically active people aged between 20 and 40 years. Between 10,000 and 20,000 new cases of AVN of the femoral head are diagnosed in the United States (US) each year [
2. Etiology of AVN
2.1. Non-Traumatic Causes of AVN
The most common non-traumatic causes are corticosteroid treatment and alcohol abuse. Corticosteroids alter adipocytes’ differentiation, increasing the size and number of adipocytes. This process leads to the intracellular accumulation of lipids. As a result of increased pressure inside the bone cells, vascular endothelial cells become damaged, leading to local coagulopathy, vascular thrombosis, and ischemia. A dose-dependent effect was observed in a meta-analysis performed by Mont et al. The incidence of AVN was 6.7% with a corticosteroid dose of >2 g prednisone equivalent per day. Every additional 10 mg/day increased the rate of AVN by 3.6%. Nonetheless, not all patients receiving corticosteroids develop AVN. It is proposed that other factors, including genetic polymorphisms and concomitant diseases, increase individuals’ vulnerability [7,10,11]. For instance, in patients treated with corticosteroids due to systemic lupus erythematosus, a higher risk of AVN was observed than in patients with other medical diagnoses [6]. Other drugs, such as antiretrovirals, are also linked to increased AVN risk [12,13].
Alcohol abuse is reported by 20–30% of the patients with AVN. The potential mechanism of induction of AVN is unknown. Alcohol may provoke osteocyte death through several pathways, e.g., by increasing intracellular deposition of triglycerides, which leads to pyknosis of osteocytes similarly to corticosteroids, and by decreasing osteogenesis through promoting stromal cell differentiation into adipocytes [14].
Other conditions related to the AVN include Gaucher’s disease. Patients who developed anemia in the course of that disease have increased chances of AVN development by 60% when compared with the non-anemic group [13]. In sickle cell hemoglobinopathy, ischemia is provoked by restrictions in local blood flow by abnormally adherent blood cells [15]. In the case of hematopoietic cell transplantation, concomitant immunosuppressive treatment with corticosteroids and graft versus host disease was proposed to induce microcirculation alterations and, consequently, AVN [16]. A less common cause is Legg–Calvé–Perthes disease, an idiopathic AVN in the pediatric population [17].
2.2. Traumatic Factors
Posttraumatic AVN occurs when the blood supply to the femoral head is disrupted due to a fracture or dislocation of the femoral head. In most cases, AVN is related to fractures in the sub-capital region of the femoral neck. Injury in this region disrupts the anastomosis between the lateral epiphyseal vessels, limiting the blood supply to the femoral head [4,18].
In the systematic review performed by Ghayoumi et al., the overall incidence of avascular necrosis in patients with displaced femoral neck fractures was 17.3% [19]. According to Slobogean et al., displaced fractures were associated with a statistically higher incidence of AVN than undisplaced fractures (14.7% vs. 6.4%) [20].
2.3. Avascular Necrosis following Stabilization of the Fractured Femoral Neck
Femoral neck fixation allows recovery of vascular supply to the femoral head and restores its functionality, thus avoiding joint replacement surgery. For internal fixation in non-displaced cases, most surgeons choose hip preserving techniques such as a dynamic hip screw (DHS) or multiple cannulated screws (MCS) [21]. DHS is a more invasive technique than MCS but achieves better anchorage with less rotation and cut-out [21].
Figure 1 and Figure 2 present AVN of the femoral head developed after surgical stabilization of an intertrochanteric fracture of the femoral bone.

Figure 1. Avascular necrosis of right femoral head following stabilization of intertrochanteric fracture. (A) Posteroanterior view of the fracture; posteroanterior (B) view after 12 weeks of procedure; (C) view at a follow-up visit 20 weeks after the procedure, prominent necrosis of right femoral head; R—right.
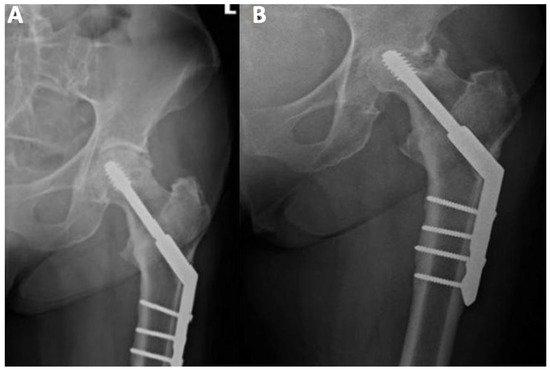
Figure 2. Posteroanterior view of internal fixation of left femoral neck fracture using the dynamic hip screw. (A) Posteroanterior view directly after the procedure; (B) posteroanterior view during control 15 weeks after the procedure, prominent necrosis of left femoral head.
2.4. Dynamic Hip Screw (DHS) Technique and the Risk of AVN
Many authors have described cases of AVN after a femoral neck fracture surgery. DHS was shown to be associated with a high risk of osteonecrosis. Some studies have demonstrated that it might be even higher than that with other hip-preserving techniques, such as cancellous screws. Schwartzman et al. observed AVN in 16% of 96 patients with sub-capital neck fractures treated with DHS, though not all other papers show a statistically significant difference between these two methods [21,22,23,24]. On the contrary, in a large randomized controlled trial, AVN was more common in patients treated with DHS than in those treated with cancellous screws (9% vs. 5%, HR 1.91, 1.06–3.44; p = 0.03) [25].
Using large implants for fixation (such as those used in DHS) of femoral neck fracture is associated with a disruption in blood supply to the femoral head. This was confirmed using bone scintigraphy in 104 patients with femoral neck fractures, indicating reduced vascularity in patients treated with DHS compared with those treated with cancellous screws (35% vs. 11%, p < 0.01) [26]. Other potential complications of surgical treatment of femoral head fractures include delayed union, nonunion, infection, and angular or rotational malalignment [27].
Some studies have shown promising results regarding AVN risk reduction following the modified DHS technique. Elgeidi et al. described the outcomes of using DHS and autogenous fibular strut graft for fixation of a femoral neck fracture with posterior comminution. Interestingly, the authors did not observe any case of AVN. This could be attributed to the fact that fibular graft has an osteoconductive and osteoinductive potential and acts as a biologically compatible implant allowing revascularization [28].
2.5. AVN following Fixation with Cannulated Screws
Some studies demonstrate that the use of cannulated screws may also be linked to a high rate of complications. Duckworth et al. observed a 32% rate of complications after fixation of intracapsular fracture of the femoral head by cannulated screws. The second most common reason for failure was AVN, observed in 11.5% of the patients with a mean time to treatment failure of 19.8 months [29]. Other authors reported similar rates of AVN after cannulated fixation [30,31,32].
Modification of the cannulated screw method was developed to decrease the odds of AVN. Li et al. compared the occurrence of AVN after fixation of the femoral neck using three cannulated screws with and without deep circumflex iliac artery bone grafting (DCIABG). The rates of AVN were significantly lower in the group of patients treated with DCIABG compared to classic fixation (9.7% vs. 26.8%, p < 0.001) [33].
New hip-preserving techniques under investigation
Preliminary results of using Targon femoral neck (TFN) implants are promising in terms of reduction in ANV risk following femoral neck fracture fixation. The TFN implant is a locking plate system with telescoping sliding screws. Depending on the fracture type, internal fixation of femoral neck fracture with a TFN implant may lower the risk of AVN to as low as 3% [34,35,36]. Though data on the incidence of AVN after short intramedullary femoral nailing are limited, it seems to be promising in terms of AVN risk reduction. Chen et al. reported a 1.2% incidence of AVN among patients with unstable, intertrochanteric fractures treated with Asian Pacific gamma-nail [37].
2.6. Other Factors to Consider When Assessing the Risk of AVN Following Femoral Neck Fixation
Estimation of the risk of AVN may help in optimizing treatment plans in patients after femoral neck fracture. Factors such as type of fracture, Garden classification, preoperative traction, and the time interval between injury and surgery seem to be crucial in terms of the risk of AVN development [38]. Displaced fractures in elderly patients are usually unsuitable for hip preserving techniques and require hemiarthroplasty or THA; the risk of AVN is higher in displaced fractures than in undisplaced ones [39]. In another study by Loizou et al., most patients with hip fractures underwent internal fixation using three cannulated screws. The overall incidence of AVN was 6.6%, and the complication was more common in patients with displaced fractures than in those with undisplaced ones (9.5% vs. 4.0%, p = 0.0004). Of note, contrary to other reports, AVN was more common in women than in men regardless of the type of fracture (displaced vs. undisplaced) [40].
The time between surgery and injury appears to be crucial in assessing the risk of bone ischemia—a time interval between injury and surgery greater than 24 h was associated with an increased risk [39]. This was confirmed by Migliorini et al. In that systematic review, data from 6112 patients with osteonecrosis of the femoral head who underwent hip-preserving procedures were retrieved to identify prognostic factors for failure of initial surgical management and conversion to total hip arthroplasties (THAs). Longer duration of symptoms and higher VAS score before treatment resulted in reduced time to treatment failure. In addition, a poor hip function was related to an increased rate of treatment failure and conversion to joint replacement. Female gender was a protective factor against treatment failure and conversion to THA and increased time to that procedure. Other analyzed factors such as body mass index, the cause of AVN, and time from surgery to full weight-bearing did not significantly affect the treatment outcome [41].
2.7. AVN Following Hip Fracture in the Pediatric Population
AVN cases in children require separate discussion. In the pediatric population, the incidence of AVN may be higher than that in adults. In the study of Bali et al. 36 children with a mean age of 10 years sustained femoral neck fractures. Patients were treated conservatively, with open reduction and internal fixation or closed reduction and internal fixation. Of 13 cases treated conservatively, 8 had lost reduction and required surgical intervention. The rate of AVN was 19.4%, which is higher than the average rate observed in adults. A plausible explanation is that the adult hip has intraosseous blood vessels that supply the femoral head, and these blood vessels are absent in children as they cannot cross the physis, which remains open at a young age. Therefore, the blood supply in children may be disrupted more easily after a hip fracture. In the literature, the rates of AVN following acute trauma in children ranged from 17% to 47% [42].
3. Clinical and Radiographic Examination of the AVN
The diagnosis of AVN is mainly based on both clinical and radiographic findings. Typical clinical presentation includes increasing pain, stiffness, and crepitus, usually proceeded by a period of minimal symptoms. During the physical examination, patients typically complain of a limited range of motion at the hip and the presence of pain, particularly with a forced internal rotation [4]. Early identification of the disease provides better outcomes. Many imaging techniques were found helpful in detecting bone necrosis signs, including X-ray, magnetic resonance imaging (MRI), computed tomography (CT), and radionuclide examinations. Imaging evaluation of AVN should begin with radiography, a non-expensive and widely available technique. Classic radiography may show subchondral radiolucency, called the “crescent sign”, indicating subchondral collapse [9]. CT and X-ray are less sensitive than MRI and show the necrotic changes during later stages of AVN. Nonetheless, signs of AVN are often apparent enough not to warrant additional radiologic evaluation [43]. Typical findings on MRI in a patient with an AVN are pictured in Figure 3.
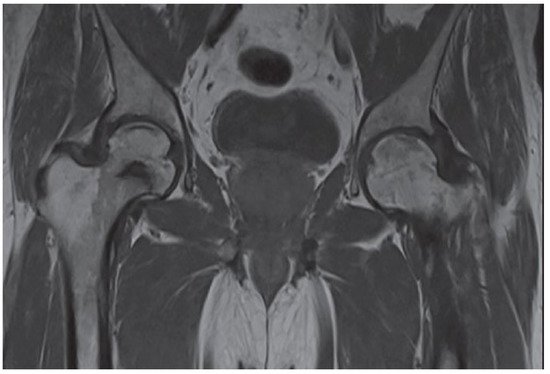
Figure 3. The posteroanterior view shows a right (R) AVN of the femoral head (T1-weighted).
MRI is the gold standard for osteonecrosis diagnosis and allows differentiating AVN from other diagnoses that may mimic it, such as bone bruises or transitioned osteopenia [1,9]. MRI allows for early AVN diagnosis and may help identify patients at risk of femoral head fracture. Identification of bone marrow edema in the proximal femur and joint effusion are critical prognostic factors [3]. T1-weighted images show a limited subchondral linear-shaped low signal intensity, while T2 demonstrates a double-line sign [44]. However, MRI cannot be used after fracture fixation with metallic implants, limiting its utility, especially in patients who develop bone ischemia following surgical procedure [18].
Fan et al. compared single-photon emission computerized tomography and computerized tomography (SPECT/CT) to determine the risk of bone necrosis in patients following femoral neck fracture. The study results revealed that SPECT is most useful for determining the prognosis of AVN in patients aged >58 years and with displaced fractures [45]. Diagnostic methods based on nuclear medicine, such as positron emission tomography (PET) or technetium bone scans, may also be used to detect the early stages of AVN and help predict the disease progression [1,46].
Although the patient’s medical history, clinical features, and radiographic examination might indicate AVN, the clinician should include other clinical entities in the differential diagnosis.
The Steinberg University of Pennsylvania system is the classification most used in AVN. This system includes six stages with the assessment of involvement within each stage. The classification allows for distinguishing between mild (<15% radiographic involvement of the femoral head), moderate (15–30% involvement of the femoral head), and severe (>30% involvement of the femoral head) stages [9,47].
This entry is adapted from the peer-reviewed paper 10.3390/ijerph19127348
This entry is offline, you can click here to edit this entry!
